Atrioventricular nodal reentrant tachycardia avnrt – Atrioventricular nodal reentrant tachycardia (AVNRT) is a common cardiac arrhythmia characterized by a rapid heartbeat originating in the heart’s AV node. This condition can cause palpitations, dizziness, and shortness of breath, and understanding its mechanisms is crucial for effective diagnosis and treatment. We’ll explore the causes, symptoms, diagnosis, and treatment options available for AVNRT, ultimately providing a comprehensive overview of this important cardiac condition.
This in-depth look at AVNRT covers everything from its definition and prevalence to the underlying pathophysiology, clinical manifestations, diagnostic methods, treatment options, and long-term implications. We’ll delve into the heart’s electrical activity during an episode, explore potential triggers, and analyze the various treatment approaches. The goal is to equip readers with a better understanding of this condition, empowering them to ask informed questions of their healthcare providers.
Definition and Epidemiology: Atrioventricular Nodal Reentrant Tachycardia Avnrt
Atrioventricular nodal reentrant tachycardia (AVNRT) is a common type of supraventricular tachycardia (SVT), a rapid heart rhythm originating above the ventricles. It’s characterized by the presence of two separate pathways within the atrioventricular (AV) node, allowing for a re-entrant circuit. This circuit causes the heart to beat abnormally fast. Understanding its prevalence and demographics is crucial for proper diagnosis and management.AVNRT is a relatively prevalent cardiac arrhythmia, though precise figures can vary based on the study methodology and population examined.
It’s estimated to affect a significant portion of the population, particularly in younger adults and adolescents. The precise number of cases is challenging to quantify definitively due to the often asymptomatic nature of the condition in many individuals.
Prevalence and Demographics
The prevalence of AVNRT is estimated to be quite high in the population. While precise numbers are difficult to pinpoint, studies indicate that AVNRT affects a notable portion of the population, with a tendency to be more common in women than men. The condition can manifest at various ages, with the majority of cases occurring in young adults and adolescents, although it can affect individuals of any age.
Risk Factors
While no definitive risk factors are consistently associated with AVNRT, certain predisposing factors may play a role. These factors may include underlying cardiac conditions, structural abnormalities, and certain medications. The exact mechanisms and significance of these potential risk factors are still under investigation.
Age and Gender Distribution
The typical age range for AVNRT presentations often falls within the younger adult and adolescent age groups. While it can affect individuals of any age, the incidence tends to be higher in these younger demographics. Additionally, studies suggest a slight female predominance, but more research is needed to fully understand this pattern.
Comparison with Other Cardiac Arrhythmias
| Arrhythmia | Mechanism | Symptoms | Treatment |
|---|---|---|---|
| AVNRT | Reentrant circuit within the AV node involving two pathways (slow and fast). | Palpitations, rapid heart rate, shortness of breath, chest discomfort, dizziness, lightheadedness. Symptoms can vary in severity and frequency. | Pharmacological interventions (e.g., adenosine, beta-blockers), catheter ablation. |
| Atrial Flutter | Reentrant circuit in the atria, often with a characteristic sawtooth pattern on an ECG. | Similar to AVNRT, including palpitations, rapid heart rate, shortness of breath, and lightheadedness. Symptoms can vary in intensity. | Pharmacological interventions (e.g., calcium channel blockers, beta-blockers), catheter ablation. |
| Atrial Fibrillation | Disorganized electrical activity in the atria. | Palpitations, irregular heart rate, shortness of breath, fatigue, chest discomfort, dizziness. Symptoms can be mild or severe. | Pharmacological interventions (e.g., rate control medications, rhythm control medications), catheter ablation. |
Pathophysiology
Atrioventricular nodal reentrant tachycardia (AVNRT) is a common cardiac arrhythmia characterized by a rapid heart rate originating from abnormal electrical circuits within the heart. Understanding the underlying mechanisms and the role of accessory pathways is crucial for effective diagnosis and treatment. This section delves into the intricate pathophysiology of AVNRT, exploring the electrical conduction abnormalities and the different types of this arrhythmia.The heart’s electrical system normally maintains a coordinated rhythm.
