Black specks in stool can be alarming, but understanding the potential causes is crucial for appropriate action. This exploration delves into various factors, from dietary indiscretions to more serious medical conditions, to help you decipher the meaning behind these dark specks. We’ll investigate the physiological mechanisms, common diagnostic procedures, and available treatment options.
From mild digestive issues to more severe health concerns, this comprehensive guide provides a structured approach to understanding the causes, symptoms, and necessary steps to take when encountering black specks in your stool. We’ll navigate the complexities of dietary factors and medical conditions, equipping you with the knowledge to make informed decisions.
Possible Causes of Black Specks in Stool
Black specks in stool, a seemingly minor issue, can sometimes signal underlying medical conditions. Understanding the potential causes, ranging from benign to severe, is crucial for prompt diagnosis and treatment. Proper evaluation by a healthcare professional is essential for accurate assessment and personalized management.
Potential Medical Conditions
Various medical conditions can lead to the appearance of black specks in stool. These conditions vary in severity, from mild digestive issues to more serious gastrointestinal or systemic problems. Careful consideration of associated symptoms and medical history is vital for accurate diagnosis.
Mild Conditions
Iron-rich foods and medications are common causes of black stool that is not indicative of a serious condition. Consuming foods rich in iron, such as red meat and leafy greens, can sometimes lead to dark-colored stools. Certain medications, particularly iron supplements, can also result in temporary discoloration. These occurrences are usually benign and resolve on their own or with dietary adjustments.
Moderate Conditions
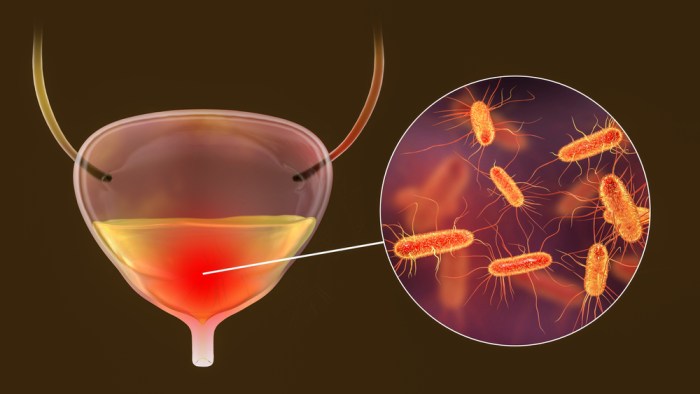
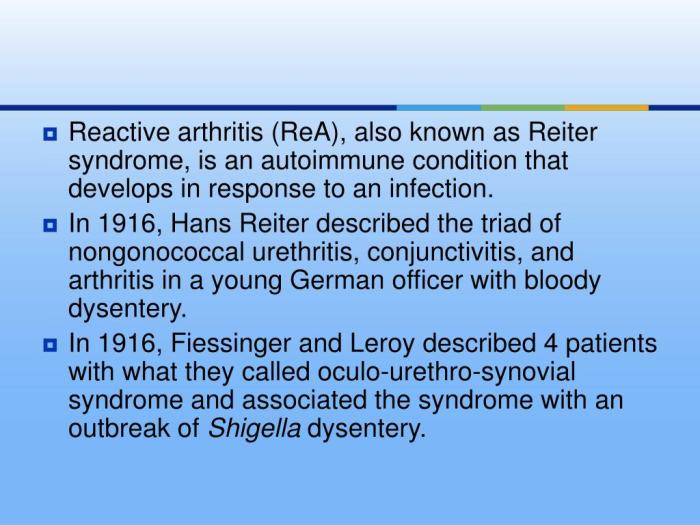
Upper gastrointestinal bleeding, a more concerning cause of black stool, involves bleeding in the esophagus, stomach, or duodenum. This bleeding can result from various factors, including ulcers, gastritis, or esophageal varices. Patients often experience symptoms like nausea, vomiting, and dizziness. The blood in the upper digestive tract breaks down into smaller particles, creating the characteristic black discoloration in stool.
This is due to the chemical process of digestion, converting the hemoglobin in the blood to a substance called melena.
