Pcos and weight loss why it is so hard – PCOS and weight loss: why it is so hard? This isn’t just about willpower; it’s a complex interplay of hormonal imbalances, metabolic hurdles, and lifestyle factors. Understanding the underlying mechanisms behind PCOS weight resistance is key to developing effective strategies for weight management. This exploration dives deep into the science, offering practical insights into dietary approaches, exercise routines, lifestyle modifications, and even medical interventions, helping you navigate this challenging journey.
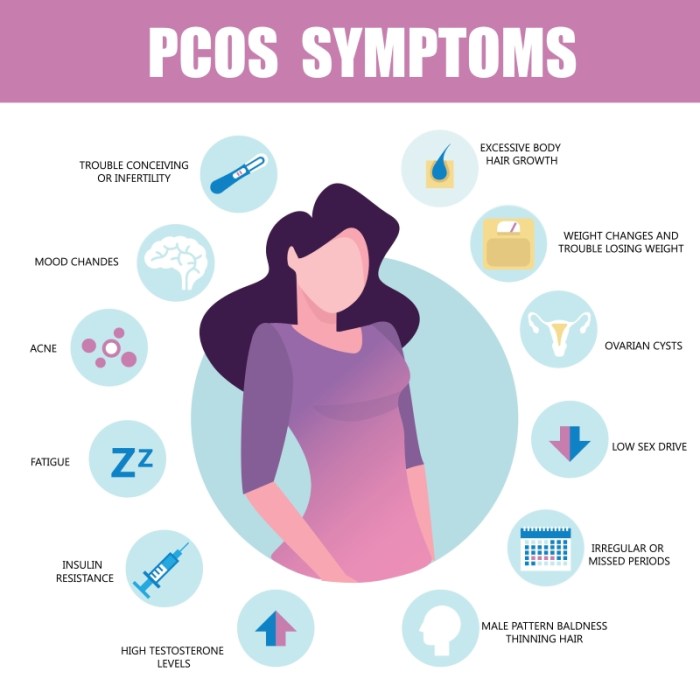
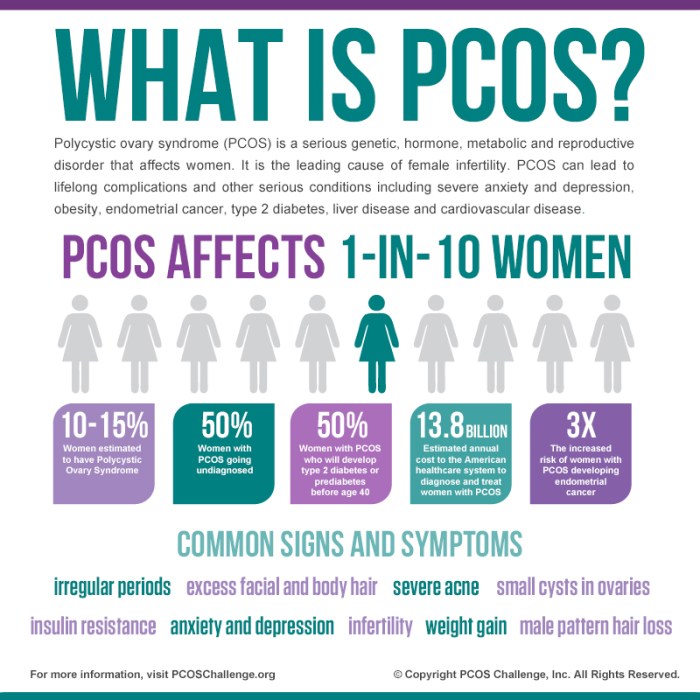
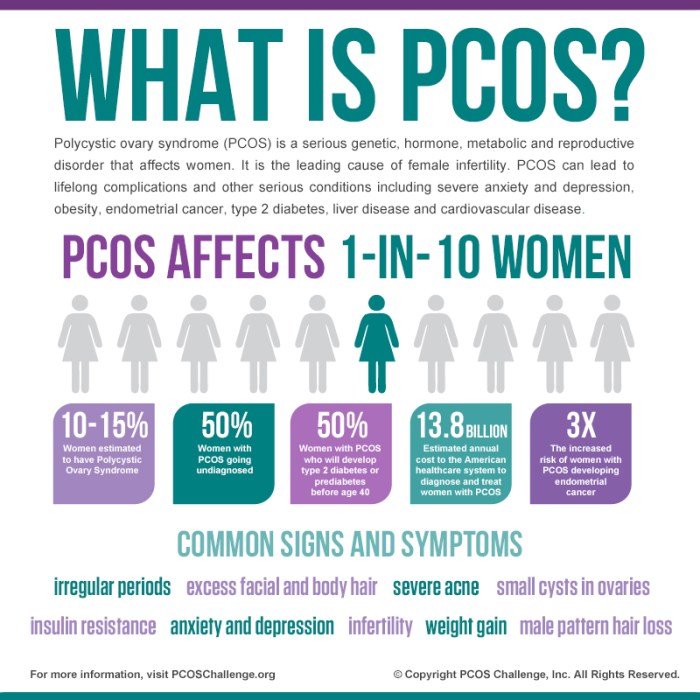
Hormonal imbalances, like insulin resistance and androgen excess, disrupt your body’s natural processes, making it harder to lose weight. This is further complicated by inflammation and issues with appetite regulation. The difficulty isn’t just about eating less; it’s about changing how your body functions. Understanding these mechanisms is the first step toward finding a path forward.
