Surgical margin in skin cancer is crucial for successful treatment. Understanding the various types of margins, the factors influencing their determination, and the surgical techniques used to achieve them is vital in preventing recurrence. This guide delves into the intricacies of this critical aspect of skin cancer management, from defining clear, close, and positive margins to examining the role of tumor characteristics and histological assessment.
Different skin cancer types and individual patient factors can impact margin selection. We’ll explore how tumor depth, location, and morphology affect the size and shape of the necessary surgical margin. The importance of precise tissue dissection and the various surgical approaches, such as Mohs micrographic surgery and shave excision, will be highlighted. Finally, we’ll examine the critical role of histopathological evaluation and the management of positive margins.
Definition and Significance of Surgical Margin in Skin Cancer
Surgical margins are crucial in skin cancer surgery. They represent the tissue surrounding the cancerous area that is removed along with the tumor. Properly assessing and managing margins directly impacts the likelihood of successful treatment and long-term patient outcomes. A key goal is to remove all cancerous cells to prevent recurrence.Understanding surgical margins is vital for both patients and healthcare professionals.
An inadequate margin can lead to the remaining cancer cells, and thus a high chance of the cancer returning at the same site or spreading to other parts of the body. Conversely, a correctly executed surgical margin minimizes the risk of recurrence.
Surgical Margin Definition
Surgical margin in skin cancer refers to the tissue surrounding the tumor that is excised during surgery. The aim is to remove not only the visible tumor but also a rim of healthy tissue to ensure complete eradication of cancerous cells. This healthy tissue surrounding the tumor is the surgical margin. Precisely defining the margin size and its characteristics is critical to minimize the risk of residual cancer cells and ensure the optimal outcome for the patient.
Surgical margins in skin cancer are crucial for complete removal, ensuring no cancerous cells remain. Learning to manage the discomfort of a new medical device like a CPAP machine can be challenging, but resources like how to get used to cpap offer practical advice. Ultimately, precise surgical margins are key to successful treatment and preventing recurrence.
Importance of Adequate Surgical Margin
Adequate surgical margins are essential for preventing recurrence. By removing a sufficient amount of tissue, surgeons can effectively remove all cancerous cells, minimizing the risk of the cancer growing back in the same area. A complete removal significantly improves the chances of successful treatment and long-term survival. Failure to achieve adequate margins can lead to a higher likelihood of recurrence.
Relationship Between Margin Size and Recurrence Risk
The size of the surgical margin directly correlates with the risk of recurrence. Smaller margins, such as those that are close to the tumor’s edge, are associated with a higher risk of recurrence compared to larger, clear margins. This is because a smaller margin may contain residual cancer cells that weren’t removed. Studies have shown that clear margins are associated with significantly lower recurrence rates compared to close margins.
Surgical margins in skin cancer are crucial for complete removal, minimizing the risk of recurrence. While focusing on those margins, it’s also important to consider potential side effects of medications like the one used to treat autoimmune conditions. For example, if you’re taking Plaquenil, you should be aware of potential eye issues, and regularly check for any problems.
Knowing about potential side effects like those associated with Plaquenil and your eyes, plaquenil and your eyes , is a vital component of your overall health management strategy, and this is equally as important as ensuring your surgical margins are appropriately wide.
Different Types of Surgical Margins
Different types of surgical margins reflect the extent of cancer removal and thus the potential risk of recurrence. These are commonly categorized as follows:
| Margin Type | Description | Recurrence Risk | Clinical Implications |
|---|---|---|---|
| Clear Margin | A clear margin indicates that the surgical removal has encompassed a sufficient amount of healthy tissue surrounding the tumor. All visible cancer cells are completely removed, and there’s no residual tumor cells in the margin tissue. | Low | Indicates successful removal and favorable prognosis. |
| Close Margin | A close margin means that the surgical removal has come very close to the tumor’s edge, but some healthy tissue is not adequately removed. The margin is within a predetermined acceptable distance from the tumor. | Moderate | Requires careful consideration for further treatment or additional surgery to achieve a clear margin, if indicated. |
| Positive Margin | A positive margin means that cancer cells are found within the surgical margin. This indicates incomplete removal of the tumor and requires further treatment to ensure complete eradication of cancerous cells. | High | Indicates the need for additional surgery or other treatment options, such as radiation therapy, to achieve a clear margin. |
Factors Influencing Surgical Margin Determination
Surgical margin determination in skin cancer surgery is a critical aspect of ensuring complete removal of the cancerous tissue and minimizing the risk of recurrence. Precisely defining the extent of the surgical margin is crucial for successful treatment and patient outcomes. The decision is multifaceted, taking into account various factors that influence the size and shape of the excision.