In AVNRT, this coordination is disrupted, leading to a rapid, irregular heartbeat. This disruption stems from the presence of abnormal electrical pathways that allow the heart to re-excite before it has fully recovered. The following sections will detail the specifics of these abnormal pathways and how they contribute to the arrhythmia.
Underlying Mechanisms
AVNRT arises from the presence of two distinct pathways for electrical conduction between the atria and ventricles. These pathways, usually involving the AV node itself, enable the heart to re-enter a rapid cycle of depolarization. The presence of a slow pathway and a fast pathway within the AV node creates the possibility of re-entry. This re-entry circuit allows the impulse to circulate repeatedly, causing the rapid heart rate characteristic of AVNRT.
Role of Accessory Pathways
Accessory pathways, also known as Kent bundles, are abnormal connections between the atria and ventricles that bypass the AV node. While not directly involved in all AVNRT cases, these pathways are a significant contributor in some instances. They facilitate a faster pathway for electrical signals, which can trigger re-entry mechanisms.
Types of AVNRT
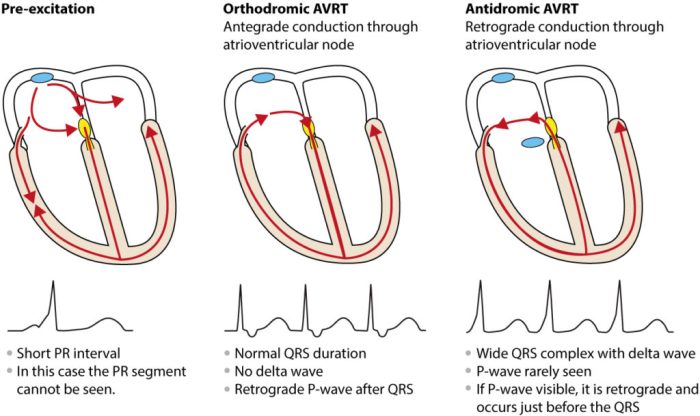
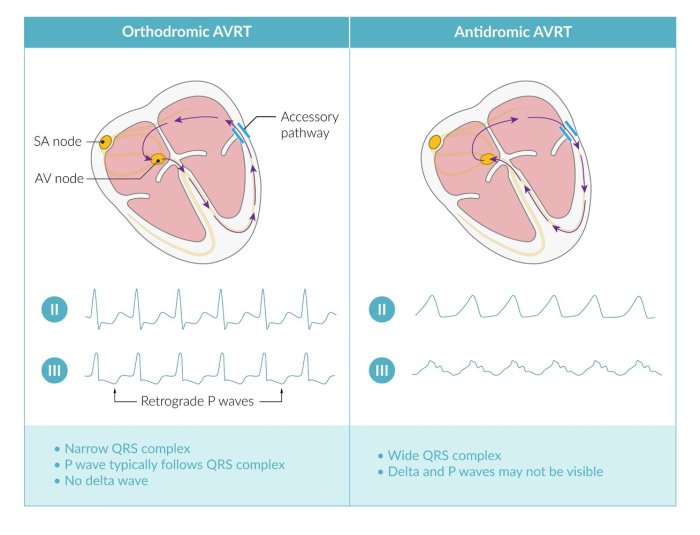
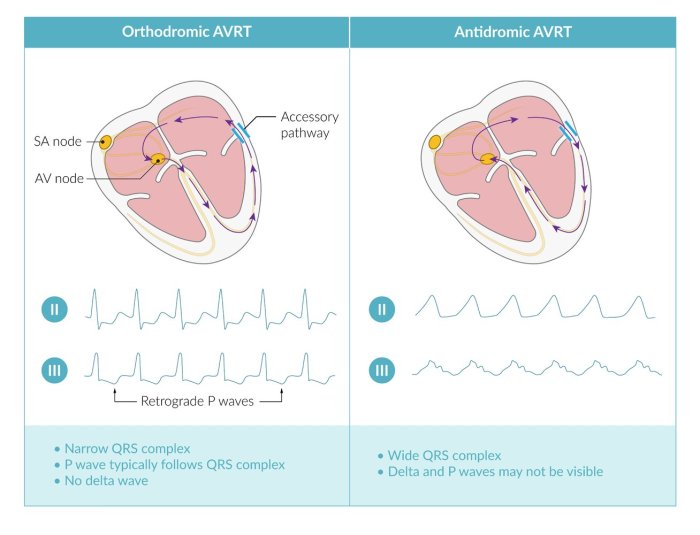
AVNRT can be categorized into two main types:
- Orthodromic AVNRT: In this type, the electrical impulse travels through the normal AV nodal pathway and then the accessory pathway. This is the more common type.