Underlying Mechanisms of PCOS and Weight Loss Resistance
Losing weight with PCOS can feel like an uphill battle. The hormonal and metabolic complexities of the condition often create roadblocks, making even the most dedicated efforts feel frustratingly ineffective. This isn’t about a lack of willpower, but rather about understanding the underlying mechanisms that contribute to weight gain and resistance to weight loss. This exploration dives into the intricacies of these mechanisms, helping to illuminate the path towards more effective strategies.The hormonal landscape of PCOS is deeply intertwined with weight management.
The key players—insulin resistance, androgen excess, and inflammation—all exert their influence on metabolic pathways, making weight loss a challenging process. Understanding these mechanisms can empower individuals with PCOS to develop personalized strategies that address the specific hurdles they face.
Hormonal Imbalances and Weight Gain
PCOS is characterized by a complex interplay of hormonal imbalances. Elevated levels of androgens, such as testosterone, are frequently observed, which can contribute to increased appetite and altered fat distribution. Insulin resistance is another hallmark, leading to higher blood sugar levels and further exacerbating the tendency to store fat. These hormonal factors are crucial to understand for effective weight management.
Metabolic Pathways Affected by PCOS
The metabolic pathways affected by PCOS significantly impact weight loss efforts. Insulin resistance disrupts glucose metabolism, impairing the body’s ability to utilize glucose for energy and leading to its storage as fat. This impaired insulin sensitivity can trigger an increase in fat storage, particularly around the abdomen. Furthermore, androgen excess can affect the body’s ability to utilize fat for energy, making it harder to break down stored fat and maintain a healthy weight.
Insulin Resistance vs. Androgen Excess
Insulin resistance and androgen excess exert different influences on weight distribution and loss. Insulin resistance typically leads to central obesity, characterized by fat accumulation around the abdomen. Androgen excess, on the other hand, can contribute to a more overall increase in body fat and changes in body shape, including an increase in facial and body hair. Understanding these differences helps tailor strategies for targeting specific areas of concern.
Inflammation in PCOS and Weight Loss, Pcos and weight loss why it is so hard
Chronic low-grade inflammation is often associated with PCOS. This inflammatory state can negatively impact fat storage and metabolism. The inflammation can increase the body’s tendency to store fat and reduce the efficiency of burning fat for energy. This contributes to the challenge of losing weight.
Appetite Regulation and Satiety
PCOS can affect appetite regulation and satiety signals. The hormonal imbalances can lead to increased hunger and reduced feelings of fullness. This can contribute to overeating, even when a person feels they’ve already consumed enough food. This is a critical factor to address in any weight management strategy.
Fat Utilization for Energy
The body’s ability to utilize fat for energy can be compromised in PCOS. The hormonal imbalances can impair the breakdown of stored fat, making it harder to tap into these reserves for fuel. This can make weight loss even more challenging.
Trying to lose weight with PCOS is a real struggle, isn’t it? It’s like battling a complex system that often sabotages your efforts. Sometimes, seemingly unrelated factors like experiencing contagious and infectious diarrhea contagious and infectious diarrhea can further complicate things, impacting your appetite and overall well-being. This just adds another layer of difficulty to the already challenging path of weight management for those with PCOS.