Tumor Depth
Tumor depth significantly impacts the size of the surgical margin. Deeper infiltrating tumors necessitate larger margins to ensure complete removal of all malignant cells. This is because the risk of residual tumor cells increases with depth. For example, a tumor that penetrates the dermis and extends into the subcutaneous fat may require a larger margin than a superficial tumor confined to the epidermis.
The depth of invasion is often categorized into different stages, with each stage correlating to different margin recommendations.
Surgical margins in skin cancer removal are crucial for complete excision. While the focus is on removing all cancerous cells, it’s interesting to consider if healthy lifestyle choices, like diet, play a role in the healing process. A recent study on the effects of diet, for example, investigated whether eating apples reduces aging, potentially impacting skin regeneration.
does eating apples reduce aging Ultimately, precise surgical margins are still the gold standard for ensuring the best outcomes in skin cancer treatment.
Tumor Location
The location of the tumor on the body also plays a role in margin selection. Margins near sensitive anatomical structures like joints, eyes, or the nose may require adjustments to avoid compromising functional integrity. For example, a tumor on the eyelid would necessitate a smaller margin to minimize the risk of functional impairment. Conversely, a tumor located in an area with ample surrounding tissue may allow for a larger margin.
Tumor Morphology
Tumor morphology, encompassing factors such as size, shape, and ulceration, directly influences margin determination. Larger tumors generally require larger margins to account for the greater potential for extensive tumor spread. Irregularly shaped tumors or those with ulceration may indicate a more aggressive behavior, potentially necessitating wider margins to ensure complete removal. For instance, a large, ulcerated tumor in a high-risk location will warrant a more extensive surgical excision.
Histological Assessment
Histological assessment of the surgical specimen plays a crucial role in confirming margin adequacy. A pathologist meticulously examines the specimen for the presence of tumor cells at the margin. A clear margin free of tumor cells confirms complete removal and a low risk of recurrence. If tumor cells are present at the margin, further surgery may be required to achieve an adequate margin.
The pathologist’s report provides definitive confirmation of the presence or absence of tumor cells at the margins.
| Factor | Description | Impact on Margin |
|---|---|---|
| Tumor Depth | The distance the tumor extends into the underlying tissue layers. | Deeper tumors require larger margins. |
| Tumor Location | The site of the tumor on the body. | Margins near sensitive areas may be adjusted. |
| Tumor Morphology | Size, shape, and ulceration of the tumor. | Larger, irregular, or ulcerated tumors necessitate wider margins. |
Surgical Techniques for Achieving Adequate Margins
Surgical removal of skin cancer requires precise techniques to ensure complete eradication of the disease while minimizing the risk of recurrence. The selection of the optimal surgical technique depends on several factors, including the size, location, and depth of the lesion, as well as the patient’s overall health. Careful consideration of these factors leads to the development of a personalized treatment plan.
Surgical Techniques for Achieving Adequate Margins
Various surgical approaches are used to achieve adequate margins for skin cancer removal. These techniques differ in their invasiveness, complexity, and ability to precisely delineate tumor borders. The goal in each case is to remove all cancerous tissue while preserving healthy skin.
| Surgical Technique | Description | Advantages | Disadvantages |
|---|---|---|---|
| Mohs Micrographic Surgery | A specialized technique where thin layers of tissue are removed and examined microscopically at each stage. This process continues until no cancer cells are detected in the margins. | Highly precise, allows for complete removal of tumor with minimal healthy tissue loss. Excellent for complex or recurrent lesions, and in areas with high cosmetic concern. | Time-consuming and requires specialized expertise. May not be suitable for large lesions. |
| Shave Excision | A less invasive technique where a superficial layer of skin is removed using a scalpel or other sharp instrument. The depth of the excision is typically limited to the epidermis and dermis. | Simple, quick, and less expensive than Mohs surgery. Suitable for small, superficial lesions. | Less precise than Mohs surgery, increasing the risk of incomplete removal and recurrence. May not be suitable for deeper lesions. |
| Excisional Biopsy | A standard surgical technique where a wider margin of tissue is removed around the lesion. The size of the margin depends on the characteristics of the lesion. | Relatively simple, can be performed in most surgical settings. Suitable for various lesion sizes and depths. | Potentially more aggressive than shave excision, higher risk of scarring, and not as precise as Mohs surgery. |
| Curettage and Electrodesiccation | A technique involving scraping the lesion with a curette and using electrical energy to destroy the tissue. It is often combined with excision. | Less invasive than excisional biopsy for small lesions. Quick and effective for superficial lesions. | Limited precision compared to Mohs or excision. May not be appropriate for deep lesions or lesions with indistinct borders. |
Precise Tissue Dissection
Achieving precise tissue dissection is crucial for all surgical techniques. This involves careful and methodical removal of tissue layers to ensure the margins are free of cancer cells. Careful attention to tissue planes is important to avoid damaging healthy tissue.
