Does insulin cause weight gain? This question sparks intense debate, and this deep dive explores the complex relationship between insulin and weight management. We’ll unravel the intricate mechanisms behind insulin’s actions, examining its effects on different bodily systems and how it impacts weight gain or loss. From the role of diet and exercise to potential clinical considerations, we’ll provide a comprehensive overview of this multifaceted topic.
Understanding insulin’s role in regulating blood sugar is crucial. High insulin levels can lead to increased fat storage, but the story is far more nuanced than a simple cause-and-effect relationship. Other factors like genetics, lifestyle, and overall health play a vital part. This exploration delves into the factors that influence insulin sensitivity, the impact of chronic high insulin levels, and the ways different treatments and interventions can address the issue.
Mechanism of Insulin Action
Insulin, a vital hormone produced by the pancreas, plays a crucial role in maintaining blood glucose homeostasis. It orchestrates a complex series of events to regulate glucose levels, ensuring that cells receive the energy they need while preventing harmful spikes or drops. Understanding this intricate process is essential for comprehending how insulin affects weight management and overall health.Insulin’s primary function is to facilitate the uptake of glucose from the bloodstream into cells.
This process, triggered by insulin binding to specific receptors on cell surfaces, is crucial for providing cells with the fuel they require for various metabolic activities. The efficiency of this process significantly impacts energy utilization and storage.
Insulin and Glucose Uptake
Insulin promotes glucose uptake by stimulating the translocation of glucose transporter proteins (GLUTs) to the cell membrane. These proteins act as channels, enabling glucose to move from the blood into the cells. The most important of these transporters, GLUT4, is particularly sensitive to insulin. In the absence of insulin, GLUT4 primarily resides within intracellular vesicles, limiting glucose entry.
Upon insulin binding, the vesicles fuse with the cell membrane, bringing GLUT4 to the surface and enabling glucose uptake. This process is crucial for maintaining normal blood glucose levels.
Effects of Insulin on Different Tissues
Insulin’s effects differ depending on the tissue type, reflecting the specific metabolic needs and functions of each.
- Muscle Tissue: Insulin stimulates glucose uptake and utilization in muscle cells for energy production and glycogen synthesis. It also promotes protein synthesis, crucial for muscle growth and repair. This effect is particularly important for individuals engaging in regular physical activity, as it facilitates the delivery of glucose for energy and aids in post-exercise recovery.
- Liver Tissue: In the liver, insulin inhibits gluconeogenesis (the production of glucose from non-carbohydrate sources) and promotes glycogen synthesis, the process of converting glucose into glycogen for storage. This helps to lower blood glucose levels and maintain a healthy glucose balance.
- Adipose Tissue (Fat Tissue): Insulin promotes glucose uptake in fat cells and stimulates the synthesis of fatty acids and triglycerides. This process stores excess glucose as fat, contributing to energy reserves. This action is essential for energy storage and utilization, especially during periods of fasting or low-calorie intake.
Role of Insulin in Glycogen Synthesis and Storage
Glycogen synthesis is a critical process facilitated by insulin. It involves the conversion of glucose into glycogen, a storage form of glucose, primarily in the liver and muscle. This process is crucial for maintaining blood glucose levels between meals and during periods of fasting. Insulin directly promotes the activation of enzymes involved in glycogen synthesis, ensuring the efficient conversion and storage of glucose.
Adequate glycogen storage is vital for maintaining energy availability throughout the day.
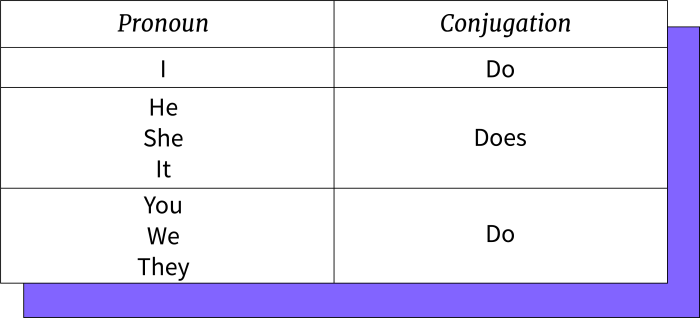
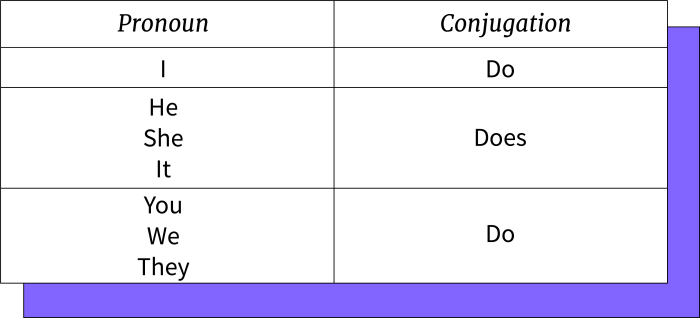
Comparison of Insulin Effects on Different Cell Types
| Cell Type | Glucose Uptake | Glycogen Synthesis | Fatty Acid Synthesis | Protein Synthesis |
|---|---|---|---|---|
| Muscle | High | High | Low | High |
| Liver | Moderate | High | Moderate | Low |
| Adipose | High | Low | High | Low |
Insulin’s actions on various tissues, as demonstrated in the table, are highly regulated and coordinated to maintain glucose homeostasis. These actions are crucial for overall metabolic health.