Severe Conditions
Conditions such as esophageal varices, tumors, or severe gastritis can cause significant bleeding in the upper digestive tract. Symptoms may include severe abdominal pain, vomiting blood (hematemesis), and signs of shock, such as rapid pulse and low blood pressure. The mechanism is the same as with moderate cases, with a large amount of blood in the upper GI tract resulting in the formation of black, tarry stool.
| Condition | Symptoms | Mechanism | Severity |
|---|---|---|---|
| Iron-rich foods/medications | Dark-colored stool only | Digestion of iron-rich substances | Mild |
| Upper GI bleeding (ulcers, gastritis) | Nausea, vomiting, dizziness, black, tarry stool (melena) | Blood in upper digestive tract digested to form melena | Moderate |
| Esophageal varices, tumors, severe gastritis | Severe abdominal pain, vomiting blood (hematemesis), shock | Significant blood loss in upper GI tract, resulting in formation of melena | Severe |
Dietary Factors
Sometimes, the culprit behind those dark specks in your stool isn’t a serious medical condition, but rather what you’ve been eating. Certain foods can temporarily alter the color of your stool, leading to a surprising appearance. Understanding these dietary influences can help distinguish between a cause for concern and a simple dietary adjustment.Dietary factors can significantly impact stool color, ranging from a subtle change to a noticeable darkness.
This often occurs due to the presence of pigments or compounds in foods that are processed differently within the digestive system. The intensity of the darkening effect depends on individual factors, including the quantity of the food consumed, the overall diet, and individual digestive processes. In some cases, the temporary discoloration might be accompanied by other symptoms like bloating or discomfort.
Hey everyone, ever noticed black specks in your stool? It can be a little alarming, right? Sometimes, these specks could be related to something completely different, like issues with digestion. But, it’s also important to consider that similar symptoms, like a clear sticky discharge, can have various causes, and when to get treatment for these is really important.
For more insight into the potential causes of clear sticky discharge and when it’s time to seek medical attention, check out this helpful resource: clear sticky discharge causes and when to get treatment. Ultimately, if you’re concerned about black specks in your stool, it’s always best to consult a doctor for a proper diagnosis and personalized advice.
Foods Causing Black Stool
A variety of foods can lead to black stool, primarily due to their iron content or other substances that react with stomach acids. These pigments can then be excreted through the stool. The duration of this effect depends on how quickly the body processes the food.
- Iron-Rich Foods: Foods like red meat, spinach, and iron-fortified cereals are excellent sources of iron. Iron supplements can also contribute to black stool. The dark color results from the iron reacting with stomach acid and being passed through the digestive tract.
- Foods Containing Certain Pigments: Some foods, though not as common as iron-rich ones, contain pigments that can affect stool color. These pigments can sometimes bind with other substances in the digestive system to cause a dark coloration.
- Foods High in Melanin: Melanin, the pigment responsible for skin color, is also present in certain foods, such as dark berries. Though not a direct cause of black stool, the presence of melanin in food can contribute to the overall color.
Duration of Effect
The time it takes for dietary factors to affect stool color varies. It typically ranges from a few hours to a couple of days, depending on the food, the amount consumed, and individual digestion. A meal rich in iron, for example, might lead to dark stool within a few hours to a day. Conversely, a more gradual effect might be seen with foods containing pigments.
| Food | Approximate Duration of Effect |
|---|---|
| Red meat | Few hours to 1-2 days |
| Iron-fortified cereals | Few hours to 1-2 days |
| Spinach | Few hours to 1-2 days |
| Iron supplements | Few hours to 1-2 days |
| Dark berries | Few hours to 2-3 days |
Comparison to Medical Conditions
Distinguishing between dietary and medical causes of black stool can be challenging. While certain foods can lead to temporary discoloration, persistent black stool or black stool accompanied by other symptoms, such as abdominal pain, vomiting, or dizziness, could indicate a more serious medical issue. It’s crucial to consult a healthcare professional if the dark stool persists or is accompanied by other concerning symptoms.
A medical evaluation is essential to rule out conditions such as bleeding in the upper gastrointestinal tract. The appearance of black stool due to dietary factors typically involves a more uniform darkening of the stool, unlike the possible tarry or sticky consistency that might be associated with bleeding.