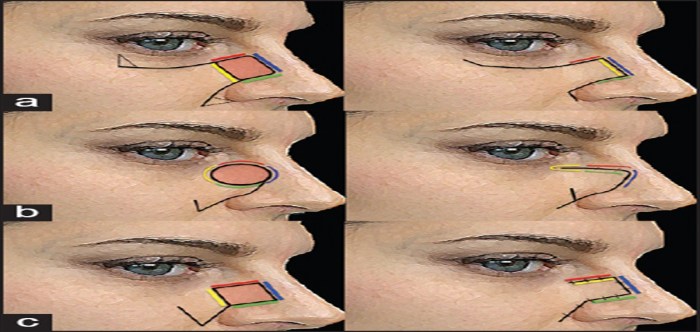
Steps Involved in Mohs Micrographic Surgery
- Anesthesia is administered to the patient.
- The surgeon meticulously removes a thin layer of tissue from the lesion.
- The removed tissue is immediately examined under a microscope to determine the presence of cancer cells.
- If cancer cells are present in the margins, the procedure is repeated until clear margins are achieved.
- The final tissue specimen is carefully examined to ensure that all cancerous cells have been removed.
Steps Involved in Shave Excision
- The patient is given local anesthesia.
- The surgeon uses a scalpel or other sharp instrument to shave off the surface layer of the skin containing the lesion.
- The removed tissue is sent to a pathology laboratory for examination to determine the extent of the lesion.
- Additional excision may be necessary if the pathology report indicates the need for deeper removal.
Steps Involved in Excisional Biopsy
- Anesthesia is administered.
- A wider margin of skin tissue surrounding the lesion is excised.
- The excised tissue is sent for pathological analysis to confirm the diagnosis and assess the presence of cancer cells in the margins.
- Post-operative care is provided.
Steps Involved in Curettage and Electrodesiccation
- The patient is given local anesthesia.
- The surgeon uses a curette to scrape the lesion.
- Electrodesiccation is performed to destroy the remaining tissue.
- The wound is then closed.
- The specimen is sent for analysis to assess the margins.
Histopathological Evaluation of Surgical Margins
The final arbiter of successful skin cancer surgery is the histopathological evaluation of the surgical margins. This crucial step confirms that all cancerous tissue has been removed, minimizing the risk of recurrence. A meticulous examination, employing various techniques, ensures the accuracy and reliability of the diagnosis.Pathologists meticulously analyze the tissue samples to determine if the surgical margins are clear of cancerous cells.
This assessment is essential in determining the effectiveness of the surgery and in guiding subsequent treatment strategies. Understanding the methods and significance of these analyses empowers patients and healthcare providers in making informed decisions about their health.
Methods of Histopathological Analysis
The histopathological analysis of surgical margins involves a series of steps, each contributing to the overall accuracy of the assessment. These steps typically include careful preparation of the tissue sample, staining to enhance visualization of cellular structures, and microscopic examination by a trained pathologist.
Role of Pathologists in Assessing Margin Adequacy
Pathologists play a critical role in determining margin adequacy. They are trained experts in identifying cancerous cells and assessing the presence or absence of cancer cells at the margins of the surgical specimen. Their expertise is essential for accurately characterizing the margin status, which significantly influences treatment decisions. Their meticulous examination and interpretation of the findings are paramount in ensuring appropriate management of the patient.
Significance of Staining Techniques in Margin Evaluation
Various staining techniques are used to enhance the visualization of cellular structures and features in the surgical margin specimens. Hematoxylin and eosin (H&E) staining is a common technique that stains the nuclei blue and the cytoplasm pink, allowing for a general overview of the tissue architecture and the presence of abnormal cells. Other special stains, such as immunohistochemistry (IHC), can target specific proteins or antigens associated with cancer cells, providing additional detail for accurate identification.