Potential for Weight Gain
Insulin, a crucial hormone for regulating blood sugar, plays a complex role in weight management. While insulin’s primary function is to facilitate glucose uptake into cells, its actions extend beyond this, influencing fat storage and utilization. Understanding this intricate relationship is essential for managing weight effectively.Insulin’s Influence on Fat StorageInsulin is a key player in the body’s fat storage mechanisms.
When blood sugar levels rise, insulin signals the body to store excess glucose as glycogen in the liver and muscles, and as fat in adipose tissue. This process is vital for maintaining energy balance. However, chronically elevated insulin levels can lead to a significant increase in fat storage, potentially contributing to weight gain. The body becomes increasingly efficient at storing fat, making it challenging to lose weight.Factors Influencing Insulin Sensitivity and ResistanceInsulin sensitivity refers to the body’s ability to respond effectively to insulin.
Conversely, insulin resistance is a condition where cells don’t respond adequately to insulin, leading to elevated insulin levels in the bloodstream. Several factors influence insulin sensitivity and resistance, including:
- Diet: A diet high in processed foods, refined carbohydrates, and saturated fats can contribute to insulin resistance. Conversely, a balanced diet rich in whole foods, fruits, vegetables, and lean proteins can improve insulin sensitivity.
- Physical Activity: Regular exercise improves insulin sensitivity and helps regulate blood sugar levels. Inactivity often leads to insulin resistance.
- Genetics: Genetic predisposition can influence insulin sensitivity. Individuals with a family history of diabetes or obesity are more prone to developing insulin resistance.
- Stress: Chronic stress can disrupt hormonal balance, including insulin regulation, potentially contributing to insulin resistance.
- Sleep Deprivation: Adequate sleep is crucial for insulin regulation. Sleep deprivation can impair insulin sensitivity and increase the risk of insulin resistance.
Impact of Chronic High Insulin Levels on Body WeightChronic high insulin levels significantly impact body weight. Elevated insulin promotes fat storage, inhibits fat breakdown, and often results in an overall increase in body fat. This can lead to weight gain, particularly in the abdominal area.Different Ways Insulin Affects Body CompositionInsulin’s influence on body composition extends beyond simply promoting fat storage.
It also affects protein synthesis and utilization, potentially impacting muscle mass. Additionally, insulin can influence appetite and food cravings, which further contribute to weight gain.Potential Consequences of Insulin Resistance on Weight ManagementThe table below Artikels potential consequences of insulin resistance on weight management.
| Aspect | Potential Consequences |
|---|---|
| Weight Gain | Increased fat storage, particularly in the abdominal region. Difficulty losing weight despite dietary restrictions and exercise. |
| Metabolic Health | Increased risk of type 2 diabetes, heart disease, and other chronic conditions. |
| Hormonal Imbalance | Disruption of hormonal balance, leading to further complications in weight management and overall health. |
| Food Cravings and Appetite | Increased cravings for sugary and high-carbohydrate foods, potentially contributing to overeating and weight gain. |
| Physical Activity | Reduced physical activity levels due to fatigue and other related symptoms. |
Factors Influencing Weight Changes
Understanding weight changes is a complex interplay of various factors. While insulin’s role in metabolism is undeniable, other aspects of lifestyle significantly impact how our bodies store and utilize energy. This includes everything from the foods we consume to the amount of sleep we get, and even the medications we take. This section will explore these influencing factors in detail.Insulin sensitivity isn’t a static condition; it’s dynamic and responsive to numerous external and internal factors.