Diagnostic Considerations

Pinpointing the cause of black specks in stool requires a systematic approach. These dark particles, while sometimes benign, can also signal underlying health issues. A thorough evaluation, combining patient history, physical examination, and appropriate diagnostic tests, is crucial to accurately determine the root cause.
Initial Evaluation and History Taking
Gathering a comprehensive medical history is the first step. This includes details about dietary habits, recent medications, travel history, family history of digestive disorders, and any other relevant symptoms. The doctor will inquire about the frequency, duration, and consistency of the black stool, as well as any accompanying symptoms like abdominal pain, nausea, or vomiting. This initial assessment helps narrow down the potential causes and guide the subsequent diagnostic procedures.
Physical Examination
A physical examination is essential to evaluate the patient’s overall health status. This may include checking for signs of anemia, such as paleness, or signs of bleeding disorders. The doctor will also examine the abdomen for tenderness, masses, or other abnormalities. This step provides valuable clues about the potential cause of the black specks, helping to direct further diagnostic investigations.
Endoscopy Procedures
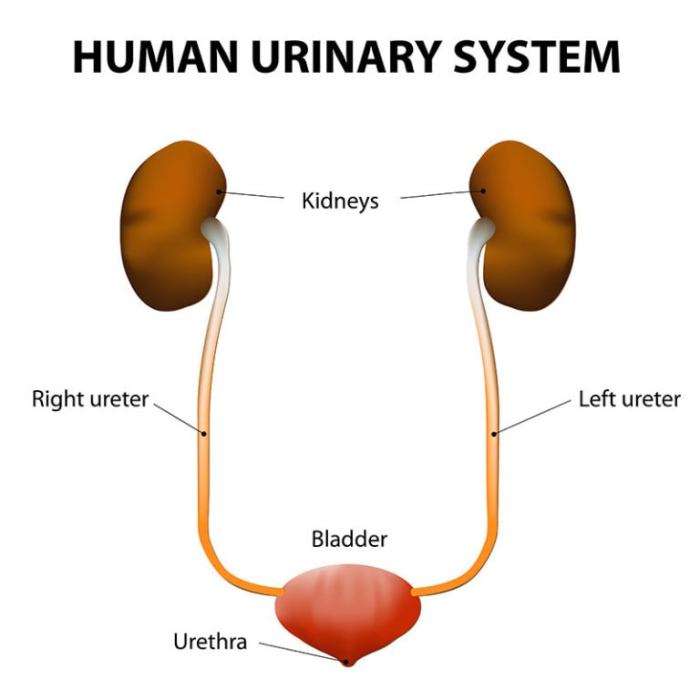
Endoscopy procedures are often used to visualize the upper digestive tract, particularly the esophagus, stomach, and duodenum. Esophagogastroduodenoscopy (EGD) is a common procedure. In EGD, a flexible tube with a camera is inserted through the mouth and into the digestive tract. This allows the doctor to directly view the lining of the digestive tract and identify any abnormalities, ulcers, or bleeding sources.
A biopsy may be taken to obtain tissue samples for further analysis if needed. A key point is that this procedure is more invasive than other tests.
Blood Tests
Blood tests are routinely performed to assess various aspects of the patient’s health. These tests may include complete blood counts (CBC) to evaluate red blood cell levels, looking for signs of anemia. Other tests might be conducted to check for clotting factors, liver function, and other relevant parameters to rule out bleeding disorders or other underlying conditions. The blood test results are instrumental in evaluating the overall health status and potential bleeding issues.
Imaging Studies
Imaging studies, such as X-rays and CT scans, are often used to visualize the digestive system. X-rays can help detect foreign bodies, tumors, or structural abnormalities. CT scans provide a more detailed view of the internal organs, allowing for a more comprehensive evaluation of the digestive tract and potentially identifying sources of bleeding. These procedures help assess the extent of any abnormalities and the underlying cause of the black stool.