- Antidromic AVNRT: In this case, the electrical impulse travels through the accessory pathway first, and then the AV node. This type is less frequent and may present with slightly different clinical manifestations.
Electrical Conduction Abnormalities
Several electrical conduction abnormalities contribute to the development of AVNRT. These include:
- Re-entry phenomenon: The core mechanism is the creation of a closed loop within the heart. The impulse travels along one pathway, then along a slower pathway, and then back again, repeating the cycle at a rapid rate. This is a crucial component of AVNRT.
- AV nodal conduction abnormalities: The AV node, a critical part of the heart’s electrical system, can exhibit abnormalities in its conduction properties. This can result in the slower pathway necessary for re-entry to exist within the node itself.
- Accessory pathway conduction: The presence of accessory pathways allows for alternative conduction routes. This, combined with the slower pathway, allows for re-entry and the rapid heart rate.
Electrical Activity During an AVNRT Episode
The electrical activity during an AVNRT episode involves a repetitive circuit. A diagram depicting the electrical activity would show:
- Atrial depolarization: The atria are stimulated, and the impulse begins its journey.
- AV nodal activation: The impulse travels through both the fast and slow pathways of the AV node.
- Ventricular depolarization: The impulse reaches the ventricles and causes them to contract.
- Re-entry: The impulse travels back to the atria through either the AV node or the accessory pathway, depending on the type of AVNRT. The impulse will continue to circulate repeatedly at a rapid pace.
Illustrative Diagram (Note: This is not an image, but a descriptive explanation of a hypothetical diagram):Imagine a circular pathway composed of two interconnected lines representing the AV node’s fast and slow pathways. A third line representing the accessory pathway branches off the fast pathway. The arrows indicate the direction of electrical impulse propagation. The closed loop created by these lines represents the re-entry circuit responsible for the rapid firing.
Clinical Manifestations
AVNRT, while often manageable, can significantly impact a patient’s quality of life. Understanding its clinical presentation is crucial for prompt diagnosis and effective treatment. Recognizing the symptoms and potential triggers allows for better patient management and potentially prevents complications.Common symptoms associated with AVNRT episodes frequently include palpitations, a feeling of a rapid or irregular heartbeat. These sensations can vary in intensity and duration, impacting the patient’s ability to perform daily tasks.
Beyond palpitations, other symptoms can accompany AVNRT, and the severity of these symptoms can vary greatly between individuals.
Common Symptoms
Patients experiencing AVNRT often report a range of symptoms. These symptoms, while variable, provide important clues to the underlying condition. Recognizing these symptoms and their associated severity levels can facilitate appropriate medical intervention.
- Palpitations: A sensation of a rapid, fluttering, or pounding heartbeat is a hallmark symptom. This can range from a mild awareness of a quickened heart rate to a more pronounced, alarming sensation. The palpitations may be described as “skipped beats” or “racing heart” and can be intermittent or persistent.
- Shortness of breath: Dyspnea, or difficulty breathing, is a possible symptom, particularly if the rapid heart rate impairs the heart’s ability to efficiently pump blood. This can be a noticeable and distressing symptom, sometimes leading to anxiety or panic.
- Lightheadedness or dizziness: These symptoms are often related to the heart’s inability to adequately circulate blood to the brain, leading to a decreased blood supply. This can result in a feeling of lightheadedness or dizziness, potentially causing falls or other safety concerns.
- Anxiety or nervousness: The rapid heart rate and associated symptoms can induce feelings of anxiety or nervousness, often exacerbating the symptoms themselves. The experience of these feelings can create a cycle of increased heart rate and anxiety, making the symptoms more pronounced.
- Chest discomfort or pain: Some patients may experience mild chest discomfort or pain, which is often described as a pressure or tightness in the chest. While not a common symptom, it can be a significant concern and should be evaluated by a healthcare professional.