Key Hormonal Factors in PCOS and Weight Loss Resistance
| Hormonal Factor | Connection to Weight Loss Resistance |
|---|---|
| Elevated Androgens (e.g., testosterone) | Increased appetite, altered fat distribution, impaired fat utilization. |
| Insulin Resistance | Impaired glucose metabolism, increased fat storage, reduced insulin sensitivity. |
| Inflammation | Increased fat storage, reduced fat metabolism. |
| Leptin Resistance | Impaired satiety signals, increased appetite, potentially altered fat storage. |
| Estrogen Imbalance | Potentially contributing to fat distribution and metabolic dysregulation. |
Dietary Strategies for PCOS and Weight Management
Navigating PCOS often feels like a balancing act, especially when weight loss is a goal. Understanding how diet interacts with PCOS is crucial for managing symptoms and achieving sustainable weight management. The right dietary approach can significantly impact insulin sensitivity, hormone regulation, and overall well-being. This section explores effective dietary strategies, focusing on personalized plans that can work for you.Dietary approaches for PCOS patients need to be tailored to individual needs and preferences, acknowledging that a one-size-fits-all approach rarely works.
Finding a sustainable eating pattern that supports both weight loss and symptom management is paramount. The following sections detail specific dietary strategies and considerations for PCOS-related weight management.
Effective Dietary Approaches for PCOS
A key aspect of successful weight management for PCOS is implementing a well-structured dietary plan that supports insulin sensitivity and hormone balance. Focus on nutrient-dense foods that provide sustained energy and promote satiety. This approach is more sustainable than restrictive diets and helps manage cravings.
Specific Foods Supporting Weight Loss and PCOS Symptom Management
Certain foods can play a positive role in both weight loss and managing PCOS symptoms. Prioritize whole, unprocessed foods. These include fruits, vegetables, lean proteins, and whole grains. Examples include berries, leafy greens, fish, poultry, and quinoa. Foods high in fiber are particularly beneficial as they promote satiety and regulate blood sugar levels.
Comparing Dietary Patterns for PCOS and Weight Loss
Different dietary patterns can be effective for PCOS and weight loss, but some are more suitable than others. A low-carb diet can help regulate blood sugar and reduce insulin resistance, which is often a challenge for PCOS. The Mediterranean diet, rich in fruits, vegetables, healthy fats, and lean proteins, offers a balanced approach to nutrition, supporting hormone regulation and overall health.
While both can be effective, individual responses vary. A personalized approach is crucial, considering individual preferences and needs.
Portion Control and Mindful Eating for PCOS
Portion control is essential for anyone aiming for weight loss, but it’s particularly crucial for individuals with PCOS. Mindful eating involves paying attention to hunger and fullness cues, eating slowly, and savoring each bite. This approach helps prevent overeating and promotes a healthier relationship with food. Tracking food intake and maintaining a food journal can be helpful tools in achieving mindful eating.
Dealing with PCOS and weight loss is tough. Hormonal imbalances make it incredibly challenging to shed those extra pounds. Sometimes, nerve pain can be a factor too, impacting your motivation and ability to exercise. Finding the right medication, like gabapentin, for managing nerve pain can be a real game-changer, but it’s crucial to understand the appropriate dosage and duration.
For example, if you’re curious about how long to take gabapentin for nerve pain, check out this helpful resource: how long to take gabapentin for nerve pain. Ultimately, consistent lifestyle changes and professional guidance are key to successfully navigating PCOS-related weight struggles.
Managing Cravings and Emotional Eating Related to PCOS
PCOS can lead to fluctuations in hormone levels, contributing to increased cravings and emotional eating. Addressing the underlying hormonal imbalances is crucial. Identify triggers for emotional eating and develop coping mechanisms such as stress management techniques and healthy outlets for emotional expression. Working with a registered dietitian can help develop strategies for managing cravings and emotional eating in the context of PCOS.
The Role of Micronutrients and Vitamins in PCOS-Related Weight Loss
Certain micronutrients and vitamins play a crucial role in managing PCOS and supporting weight loss. For example, vitamin D deficiency is often linked to PCOS. Ensuring adequate intake of vitamins and minerals through a balanced diet or supplements, if necessary, can be beneficial. A registered dietitian or healthcare professional can provide personalized recommendations for micronutrient intake.
