Which Type of Mouthwash Works Best?
Which type of mouthwash works best? This isn’t a simple question, as the ideal mouthwash depends heavily on individual needs....







Which type of mouthwash works best? This isn’t a simple question, as the ideal mouthwash depends heavily on individual needs....
A 10 panel drug test is a common procedure used to detect the presence of various substances in a person’s...
Coping skills for depression are crucial for managing symptoms and improving overall well-being. This guide explores various coping mechanisms, from...
What causes hair loss? This isn’t just a cosmetic concern; it can significantly impact self-esteem and overall well-being. From genetic...
Longevity to dos for your 30s – Longevity to-dos for your 30s: This isn’t just about hitting your 40s feeling...
How to create the perfect skin care routine is a journey into understanding your skin’s unique needs. It’s not about...
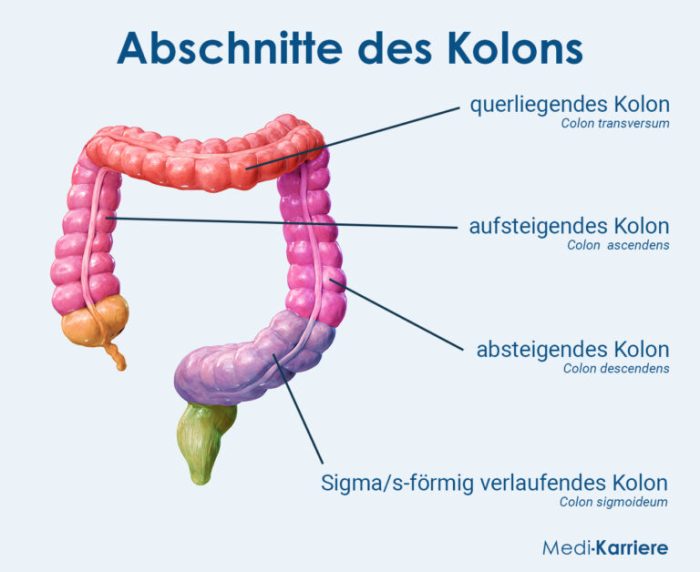
Does IBS cause nausea? This is a common question for those living with Irritable Bowel Syndrome (IBS). While nausea isn’t...
What is incisional hernia? It’s a bulge or protrusion in the abdominal wall, often appearing at the site of a...
How to deliver a baby? This comprehensive guide dives deep into the entire birthing process, from the initial stages of...
How long does COVID headache last? This question plagues many recovering from the virus. This exploration delves into the complexities...