Triggers for AVNRT Episodes
Certain factors can precipitate or exacerbate AVNRT episodes. Understanding these triggers can assist in managing the condition and potentially preventing episodes.
- Stress: Emotional stress, anxiety, and intense physical exertion can stimulate the autonomic nervous system, increasing the likelihood of an AVNRT episode. This is a significant trigger, as it highlights the interplay between emotional state and cardiac function.
- Caffeine and alcohol: These substances can stimulate the heart and increase the risk of AVNRT episodes. Their effect on the cardiovascular system should be considered, particularly in individuals prone to these episodes.
- Certain medications: Some medications can trigger or worsen AVNRT. This underscores the importance of discussing medication use with a healthcare professional, especially for those with a history of this condition.
- Hypokalemia (low potassium levels): Electrolyte imbalances, such as low potassium levels, can affect the heart’s electrical conduction system, increasing the susceptibility to AVNRT. Maintaining appropriate electrolyte balance is essential.
Severity of Symptoms
The intensity and duration of AVNRT symptoms vary considerably among patients. This variability necessitates a personalized approach to diagnosis and management.
| Symptom | Description | Severity (mild/moderate/severe) |
|---|---|---|
| Palpitations | A brief, mild awareness of a rapid heartbeat. | Mild |
| Palpitations | Frequent, noticeable rapid heartbeat lasting several minutes. | Moderate |
| Palpitations | Severe, prolonged rapid heartbeat causing significant distress and breathing difficulty. | Severe |
| Shortness of breath | Mild shortness of breath during exertion. | Mild |
| Shortness of breath | Significant shortness of breath, limiting daily activities. | Moderate |
| Shortness of breath | Severe shortness of breath, requiring medical attention. | Severe |
| Lightheadedness | Mild dizziness or lightheadedness. | Mild |
| Lightheadedness | Significant dizziness or lightheadedness, potentially leading to falls. | Moderate |
| Lightheadedness | Severe dizziness, loss of consciousness. | Severe |
ECG Findings in AVNRT, Atrioventricular nodal reentrant tachycardia avnrt
The electrocardiogram (ECG) is a valuable tool in diagnosing AVNRT. Characteristic ECG patterns provide crucial information about the arrhythmia.
- Rapid heart rate: The ECG will show a rapid heart rate, typically above 150 beats per minute. This is a key indicator.
- Short PR interval: A shortened PR interval is often observed, indicating the presence of an accessory pathway. This is a key diagnostic finding.
- Atrial fibrillation or flutter: In some cases, atrial fibrillation or flutter may be seen preceding or concurrent with the AVNRT episode. This can provide valuable diagnostic insights.
Diagnosis
Unmasking Atrioventricular Nodal Reentrant Tachycardia (AVNRT) hinges on a meticulous diagnostic approach. A thorough understanding of the patient’s symptoms, coupled with a comprehensive evaluation of their electrocardiogram (ECG), plays a pivotal role in accurate diagnosis. This section delves into the various diagnostic tools used, emphasizing the crucial role of ECG and patient history.
Atrioventricular nodal reentrant tachycardia (AVNRT) can cause some uncomfortable heart racing, and it’s crucial to manage underlying factors. While not directly related, excessive protein intake can sometimes lead to issues like dehydration or electrolyte imbalances, which can potentially worsen some heart conditions. For more on the potential side effects of consuming too much protein, check out this helpful resource: too much protein side effects.
Ultimately, maintaining a healthy diet, in conjunction with proper medical care, is key to managing AVNRT effectively.
Electrocardiographic (ECG) Findings
ECG is the cornerstone of diagnosing AVNRT. Its diagnostic utility stems from its ability to visualize the electrical activity of the heart over time. Specific ECG features are highly suggestive of AVNRT. These include a narrow complex tachycardia, typically with a rapid ventricular rate (ranging from 150-250 bpm). The presence of a PR interval that is either normal or shortened, as well as a consistently short or absent P wave, are often observed.
A common observation is the presence of a retrograde P wave hidden within the QRS complex, sometimes referred to as a “premature atrial contraction.” These observations aid in differentiating AVNRT from other tachycardias.