Sample Meal Plans for PCOS Patients
| Meal | Description | Portion Size (Approximate) | Nutrient Highlights |
|---|---|---|---|
| Breakfast (Option 1) | Greek Yogurt with Berries and Nuts | 1 cup yogurt, ½ cup berries, ¼ cup nuts | Protein, fiber, healthy fats |
| Lunch (Option 1) | Salad with Grilled Chicken or Fish | Large salad with 4oz lean protein, 2 cups vegetables | Protein, fiber, healthy fats |
| Dinner (Option 1) | Baked Salmon with Quinoa and Asparagus | 4oz salmon, ½ cup quinoa, 1 cup asparagus | Protein, fiber, healthy fats, complex carbohydrates |
Note: These are sample meal plans and portion sizes may vary based on individual needs and calorie requirements. Consulting with a registered dietitian or healthcare professional is recommended for personalized meal plans.
Exercise and Physical Activity Recommendations
Moving your body is crucial for managing PCOS and achieving weight loss. Exercise isn’t just about burning calories; it plays a vital role in improving insulin sensitivity, reducing stress, and boosting overall well-being, all of which are significantly impacted by PCOS. Finding the right exercise routine that fits your lifestyle and energy levels is key.Exercise routines should be tailored to individual needs and preferences, while considering the potential challenges of PCOS.
It’s essential to prioritize consistency and gradual progression to avoid injury and ensure long-term success. Remember, every little bit counts.
Types of Exercise Most Effective for PCOS-Related Weight Loss
Cardiovascular exercise, strength training, and flexibility exercises all contribute to weight loss and overall health. Aerobic activities like brisk walking, jogging, swimming, or cycling help burn calories and improve cardiovascular health, which are important components of a PCOS management strategy. Resistance training builds muscle mass, increasing your metabolism and further aiding in weight loss. Flexibility exercises, such as yoga or stretching, improve range of motion, reduce muscle stiffness, and promote overall well-being.
Choosing a combination of these types of exercise is ideal for optimal results.
Exercise Routines Tailored for Individuals with PCOS
Tailoring exercise routines to accommodate PCOS-related symptoms is crucial. Consider starting with shorter durations of exercise and gradually increasing the intensity and duration as your body adapts. Prioritize low-impact activities to minimize discomfort and pain. For example, a beginner routine might include 20-30 minutes of brisk walking three times a week, progressing to 45 minutes four times a week as fitness improves.
Consistency is key. Listen to your body, and rest when needed.
Dealing with PCOS and weight loss can feel like a constant uphill battle. Hormonal imbalances make it tough to shed those extra pounds, and sometimes, even the healthiest eating habits struggle to make a difference. Knowing which foods can support your weight loss journey is key, and incorporating plenty of fruits, like those highlighted in this article about best fruits for weight loss , can be a great starting point.
But even with the best diet plan, the complexities of PCOS still make it a challenging road to navigate.
Importance of Consistency and Gradual Progression
Consistency is paramount in any exercise program, especially for individuals with PCOS. A regular exercise routine, even if it’s just 15-30 minutes a day, will lead to significant improvements over time. Gradual progression is equally important to avoid injuries and burnout. Increasing the intensity or duration of workouts too quickly can lead to setbacks. For instance, instead of jumping from a 15-minute walk to a 60-minute run, gradually increase the duration and intensity of workouts, allowing your body to adjust.
Role of Exercise in Improving Insulin Sensitivity and Blood Sugar Control
Exercise improves insulin sensitivity, helping your body utilize glucose more effectively. This is vital for managing blood sugar levels, a common challenge for those with PCOS. Regular physical activity can reduce the risk of developing type 2 diabetes, a serious health concern often associated with PCOS. For example, studies show that individuals with PCOS who engaged in regular exercise had improved insulin sensitivity and lower blood sugar levels compared to those who were inactive.
Impact of Exercise on Stress Management
Exercise is a powerful stress reliever. Physical activity releases endorphins, which have mood-boosting effects and can help manage stress, a common symptom experienced by individuals with PCOS. Incorporating stress-reducing activities like yoga or meditation into your routine can further enhance the benefits of exercise. For instance, a 30-minute yoga session can be a valuable addition to an exercise routine, promoting relaxation and stress management.
Contribution of Exercise to Overall Well-being and Mental Health
Exercise contributes significantly to overall well-being and mental health in individuals with PCOS. Regular physical activity can improve mood, reduce anxiety, and enhance self-esteem. Exercise provides a healthy outlet for stress, promoting a sense of accomplishment and control over one’s health. For example, many individuals with PCOS report feeling more positive and empowered after engaging in regular exercise, which positively impacts their mental health.