This multifaceted approach allows pathologists to evaluate the margin more comprehensively.
Terminology Used to Describe Margin Status
Understanding the terminology used to describe margin status is crucial for interpreting the results of the histopathological evaluation. A “clear margin” indicates that no cancer cells are present at the edge of the surgical specimen. A “close margin” signifies that cancer cells are very close to the surgical margin, often within a predetermined distance. Finally, a “positive margin” indicates that cancer cells are present at the edge of the surgical specimen, requiring further treatment.
Accurate communication of this terminology ensures clarity and proper patient management.
Key Elements of Histopathological Evaluation
| Evaluation Step | Description | Significance |
|---|---|---|
| Specimen Preparation | The surgical specimen is carefully processed, typically involving fixation in formalin, embedding in paraffin wax, and sectioning into thin slices. This ensures structural preservation and facilitates microscopic examination. | Preservation of tissue architecture and cellular details is critical for accurate interpretation. |
| Staining | Staining techniques, such as H&E and IHC, highlight different cellular components and structures. H&E staining provides a general view of tissue morphology, while IHC can identify specific proteins associated with cancer cells. | Enhanced visualization of cellular details and identification of specific markers are crucial for accurate diagnosis. |
| Microscopic Examination | The prepared and stained tissue sections are examined under a microscope by a pathologist. The pathologist meticulously evaluates the presence or absence of cancer cells at the surgical margins, noting their location and characteristics. | Expert visual assessment of margin status is paramount in determining the need for further treatment. |
Management of Positive Surgical Margins
Dealing with a positive surgical margin in skin cancer necessitates a thoughtful and strategic approach. This isn’t a simple “all or nothing” situation, but rather a nuanced process that prioritizes the patient’s well-being and the long-term efficacy of treatment. It requires a combination of re-excision, meticulous follow-up, and a thorough understanding of the potential implications for the patient.
Strategies for Managing Patients with Positive Margins
Positive surgical margins indicate that cancer cells were present at the edge of the removed tissue. This necessitates further intervention to ensure complete removal and prevent recurrence. The strategy employed depends on factors such as the size and location of the tumor, the extent of the positive margin, and the patient’s overall health. Strategies often involve re-excision to achieve wider margins.
Need for Re-excision and Rationale
Re-excision is a crucial component in managing positive margins. It involves surgically removing a wider area of tissue surrounding the original excision site. The rationale behind re-excision is straightforward: to ensure that all cancerous cells are removed and to minimize the risk of recurrence. This approach aims to achieve a clear margin of healthy tissue, providing a barrier against the growth of any residual cancer cells.
Re-excision is often necessary to prevent recurrence, and the success of the treatment is contingent on the surgeon’s expertise in achieving adequate margins.
Importance of Appropriate Follow-Up
Thorough and consistent follow-up is vital after re-excision or any surgical procedure involving skin cancer. Regular check-ups, often including skin examinations and potentially imaging tests, allow for early detection of any recurrence. This proactive approach enables prompt intervention if necessary. Follow-up protocols should be tailored to the individual patient’s situation, factoring in the tumor’s characteristics, the extent of the positive margin, and the patient’s overall health.
Long-Term Implications of Positive Margins, Surgical margin in skin cancer
Positive margins can have significant long-term implications for patients. Recurrence is a potential concern, and the frequency and severity of recurrence can vary greatly depending on factors like the tumor’s aggressiveness, the patient’s immune system, and the effectiveness of the re-excision. The long-term psychological impact on patients is also significant, with anxiety about recurrence being a common issue.
Therefore, providing robust support and ongoing communication with the patient is crucial.
Flowchart of Managing a Patient with a Positive Margin
Start
|
V
Assessment (Patient history, tumor characteristics, etc.)
|
V
Re-excision (Surgical removal of a wider area)
|
V
Histopathological Evaluation (Confirmation of clear margins)
|
V
Follow-up (Regular check-ups, imaging, etc.)
|
V
Monitoring (Continuous surveillance for recurrence)
|
V
...
Prevention of Recurrence Through Surgical Margin: Surgical Margin In Skin Cancer
Surgical margin management plays a crucial role in minimizing the risk of skin cancer recurrence. Careful attention to the extent of resection, surgical technique, and post-operative care significantly impacts long-term outcomes. This meticulous approach is essential for patients with skin cancer, aiming for a complete removal of the cancerous cells and surrounding tissue.