Additional Diagnostic Tests
While ECG is the primary diagnostic tool, additional tests may be employed to confirm the diagnosis or rule out other possibilities. These tests can provide more comprehensive insights into the patient’s cardiac function and overall health. For instance, an echocardiogram can assess the structure and function of the heart, excluding structural abnormalities or valvular disease that could be contributing to the tachycardia.
Exercise testing may be used to evaluate the patient’s response to physical stress and to identify any changes in heart rate or rhythm. Holter monitoring, a continuous ECG recording over 24 hours or more, can be used to capture the tachycardia events as they occur in the patient’s natural environment.
Patient History
A detailed patient history is indispensable in the diagnostic process. The patient’s symptoms, such as palpitations, shortness of breath, and chest pain, can offer crucial clues. The frequency and duration of these symptoms, as well as any precipitating factors (e.g., stress, caffeine intake), can significantly assist in the diagnostic evaluation. Symptoms such as dizziness or lightheadedness may be indicative of the tachycardia’s impact on the body.
Furthermore, a thorough medical history, including any prior cardiac conditions or medications, can be helpful. This context aids in understanding the patient’s overall health status and aids in the diagnostic process.
Diagnostic Flowchart
The following flowchart illustrates the diagnostic process for AVNRT.
Start --> Patient History (Symptoms, Frequency, Duration, Precipitating factors) --> ECG (Narrow complex tachycardia, short/absent P waves, PR interval) --> Additional Tests (Echocardiogram, Holter Monitoring, Exercise testing) --> Diagnosis (AVNRT)
Treatment and Management
Atrioventricular nodal reentrant tachycardia (AVNRT) is often manageable with various approaches, ranging from lifestyle adjustments to more invasive procedures. Understanding the different treatment options and their efficacy is crucial for patients and healthcare providers to make informed decisions.
Atrioventricular nodal reentrant tachycardia (AVNRT) is a type of heart arrhythmia that can cause uncomfortable palpitations. While it’s important to get these checked out, it’s also crucial to be aware of the potential differences between digestive issues like Irritable Bowel Syndrome (IBS) and more serious conditions like colon cancer, especially when symptoms overlap. Understanding the distinctions between these conditions is vital for proper diagnosis and treatment.
For a deeper dive into the complexities of IBS versus colon cancer, check out this helpful resource: ibs vs colon cancer. Ultimately, seeking professional medical advice is key for any health concerns, including AVNRT.
This section details the diverse strategies for tackling AVNRT, highlighting the role of medications, catheter ablation, and other considerations.
The choice of treatment for AVNRT hinges on several factors, including the frequency and severity of episodes, the patient’s overall health, and their preference. Mild or infrequent cases may respond well to lifestyle modifications and medication, while more persistent or severe episodes often necessitate catheter ablation.
Medication Management
Medications play a crucial role in managing AVNRT, particularly for patients experiencing occasional episodes. These drugs primarily aim to slow down the heart rate and reduce the likelihood of AVNRT occurrences. Beta-blockers, such as metoprolol or atenolol, are commonly prescribed due to their effectiveness in decreasing heart rate and conduction velocity. Calcium channel blockers, like verapamil or diltiazem, are another class of drugs that can effectively control heart rate and potentially reduce AVNRT episodes.
Catheter Ablation Procedure
Catheter ablation is a highly effective procedure for treating AVNRT. It involves inserting thin, flexible tubes (catheters) into blood vessels, guided by imaging techniques like fluoroscopy, to reach the specific area in the heart where the abnormal electrical pathway is located. Radiofrequency energy is then delivered through the catheters to precisely destroy the tissue responsible for the reentrant circuit, effectively eliminating the abnormal electrical signal.
Atrioventricular nodal reentrant tachycardia (AVNRT) is a heart rhythm issue that can cause palpitations. While not directly related, understanding conditions like congenital adrenal hyperplasia symptoms can be insightful when considering potential underlying causes of heart irregularities. For example, certain hormonal imbalances, as seen in congenital adrenal hyperplasia symptoms , can sometimes indirectly affect the heart’s electrical system, potentially contributing to AVNRT.
Ultimately, proper diagnosis and treatment of AVNRT require a comprehensive evaluation by a medical professional.