Table: Exercise Types and Potential Benefits for PCOS Weight Loss
| Exercise Type | Potential Benefits for PCOS Weight Loss |
|---|---|
| Brisk Walking | Burns calories, improves cardiovascular health, low-impact, accessible |
| Swimming | Full-body workout, low-impact, excellent for cardiovascular health |
| Cycling | Low-impact cardio, good for joint health, enjoyable |
| Yoga | Improves flexibility, strength, and balance; stress reduction |
| Strength Training | Builds muscle mass, increases metabolism, improves bone density |
| Dancing | Fun and engaging cardio, improves coordination, boosts mood |
Lifestyle Modifications for PCOS and Weight Loss: Pcos And Weight Loss Why It Is So Hard
Navigating PCOS often feels like a marathon, not a sprint. While diet and exercise are crucial, truly conquering PCOS requires a holistic approach. Lifestyle modifications, encompassing stress management, sleep hygiene, and consistent habits, play a significant role in both weight loss and symptom management. These strategies are not just about the numbers on the scale; they’re about reclaiming energy, improving overall well-being, and fostering a healthier relationship with your body.Beyond the typical dietary and exercise routines, incorporating proactive stress management and adequate sleep significantly impacts PCOS symptom control and weight loss efforts.
This is because these factors directly influence hormone regulation, insulin sensitivity, and overall metabolic health, which are often disrupted in PCOS. By integrating these strategies, individuals can create a more supportive environment for their bodies to achieve optimal results.
Stress Management Techniques
Stress, a common element in modern life, can exacerbate PCOS symptoms and hinder weight loss efforts. Chronic stress elevates cortisol levels, a hormone that can disrupt insulin sensitivity and promote fat storage, particularly in the abdominal region. Therefore, implementing stress management techniques is vital for effective PCOS management.Effective stress reduction techniques include mindfulness practices like meditation and deep breathing exercises.
These practices help calm the nervous system, reduce cortisol levels, and improve overall well-being. Yoga and tai chi also combine physical postures, breathing techniques, and mindfulness, offering a holistic approach to stress management. Regular practice of these techniques can improve emotional regulation and create a more balanced response to stress. Furthermore, seeking support from a therapist or counselor can provide a structured environment for processing emotions and developing coping mechanisms.
Importance of Adequate Sleep
Adequate sleep is a cornerstone of overall health, and for individuals with PCOS, it’s even more crucial. Sleep deprivation disrupts the delicate hormonal balance in the body, impacting insulin sensitivity and metabolism. Poor sleep quality can lead to increased cortisol levels and decreased leptin, a hormone that regulates appetite and energy expenditure. Consequently, individuals with PCOS are more prone to experiencing cravings and accumulating excess body fat.
Aiming for 7-9 hours of quality sleep each night is essential for optimal hormonal regulation and weight management.Creating a consistent sleep schedule, establishing a relaxing bedtime routine, and optimizing the sleep environment (dark, quiet, cool room) are crucial steps in improving sleep quality. Avoid caffeine and alcohol close to bedtime, and ensure your bedroom is conducive to sleep.
Lifestyle Modifications for Improved Insulin Sensitivity and Weight Loss
A comprehensive lifestyle plan for PCOS weight loss involves more than just diet and exercise. Implementing strategies to improve insulin sensitivity and support overall metabolic health is key. These strategies, combined with dietary and exercise plans, create a powerful synergistic effect.
- Prioritize whole, unprocessed foods: Focus on a diet rich in fruits, vegetables, whole grains, lean proteins, and healthy fats. This approach provides essential nutrients, supports blood sugar control, and promotes satiety, ultimately aiding weight management.
- Engage in regular physical activity: Combining cardiovascular exercise with strength training can significantly enhance insulin sensitivity. Regular physical activity improves blood sugar control and aids in weight management, contributing to a more balanced hormonal profile.
- Manage stress effectively: Incorporating stress-reducing techniques into daily routines can help regulate cortisol levels and improve insulin sensitivity. This promotes a more stable hormonal environment, supporting weight loss efforts.
- Prioritize sufficient sleep: Aiming for 7-9 hours of quality sleep each night is essential for optimal hormone regulation, metabolic function, and weight management.