The way we eat, exercise, manage stress, and even the medications we take all play crucial roles in modulating insulin’s effect on our bodies. These factors are not independent entities but interconnected pieces of a larger puzzle, and understanding their influence is vital for effective weight management.
Diet and Exercise in Managing Blood Sugar and Weight
Diet and exercise are cornerstones of healthy blood sugar management and weight control. A balanced diet rich in fruits, vegetables, whole grains, and lean proteins helps regulate blood sugar levels, preventing significant spikes and promoting steady energy release. Regular physical activity enhances insulin sensitivity, allowing the body to utilize glucose more effectively. Exercise also contributes to calorie expenditure, promoting weight loss and maintenance.
Individuals with prediabetes or type 2 diabetes can often improve their condition through dietary adjustments and regular exercise, potentially delaying or even preventing the onset of complications.
Stress, Sleep, and Insulin Sensitivity
Chronic stress can negatively impact insulin sensitivity. Stress hormones like cortisol can interfere with the body’s ability to utilize insulin effectively, leading to elevated blood sugar levels and potentially hindering weight loss efforts. Adequate sleep is equally important for maintaining healthy insulin sensitivity. Sleep deprivation can disrupt metabolic processes, impacting glucose metabolism and increasing the risk of insulin resistance.
While the connection between insulin and weight gain is often debated, it’s important to remember that other factors play a crucial role. Certain medications, like some used to treat high blood pressure or other conditions, can sometimes lead to unexpected side effects like tinnitus. For a comprehensive list of medications linked to this auditory issue, check out this resource on medications that can cause tinnitus.
Ultimately, understanding the complex interplay of factors affecting weight gain, and the potential side effects of various treatments, is key to a healthier lifestyle.
Prioritizing stress reduction techniques like mindfulness and ensuring sufficient sleep are crucial for optimizing insulin function and weight management.
Different Types of Carbohydrates and Insulin Release
Different types of carbohydrates have varying effects on insulin release. Simple carbohydrates, like white bread and sugary drinks, are rapidly digested, causing a rapid surge in blood sugar and insulin. Complex carbohydrates, found in whole grains, fruits, and vegetables, are digested more slowly, leading to a more gradual increase in blood sugar and a more sustained release of insulin.
Choosing complex carbohydrates over simple ones can be beneficial for maintaining stable blood sugar levels and promoting weight management.
Medications and Insulin Sensitivity
Certain medications can impact insulin sensitivity. Some medications, such as corticosteroids, can increase blood sugar levels and reduce insulin effectiveness. Others, such as certain antipsychotics and some blood pressure medications, can also affect insulin sensitivity. Individuals taking medications should discuss their potential impact on blood sugar and insulin sensitivity with their healthcare provider to ensure appropriate monitoring and management.
It is important to note that this is not an exhaustive list, and specific medications may have unique effects.
Lifestyle Factors Impacting Insulin Function
Numerous lifestyle factors can influence insulin function. These include:
- Dietary Habits: A diet high in processed foods, refined sugars, and saturated fats can contribute to insulin resistance. Conversely, a diet rich in whole foods, fiber, and lean proteins can promote healthy insulin function.
- Physical Activity: Regular exercise, including both aerobic and strength training, can enhance insulin sensitivity and promote weight management.
- Stress Management: Chronic stress can impair insulin function. Implementing stress-reduction techniques, such as yoga, meditation, or spending time in nature, can be beneficial.
- Sleep Quality: Adequate sleep is essential for regulating metabolic processes, including insulin function. Prioritizing sufficient sleep can contribute to improved insulin sensitivity.
- Alcohol Consumption: Excessive alcohol consumption can negatively affect insulin sensitivity and potentially contribute to weight gain.
- Smoking: Smoking is associated with insulin resistance and may hinder weight management efforts.
- Medications: Certain medications can impact insulin sensitivity. Consulting a healthcare provider is essential to understand any potential effects.
By understanding and addressing these factors, individuals can take proactive steps to optimize their insulin function and achieve better weight management outcomes.
Clinical Considerations: Does Insulin Cause Weight Gain
Understanding insulin resistance and its link to weight gain is crucial for effective management. Doctors use a multi-faceted approach, combining assessment, diagnostics, lifestyle modifications, and potentially medications to help patients navigate this complex issue. This section delves into the practical aspects of clinical evaluation and treatment.
Evaluating Insulin Resistance and Weight Impact
Doctors assess insulin resistance by considering a patient’s medical history, physical examination findings, and laboratory results. A key aspect is identifying patterns of weight gain, particularly central obesity (fat accumulation around the abdomen), a common characteristic associated with insulin resistance. This assessment often includes detailed discussions about dietary habits, physical activity levels, and any pre-existing conditions that might contribute to the issue.