Efficacy Comparison of Treatment Approaches
While medication can effectively control symptoms in many cases, catheter ablation offers a more definitive and potentially curative approach. Medication is often a first-line treatment, but its effectiveness varies considerably among individuals. In some cases, medication may only provide temporary relief, and the frequency of episodes may increase over time. Catheter ablation, on the other hand, is generally considered curative in the majority of patients who undergo the procedure successfully.
Long-term follow-up studies demonstrate a high success rate in preventing recurrence of AVNRT after ablation.
Potential Complications of Treatment
Any medical procedure carries potential risks, and AVNRT treatment is no exception. While complications are generally rare, understanding the potential side effects is essential for informed decision-making. Complications related to medication include, but are not limited to, hypotension, bradycardia, and other adverse drug reactions. Catheter ablation carries risks such as bleeding, infection, pericardial effusion (fluid buildup around the heart), and cardiac perforation (a hole in the heart).
Lifestyle Modifications
Lifestyle adjustments can complement medication management, playing a significant role in managing the frequency and severity of AVNRT episodes. These adjustments include maintaining a healthy weight, regular exercise, and a balanced diet. Adequate hydration and stress reduction techniques can also contribute to better overall heart health and reduce triggers for AVNRT.
Prognosis and Long-Term Implications
AVNRT, while often manageable, can have a significant impact on a patient’s overall well-being and future health. Understanding the potential long-term implications is crucial for both patients and healthcare providers to develop effective strategies for managing the condition. This section will explore the prognosis for AVNRT, potential complications, the importance of monitoring, the impact on quality of life, and preventative measures.
The prognosis for AVNRT is generally favorable. Most individuals with occasional episodes can lead normal lives with appropriate medical management. However, the severity and frequency of episodes can vary significantly, impacting the quality of life and potentially leading to more serious complications if left untreated.
Prognosis for Patients with AVNRT
The prognosis for AVNRT is typically excellent, especially when episodes are infrequent and mild. The condition rarely progresses to life-threatening complications in these cases. With proper management, most individuals with AVNRT can maintain a good quality of life. However, the risk of complications increases with the frequency and severity of episodes.
Potential Long-Term Complications
Chronic episodes of AVNRT can potentially lead to a number of long-term complications, although these are less common in patients with infrequent episodes. One concern is the development of structural heart disease over time, although the link is not fully understood. In some cases, recurrent episodes can contribute to cardiac fatigue and reduce overall physical endurance. Moreover, prolonged periods of rapid heartbeats can lead to symptoms like lightheadedness or fainting.
Furthermore, the sustained stress on the heart can, in rare cases, lead to more severe heart rhythm disturbances.
Importance of Ongoing Monitoring and Follow-up
Regular monitoring and follow-up are essential for managing AVNRT effectively. This involves close monitoring of heart rate and rhythm, especially after the initial diagnosis and treatment. This can be achieved through periodic checkups, electrocardiograms (ECGs), and Holter monitoring to detect any recurrence or changes in heart activity. Ongoing monitoring helps in early identification of potential complications and allows for prompt intervention if needed.
Impact of AVNRT on Patient Quality of Life
AVNRT can significantly impact a patient’s quality of life, particularly if episodes are frequent and severe. The palpitations, dizziness, and shortness of breath associated with AVNRT can interfere with daily activities, social interactions, and overall well-being. The anxiety and fear associated with these episodes can also contribute to a reduced quality of life. In severe cases, the constant worry about the next episode can lead to psychological distress.
Potential Preventative Measures for Future AVNRT Episodes
Although a complete cure for AVNRT isn’t always possible, various measures can help reduce the risk of future episodes. Maintaining a healthy lifestyle, including a balanced diet, regular exercise, and stress management techniques, is important. Furthermore, adherence to prescribed medications and lifestyle changes can help regulate heart rate and rhythm, thus potentially preventing or reducing the frequency of episodes.
Final Review
In conclusion, atrioventricular nodal reentrant tachycardia (AVNRT) is a complex cardiac arrhythmia with a range of presentations and potential consequences. Understanding its underlying mechanisms, clinical features, and diagnostic tools is essential for appropriate management. From lifestyle modifications to medical interventions and ablation procedures, various treatment strategies are available. Ultimately, a multidisciplinary approach, involving patients, physicians, and other healthcare professionals, is vital to ensure optimal outcomes and maintain a high quality of life for individuals affected by AVNRT.

Leave a Reply