- Manage stress effectively: Chronic stress negatively impacts insulin sensitivity and can worsen PCOS symptoms. Mindfulness practices, meditation, or deep breathing exercises can help regulate stress levels.
Connection Between Sleep Quality and PCOS-Related Hormonal Imbalances
Sleep quality and PCOS-related hormonal imbalances are closely intertwined. Sleep deprivation can disrupt the circadian rhythm, which regulates hormones like cortisol and leptin. This disruption can negatively affect insulin sensitivity, potentially worsening PCOS symptoms and making weight loss more challenging. Improving sleep hygiene and ensuring adequate sleep duration are essential for managing PCOS-related hormonal imbalances.
Comprehensive Lifestyle Plan
The following table Artikels a comprehensive lifestyle plan integrating diet, exercise, stress management, and sleep for PCOS weight loss.
| Category | Strategies |
|---|---|
| Diet | Focus on whole, unprocessed foods, manage portion sizes, control refined carbohydrates and sugary drinks, and increase fiber intake. |
| Exercise | Incorporate both cardiovascular and strength training exercises, aim for at least 150 minutes of moderate-intensity aerobic activity per week and incorporate strength training exercises two to three times per week. |
| Stress Management | Practice mindfulness techniques like meditation, deep breathing exercises, yoga, or tai chi. Seek professional support if needed. |
| Sleep | Prioritize 7-9 hours of quality sleep each night. Establish a consistent sleep schedule, create a relaxing bedtime routine, and optimize your sleep environment. |
Medical Interventions and Support
Navigating PCOS and weight loss can feel like a marathon, not a sprint. While lifestyle changes are crucial, medical interventions can play a significant role in optimizing your journey. Understanding the options available and communicating effectively with your healthcare provider is key to a successful approach.Medical interventions, when combined with lifestyle modifications, can often lead to more significant and sustainable weight loss results for individuals with PCOS.
These interventions target the underlying hormonal imbalances that contribute to weight gain and resistance to weight loss.
Role of Medication in PCOS Management
Medications can be valuable tools in managing PCOS symptoms and potentially aiding weight loss. They often work by addressing hormonal imbalances, improving insulin sensitivity, or reducing androgen levels. The effectiveness of these medications varies from person to person, and the decision to use them should be made in consultation with a healthcare professional.
Types of Medications for PCOS
Several medications can be used to manage PCOS symptoms. Their potential impact on weight varies.
- Metformin: This medication is frequently prescribed to improve insulin sensitivity. While not a direct weight loss medication, improved insulin sensitivity can often lead to better weight management by reducing the body’s tendency to store fat and improve metabolism. Many individuals report a positive correlation between metformin use and weight loss, though the effect varies.
- Birth Control Pills (Combined Oral Contraceptives): These pills can regulate menstrual cycles, reduce androgen levels, and improve acne, all of which can indirectly impact weight management. The impact on weight is usually not significant, but it can contribute to a more stable hormonal environment.
- Anti-androgen Medications: These medications, such as spironolactone, are used to reduce the levels of androgens, which can lead to acne, hair growth, and potentially weight gain. They may aid in weight loss by reducing factors that contribute to hormonal imbalances. The weight loss effect is not always substantial but may be a beneficial component in a broader treatment plan.
Importance of Regular Check-ups and Monitoring
Regular check-ups with your healthcare provider are essential for monitoring your progress and adjusting your treatment plan as needed. Blood tests to assess hormone levels, blood sugar, and other relevant factors provide crucial information. This ongoing monitoring ensures that the chosen medications are effective and safe.
Healthcare Professionals’ Role in Guiding Weight Loss Strategies
Your healthcare provider plays a vital role in guiding you through the weight loss process. They can provide personalized advice, tailor treatment plans to your specific needs, and address any concerns or side effects. They can also help in creating a holistic approach to weight loss, encompassing lifestyle modifications and medical interventions.
Support Systems for PCOS Patients
Finding support is crucial in managing PCOS. Support groups and online communities offer valuable resources, providing a platform for sharing experiences, advice, and encouragement. They can help individuals feel less isolated and more empowered in their journey.