Blood tests are essential for measuring various parameters.
So, does insulin cause weight gain? It’s a complex question, and the answer isn’t a simple yes or no. While insulin’s role in storing glucose is crucial, understanding how it interacts with the body’s systems is key. For instance, the patellofemoral joint, the connection between your kneecap and thigh bone, what is the patellofemoral joint , plays a vital part in movement and overall health, but its function isn’t directly related to insulin’s effect on weight.
Ultimately, a balanced diet and regular exercise are far more important factors in weight management than focusing solely on insulin.
Diagnostic Methods for Insulin Resistance
Several diagnostic methods help identify insulin resistance. Fasting insulin levels and glucose tolerance tests are frequently employed. The oral glucose tolerance test (OGTT) measures how the body responds to a glucose load. An elevated fasting insulin level or impaired glucose tolerance often suggests insulin resistance. Further evaluation might include assessing for specific genetic predispositions or other hormonal imbalances.
Lifestyle Interventions for Weight Management
Lifestyle interventions are fundamental in managing weight gain related to insulin resistance. Dietary modifications play a significant role. These include adopting a balanced diet rich in whole grains, fruits, vegetables, and lean proteins, while limiting processed foods, sugary drinks, and excessive saturated fats. Regular physical activity, such as brisk walking, jogging, or cycling, is crucial for improving insulin sensitivity and promoting weight loss.
Adequate sleep is also essential as sleep deprivation can disrupt metabolic processes and contribute to weight gain.
Medications to Address Insulin Resistance and Weight
In some cases, medications can assist in managing insulin resistance and its associated weight gain. Metformin, a commonly prescribed medication for type 2 diabetes, is often used to improve insulin sensitivity and may contribute to weight loss in certain individuals. Other medications might be considered in specific cases, but it’s crucial to consult a healthcare professional to determine the most appropriate course of action.
These decisions are personalized based on individual patient needs and risk factors.
Lifestyle vs. Medication-Based Treatments
| Feature | Lifestyle-Based Treatment | Medication-Based Treatment |
|---|---|---|
| Mechanism | Improving insulin sensitivity and promoting healthy metabolic function through diet, exercise, and lifestyle changes. | Directly affecting insulin production, action, or sensitivity through pharmaceutical intervention. |
| Effectiveness | Generally effective when consistently adhered to, demonstrating long-term positive impact on overall health and reducing risk factors. | Can be effective but may not address the underlying causes of insulin resistance, potentially leading to dependence or adverse side effects. |
| Side Effects | Minimal, primarily related to patient compliance with dietary and exercise regimens. | Potentially various, ranging from mild gastrointestinal issues to more serious health concerns; carefully monitored by medical professionals. |
| Cost | Generally lower, primarily requiring investment in healthy foods and gym memberships. | Higher, as medications can be expensive and may need long-term commitment. |
| Long-term impact | Promotes sustained health improvements and long-term weight management. | May be effective in the short-term but long-term efficacy can vary depending on the individual and medication. |
Illustrative Examples
Understanding the complex interplay between insulin, weight, and overall health requires looking at real-world scenarios. These examples illustrate how insulin resistance and weight gain can manifest, and how lifestyle interventions can help manage and reverse these effects. They also highlight the importance of personalized approaches to weight management.Insulin resistance, a condition where the body doesn’t respond effectively to insulin, often leads to weight gain.
This is not always straightforward; genetics, lifestyle choices, and other health factors influence the relationship. The following examples demonstrate this dynamic.
While some folks worry about insulin causing weight gain, it’s a bit more complex than that. Focusing on a balanced diet and regular exercise can significantly impact weight management, regardless of insulin levels. This is particularly important during the winter months when seasonal affective disorder (SAD) can impact our mood and motivation. Fortunately, there are some great strategies for coping with SAD, such as light therapy and spending time outdoors.
Check out these 4 ways to tackle seasonal affective disorder for some helpful tips. Ultimately, a healthy lifestyle encompassing both mental and physical well-being is key to managing weight and overall health.
Hypothetical Case Study: Insulin Resistance and Weight Gain
A 45-year-old woman, Sarah, presents with a history of gestational diabetes and a family history of type 2 diabetes. She has gradually gained weight over the past five years, despite maintaining a relatively consistent diet and activity level. Blood tests reveal elevated fasting blood glucose and insulin levels, indicative of insulin resistance. This resistance causes the body to produce more insulin to compensate, leading to a cycle of weight gain and further insulin resistance.