Comparison of Diagnostic Procedures
| Diagnostic Procedure | Accuracy | Invasiveness | Cost |
|---|---|---|---|
| History Taking | Moderate | Low | Low |
| Physical Examination | Moderate | Low | Low |
| Endoscopy (EGD) | High | Moderate | Moderate to High |
| Blood Tests | Moderate to High | Low | Low to Moderate |
| Imaging Studies (X-ray, CT) | Moderate to High | Moderate | Moderate to High |
Treatment Options
Dealing with black specks in your stool can be concerning, but understanding the potential causes and appropriate treatments is crucial. The treatment approach will vary significantly depending on the underlying reason for the discoloration. Proper diagnosis is paramount to ensure the chosen treatment effectively addresses the root cause and prevents potential complications.Effective treatment for black stools often involves addressing the specific cause, whether it’s dietary, medication-related, or a more serious condition.
This necessitates a thorough evaluation by a healthcare professional to pinpoint the source of the issue. Self-treating can be risky and may mask or worsen the underlying problem.
Dietary Modifications
Dietary changes can be effective for some causes of black stools. If the cause is related to food consumption, adjusting your diet can resolve the problem. For instance, if iron-rich foods are consumed excessively or improperly combined with other ingredients, dietary modifications can be an effective solution. Iron-rich foods, while essential, need to be balanced with other nutrients to prevent digestive issues.
- Reducing or eliminating iron-rich foods for a period of time, and reintroducing them gradually, allows your body to adjust and potentially resolve the issue.
- Increasing fiber intake through fruits, vegetables, and whole grains can improve digestion and promote regular bowel movements.
- Avoiding foods known to cause digestive distress, such as spicy or greasy foods, can alleviate symptoms.
Medication Adjustments
Certain medications can cause black stools. If the black stools are related to medication, working with a doctor to adjust the dosage or switch to an alternative medication is important. For instance, if a patient taking iron supplements experiences black stools, a lower dose or a different form of iron may resolve the problem.
- Adjusting the dosage of medications that may be contributing to the black stools.
- Switching to alternative medications if possible.
- Following prescribed medication instructions carefully.
Medical Interventions
For more serious causes of black stools, such as bleeding in the upper gastrointestinal tract, medical interventions might be necessary. This could range from endoscopy to identify the source of the bleeding to more invasive procedures if necessary. The approach will depend on the severity and location of the bleeding.
- Endoscopy: A procedure where a thin, flexible tube with a camera is inserted into the esophagus, stomach, and duodenum to visualize the lining and identify any bleeding sources. Expected outcomes are identifying the cause and potentially treating it during the procedure.
- Angiography: A procedure using X-rays to visualize blood vessels and treat bleeding in the gastrointestinal tract. Outcomes may include stopping bleeding and treating the underlying cause, with potential complications including allergic reactions or infections.
- Surgical interventions: For severe cases of bleeding ulcers or tumors, surgery may be necessary. Expected outcomes include resolving the source of bleeding, but risks are significant, including potential complications during and after surgery.
Comparison of Treatment Options, Black specks in stool
The best treatment option depends on the underlying cause. Dietary modifications are generally the safest and least invasive option for simple cases. Medication adjustments require close collaboration with a physician to avoid adverse effects. Medical interventions are reserved for more severe conditions requiring specialized procedures.
| Treatment Option | Potential Benefits | Potential Risks | Typical Duration |
|---|---|---|---|
| Dietary Modifications | Relatively safe, inexpensive, and can resolve the issue in simple cases. | May not be effective for all causes, requires patient adherence. | Variable, often weeks to months. |
| Medication Adjustments | Can resolve the issue related to medications. | Potential side effects from altered medications, requires careful monitoring by a physician. | Variable, dependent on the medication and its effects. |
| Medical Interventions | Effective for severe cases, addresses the underlying cause. | Higher risk of complications, more invasive procedures. | Variable, from days to weeks, dependent on the severity and type of procedure. |
Preventive Measures
Preventing black specks in stool often hinges on proactive dietary and lifestyle choices. By understanding the potential causes and adopting healthy habits, you can significantly reduce the risk of experiencing this unsettling issue. Early detection through regular checkups plays a crucial role in addressing underlying problems before they escalate.Maintaining a healthy digestive system is a multifaceted process. A balanced diet, combined with mindful lifestyle choices, can significantly impact the overall health of your digestive tract.