Effective Communication Strategies
Open and honest communication with your healthcare provider is essential. Clearly articulate your concerns, goals, and any challenges you face. Actively listen to their advice and recommendations, and ask questions to ensure you understand the treatment plan.
| Medical Intervention | Potential Effect on Weight Loss in PCOS |
|---|---|
| Metformin | May improve insulin sensitivity, potentially leading to weight loss |
| Birth Control Pills | May improve hormonal balance, with potential for modest weight impact |
| Anti-androgen Medications | May reduce factors contributing to weight gain, potentially aiding weight loss |
Potential Challenges and Considerations
Losing weight with PCOS can be a complex journey, often fraught with more than just dietary and exercise hurdles. Beyond the biological factors, psychological and societal pressures significantly impact the success and sustainability of weight loss efforts. Understanding these challenges is crucial for developing effective strategies to support individuals through this process.Navigating the emotional landscape of weight loss is just as important as understanding the underlying hormonal imbalances.
Many individuals with PCOS experience feelings of frustration, disappointment, and even shame when weight loss progress stalls. This emotional toll can undermine motivation and lead to a vicious cycle of discouragement. Acknowledging and addressing these emotional factors is essential for sustained success.
Common Obstacles to Weight Loss in PCOS
Weight loss struggles in PCOS are often multi-faceted. Beyond the hormonal influences, practical issues like time constraints, access to resources, and social support can impede progress. Individuals may face challenges in finding the time for regular exercise or healthy meal preparation. Furthermore, navigating social situations that revolve around food can be difficult for those with PCOS, often requiring significant adjustments and strategies to cope with social pressure.
Psychological Factors Influencing Weight Loss in PCOS
Psychological factors play a significant role in weight loss journeys, especially for individuals with PCOS. Low self-esteem, body image issues, and feelings of inadequacy can create a negative self-perception that hinders progress. Depression and anxiety, which are sometimes associated with PCOS, can also contribute to feelings of hopelessness and a lack of motivation to pursue healthy habits. These psychological factors often interact with the physical challenges, making weight loss an even more intricate and personal experience.
Importance of Realistic Expectations and Positive Mindset
Setting unrealistic weight loss goals is a common pitfall. Focusing on gradual, sustainable progress, rather than quick fixes, is crucial. A positive mindset, built on self-compassion and a realistic understanding of the complexities of PCOS, is essential. Recognizing that weight loss might not be linear, and that setbacks are part of the process, allows individuals to maintain motivation and perseverance.
Societal Pressures and Body Image Concerns
Societal pressures to conform to specific body ideals can be particularly challenging for individuals with PCOS. The constant exposure to unrealistic beauty standards and the emphasis on thinness can contribute to body image concerns and feelings of inadequacy. Internalizing these pressures can lead to emotional distress and hinder efforts to embrace a healthy lifestyle.
Strategies for Overcoming Challenges and Maintaining Motivation
Overcoming obstacles requires a multifaceted approach. Seeking support from a healthcare team, including endocrinologists, registered dietitians, and mental health professionals, is crucial. Creating a supportive network of friends and family who understand the challenges can provide encouragement and accountability. Building a strong support system, which may include online communities or support groups for PCOS, can offer valuable insights and strategies.
Comparison of Support Systems
Different support systems offer varying levels of effectiveness. Healthcare professionals provide expert guidance and personalized strategies, while support groups offer peer-to-peer support and shared experiences. Online communities can offer broad access to information and diverse perspectives, but may lack the individualized attention of professional guidance. Ultimately, the most effective approach often involves a combination of these resources.
Table of Common Challenges and Suggested Strategies
| Challenge | Suggested Strategies |
|---|---|
| Time constraints | Prioritize short, manageable workouts; plan healthy meals in advance; utilize quick, healthy recipes. |
| Social pressures | Communicate needs and boundaries clearly; practice self-care; surround yourself with supportive individuals; educate others about PCOS. |
| Body image concerns | Focus on overall health and well-being; celebrate progress; practice self-compassion; seek professional guidance. |
| Lack of motivation | Set realistic goals; reward progress; find activities you enjoy; connect with a support group. |
| Financial limitations | Explore affordable meal options; seek out local resources; consider food banks or assistance programs. |
End of Discussion
In conclusion, successfully navigating PCOS weight loss requires a multifaceted approach. Addressing the underlying hormonal and metabolic issues, coupled with targeted dietary strategies, exercise routines, and lifestyle modifications, is crucial. Remember that support from healthcare professionals and potentially medical interventions are vital components of a comprehensive plan. This isn’t about quick fixes; it’s about creating sustainable habits that support long-term well-being.
Don’t give up – you’ve got this.

Leave a Reply