Tylenol Types & Dosages A Comprehensive Guide
Types of tylenol and dosage – Tylenol types and dosages sets the stage for understanding this commonly used pain reliever....







Types of tylenol and dosage – Tylenol types and dosages sets the stage for understanding this commonly used pain reliever....
Three common toenail problems plague millions, causing discomfort and sometimes, more serious issues. From the agonizing pain of ingrown nails...
Is MRSA an STD? This question sparks curiosity and concern, as we delve into the world of Methicillin-resistant Staphylococcus aureus...
Butterfly needles for blood draws and simple IVs are a common and crucial part of medical procedures. This guide dives...
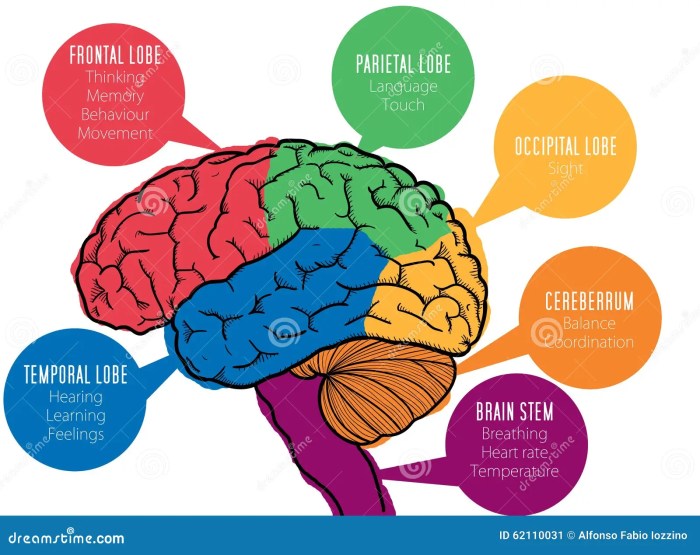
Dyspnea meaning causes symptoms – Dyspnea meaning, causes, and symptoms – this comprehensive guide delves into the complexities of shortness...
Testing for JC virus antibodies is crucial for understanding the presence and activity of this virus, often associated with severe...
Health care sharing ministries offer an alternative to traditional insurance, based on shared responsibility and community values. These ministries, with...
Can yeast infection cause bleeding? This article explores the potential link between these two seemingly disparate conditions. We’ll delve into...
Ismael ruiz my journey with hiv – Ismael Ruiz: My HIV Journey sets the stage for this enthralling narrative, offering...
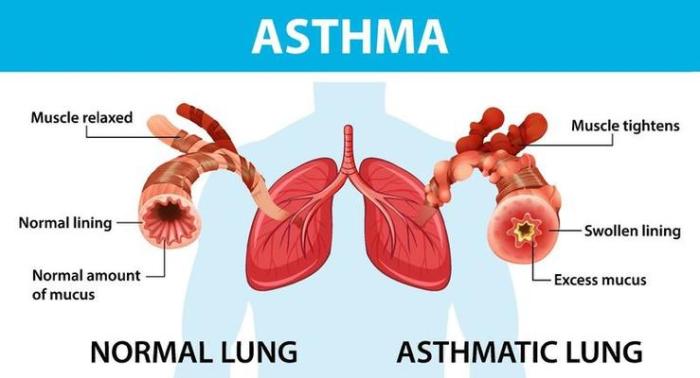
Asthma your immune system – Asthma: Your Immune System’s Role explores the intricate connection between your immune system and asthma....