Understanding these connections is key to preventative measures.
Dietary Habits for Digestive Health
A balanced diet is paramount for maintaining a healthy digestive system. Focus on incorporating a variety of nutrient-rich foods, including fruits, vegetables, whole grains, and lean proteins. These foods provide essential vitamins, minerals, and fiber, which are crucial for proper digestion.
Hey everyone, Have you ever noticed black specks in your stool? It can be a bit concerning, but sometimes it’s just harmless. However, if it’s persistent, it’s definitely worth checking in with a doctor. Interestingly, donating blood can actually have some surprising benefits for your overall health, such as boosting your iron levels. Consider looking into the benefits of donating blood if you’re healthy enough.
Either way, if you’re experiencing black specks in your stool, consulting a healthcare professional is key to getting to the bottom of it and ensuring you’re taking care of your health.
- Fiber-Rich Foods: Increasing fiber intake promotes regular bowel movements and helps prevent constipation, a factor that can contribute to the appearance of black specks. Examples include whole grains, fruits (like berries and apples), and vegetables (like broccoli and spinach). Adequate fiber consumption can help maintain regularity.
- Hydration: Drinking plenty of water is essential for proper digestion and bowel movements. Water helps soften stool and aids in its passage through the digestive tract. Dehydration can lead to constipation and potentially contribute to the appearance of black specks.
- Limit Processed Foods and Red Meat: Reducing consumption of processed foods, especially those high in saturated fats and unhealthy additives, can be beneficial for overall digestive health. Similarly, excessive consumption of red meat may also impact digestion. Moderation in these areas can help prevent digestive issues.
Lifestyle Choices for Digestive Well-being
Beyond diet, lifestyle choices play a significant role in maintaining a healthy digestive system. Stress management techniques and regular exercise are crucial components of a holistic approach.
- Stress Management: Chronic stress can negatively impact the digestive system, potentially leading to irregularities. Incorporating stress-reducing activities, such as yoga, meditation, or spending time in nature, can promote digestive health.
- Regular Exercise: Physical activity is beneficial for overall health and can aid in promoting regular bowel movements. A moderate exercise routine can help maintain a healthy weight and support digestive function.
- Adequate Sleep: Getting sufficient sleep is crucial for overall health, including digestive health. Lack of sleep can disrupt the body’s natural processes, potentially impacting digestion.
Importance of Regular Checkups and Screenings
Regular medical checkups and screenings are essential for early detection of potential issues. These checkups allow for early identification of underlying conditions that might be causing black specks in stool.
- Routine Colonoscopies: For individuals with risk factors or a family history of digestive disorders, routine colonoscopies are crucial for early detection of polyps or other abnormalities that could be associated with black specks in stool. These procedures can help identify potential issues before they become serious.
- Regular Blood Tests: Routine blood tests can reveal potential underlying conditions that might be contributing to digestive problems, such as anemia or other medical issues. These tests provide crucial diagnostic information.
Situations Requiring Increased Preventative Measures
Certain individuals may require heightened attention to preventative measures due to specific circumstances or risk factors.
- Individuals with a Family History of Digestive Disorders: Those with a family history of conditions like inflammatory bowel disease (IBD) or colorectal cancer should prioritize regular checkups and screenings to detect any potential issues early.
- Individuals with Existing Digestive Issues: If you have a history of digestive problems, maintaining a healthy diet and lifestyle is particularly important. This includes managing stress, staying hydrated, and following a balanced eating plan.
Additional Information
Persistent black specks in your stool, while often benign, warrant attention. Ignoring these specks could potentially mask underlying conditions requiring prompt medical intervention. Understanding when to seek immediate help and where to find reliable resources is crucial for managing this concern effectively.Seeking medical advice for persistent black specks in stool is important to rule out any serious underlying conditions.
A healthcare professional can evaluate your specific situation, considering your medical history, lifestyle, and dietary habits. This personalized assessment is essential for an accurate diagnosis and appropriate treatment plan.
Importance of Seeking Medical Advice
A healthcare provider can thoroughly assess the cause of black specks in your stool. They can perform necessary diagnostic tests and determine if the specks are indicative of a serious condition. Ignoring persistent black specks could lead to delays in diagnosis and treatment of a more serious condition, potentially impacting your health negatively.