Surgical removal of skin cancer, while often successful, carries the risk of recurrence if the cancerous cells are not completely eradicated. Minimizing this risk necessitates a multi-faceted approach that considers the interplay of surgical precision, patient factors, and the potential for future complications. Achieving an adequate surgical margin is the cornerstone of preventing recurrence and improving patient outcomes.
Strategies to Reduce Recurrence Risk
Minimizing the risk of recurrence involves a proactive and multi-pronged approach to surgical margin management. A crucial aspect is the precise and complete excision of the tumor, ensuring that no cancerous cells remain in the surrounding tissue. This requires meticulous surgical planning and execution.
Surgical Techniques for Wider Margins
Achieving wider surgical margins is a key component in preventing recurrence. Several techniques can be employed to achieve these wider margins, while minimizing the amount of healthy tissue removed. These methods are essential to maximize the chances of complete tumor removal.
- Precise Tumor Localization: Preoperative imaging plays a significant role in accurate tumor localization. High-resolution imaging techniques like Mohs micrographic surgery and advanced imaging techniques help precisely identify the tumor’s boundaries, leading to more precise surgical resection and optimized margin size.
- Advanced Surgical Instruments: Specialized instruments and techniques can enhance the surgeon’s ability to achieve precise excisions, reducing the likelihood of incomplete removal. Examples include electrosurgery, lasers, and specialized scalpels.
- Intraoperative Consultation: Employing intraoperative consultations with pathologists can expedite the process of evaluating margins during the procedure. This real-time assessment can inform surgical decisions, potentially enabling adjustments to the resection margins to ensure adequate removal and minimize the need for a second operation.
Patient Education and Follow-up Care
Patient education and adherence to post-operative follow-up care are vital to long-term success. A thorough understanding of the importance of regular check-ups and prompt reporting of any concerning symptoms is essential for early detection of recurrence.
- Comprehensive Patient Education: Educating patients about the importance of monitoring their surgical site, recognizing potential warning signs, and understanding the rationale behind regular follow-up appointments is paramount. This includes providing detailed instructions and a clear understanding of the potential risks and benefits of the surgical procedure.
- Proactive Monitoring: Post-operative monitoring, including regular physical examinations, imaging studies, and skin assessments, is crucial for early detection of any signs of recurrence. This proactive approach allows for timely intervention if recurrence occurs.
- Promoting Adherence: Encouraging patient adherence to follow-up care and providing resources to support this adherence, such as appointment reminders and clear communication channels, is essential.
Interdisciplinary Collaboration
Collaboration among dermatologists, surgeons, pathologists, and oncologists is essential for optimal patient care. This multidisciplinary approach allows for a comprehensive assessment and management of skin cancer.
- Shared Decision-Making: Collaboration fosters a shared understanding of the patient’s specific needs and preferences, leading to better-informed treatment decisions and improved patient outcomes.
- Comprehensive Care Plans: Interdisciplinary teams create personalized care plans tailored to the patient’s individual circumstances, incorporating insights from different specialists. This comprehensive approach ensures that all aspects of the patient’s care are addressed.
- Enhanced Diagnostic Accuracy: Collaboration among specialists can lead to more accurate diagnoses, enabling timely interventions and potentially improving treatment outcomes.
Optimizing Surgical Margin Management
Optimizing surgical margin management involves a multifaceted strategy that encompasses careful surgical planning, precise surgical techniques, and proactive patient care.
- Standardized Protocols: Implementing standardized protocols for surgical margin assessment, resection, and post-operative care can ensure consistent and high-quality surgical practices.
- Technological Advancements: Integrating advanced technologies, such as real-time imaging and intraoperative pathology, into surgical practice can enhance the precision of tumor removal and margin assessment.
- Continuous Quality Improvement: Continuously evaluating and improving surgical practices through data analysis and feedback mechanisms can optimize margin management strategies and enhance patient outcomes.
Final Wrap-Up
In conclusion, achieving adequate surgical margins is paramount in skin cancer treatment. A thorough understanding of the factors influencing margin determination, coupled with appropriate surgical techniques and meticulous histopathological evaluation, significantly minimizes the risk of recurrence. This comprehensive guide provides a roadmap for effectively managing skin cancer patients, emphasizing the importance of interdisciplinary collaboration and ongoing patient education to optimize outcomes.

Leave a Reply