When to Seek Immediate Medical Attention
Certain situations demand immediate medical attention. Seek emergency care if you experience black specks in your stool alongside other symptoms like severe abdominal pain, vomiting, dizziness, or difficulty breathing. These symptoms could signal a significant issue requiring prompt intervention. Additionally, if the black specks appear with other signs of internal bleeding such as unusually dark or tarry stools, or if you experience significant blood loss, seek immediate medical attention.
Those pesky black specks in your stool can be a real worry. While they might seem alarming, they’re often nothing to panic about. Sometimes, though, they could be a sign of something more serious, like a digestive issue. Knowing what a seizure looks like can also be helpful in understanding potential causes for unusual symptoms. For a better understanding of how a seizure might manifest, check out this informative article on what does a seizure look like.
If you’re concerned about black specks in your stool, it’s always best to consult a doctor for a proper diagnosis.
Reliable Resources for Further Information
For further information and support, consult reputable medical organizations like the Mayo Clinic, the Cleveland Clinic, and the National Institutes of Health (NIH). These organizations offer reliable and comprehensive information about various health concerns. Additionally, your primary care physician or a gastroenterologist can provide tailored advice based on your individual circumstances.
Key Takeaways: When to Seek Immediate Medical Attention
| Symptom(s) | Action |
|---|---|
| Black specks in stool accompanied by severe abdominal pain, vomiting, dizziness, or difficulty breathing | Seek immediate medical attention. |
| Black specks in stool accompanied by unusually dark or tarry stools, or significant blood loss | Seek immediate medical attention. |
Illustrative Examples: Black Specks In Stool
Understanding the causes of black specks in stool requires examining various scenarios. These examples highlight the diverse factors contributing to this symptom, ranging from dietary choices to underlying medical conditions. A detailed understanding of these scenarios can aid in proper diagnosis and treatment.
Dietary Factor Example: Iron-Rich Foods
A patient experiencing black stool following the consumption of a significant amount of iron-rich foods, such as red meat or iron supplements, is a common dietary-related example. The iron in these foods reacts with stomach acid, leading to the appearance of black, tarry stools. This is a harmless, temporary effect and usually resolves as the patient reduces or eliminates the offending foods from their diet.
Medical Condition Example: Gastrointestinal Bleeding
Gastrointestinal (GI) bleeding, stemming from ulcers, esophageal varices, or inflammatory bowel disease, can manifest as black specks or tarry stool. The blood, broken down in the digestive tract, imparts the dark color to the stool. The severity of the bleeding can vary greatly, impacting the appearance and consistency of the stool. In severe cases, the stool may appear very dark and resemble tar.
Patient Presentation and Diagnostic Process
A patient presenting with black specks in stool should undergo a comprehensive evaluation. This involves a detailed medical history, focusing on recent dietary changes, medications, and any prior GI issues. A physical examination follows, assessing for signs of anemia, abdominal tenderness, or other relevant symptoms. Laboratory tests, including stool tests to check for blood, and blood tests to evaluate hemoglobin levels, will aid in identifying the underlying cause.
Further diagnostic procedures, such as endoscopy or colonoscopy, may be necessary to visualize the source of the bleeding.
Importance of Detailed Medical History and Physical Examination
A detailed medical history is crucial in determining the cause of black stool. This includes inquiries about recent dietary changes, medication use, and past medical conditions, including previous gastrointestinal issues. The patient’s medical history provides a context for understanding the potential causes and helps differentiate between benign and potentially serious conditions. The physical examination plays a vital role in assessing the patient’s overall health status, identifying any signs of anemia or abdominal tenderness, and supporting the information gathered from the medical history.
These combined efforts provide a strong foundation for a comprehensive diagnostic approach.
Ultimate Conclusion
In conclusion, black specks in stool can be a sign of something minor or something requiring immediate attention. This guide has explored the potential causes, diagnostic procedures, and treatment options. Remember, seeking medical advice is paramount if you experience persistent black specks. A detailed discussion with your doctor is essential for a proper diagnosis and personalized treatment plan.