Sarah’s lifestyle, including her diet and exercise routine, needs to be tailored to address her specific condition.
Healthy Diet Plan for Optimal Insulin Function
A healthy diet for optimal insulin function prioritizes whole, unprocessed foods. It emphasizes complex carbohydrates, lean proteins, and healthy fats. This diet plan incorporates the following principles:
- Prioritize whole grains: Opt for brown rice, quinoa, oats, and whole-wheat bread over refined grains. These complex carbohydrates are digested more slowly, preventing blood sugar spikes and promoting steady insulin release.
- Include lean protein sources: Incorporate lean meats, poultry, fish, beans, lentils, and tofu. Protein helps stabilize blood sugar levels and promotes satiety.
- Focus on healthy fats: Include sources like avocados, nuts, seeds, and olive oil. Healthy fats support hormone regulation and satiety.
- Control portion sizes: Portion control is crucial for maintaining a healthy weight and managing insulin levels. Consider using smaller plates and bowls.
- Limit processed foods, sugary drinks, and excessive saturated and trans fats: These foods contribute to blood sugar fluctuations and hinder insulin function.
Exercise Regimen for Improved Insulin Sensitivity
A regular exercise routine plays a vital role in improving insulin sensitivity and weight management. The following regimen incorporates both aerobic and resistance training:
- Aerobic exercise: Aim for at least 150 minutes of moderate-intensity aerobic exercise per week, such as brisk walking, jogging, cycling, or swimming.
- Resistance training: Incorporate strength training exercises two to three times a week. Focus on compound exercises like squats, lunges, push-ups, and rows. This helps build muscle mass, which improves insulin sensitivity.
- Consistency is key: Regularity in exercise is more effective than sporadic intense workouts. Start slowly and gradually increase the intensity and duration as your fitness level improves.
Medication-Based Treatments and Weight Management
Certain medications, such as metformin, can improve insulin sensitivity and help with weight management in individuals with type 2 diabetes or prediabetes. This can improve overall health and well-being, and also positively impact weight loss efforts.
Lifestyle Interventions for Positive Impact
Numerous lifestyle interventions can positively impact insulin function and weight loss. These include:
- Stress management techniques: Chronic stress can negatively impact insulin sensitivity. Practices like meditation, yoga, and deep breathing can help manage stress levels.
- Adequate sleep: Sufficient sleep is essential for hormone regulation, including insulin function. Aim for 7-9 hours of quality sleep per night.
- Hydration: Drinking plenty of water is crucial for overall health and can contribute to satiety, aiding in weight management.
- Support network: Seeking support from friends, family, or a healthcare professional can help individuals stay motivated and accountable on their weight loss journey.
Misconceptions and Controversies
The relationship between insulin and weight gain is often shrouded in misconceptions and fueled by conflicting narratives. While insulin’s role in regulating blood sugar is crucial, the idea that it directly and invariably leads to weight gain is a simplification. Understanding the nuances of this relationship requires delving into the common arguments, examining the scientific evidence, and identifying misleading information.Misconceptions surrounding insulin and weight gain often stem from a misunderstanding of its complex interplay with various physiological factors.
These misunderstandings can lead to anxieties and misinformed dietary choices, potentially hindering effective weight management strategies.
Common Misconceptions
Misconceptions about insulin’s role in weight gain are prevalent. A common one is the belief that simply consuming carbohydrates triggers an immediate and excessive insulin release, leading to rapid weight gain. This oversimplification ignores the intricate processes that govern carbohydrate metabolism and the body’s capacity to regulate blood sugar.
Prevalent Arguments
One prevalent argument is that high-carbohydrate diets inevitably lead to elevated insulin levels, promoting fat storage. Another is that insulin’s primary function is to facilitate fat storage, regardless of other factors. These arguments, while seemingly logical, often lack the context of individual metabolic responses, the role of other hormones, and the significance of lifestyle factors.
Scientific Evidence
The scientific evidence suggests a more nuanced picture. While insulin does play a role in glucose metabolism and fat storage, it’s not the sole determinant of weight gain. Other factors, such as genetics, physical activity, and overall caloric intake, significantly influence body weight. The impact of insulin on weight gain is highly dependent on individual metabolic profiles, which vary considerably.
Misleading Information, Does insulin cause weight gain
Misleading information about insulin and weight gain is widespread. Some sources imply a direct correlation between insulin and weight gain, neglecting the complex interplay of factors. Others may focus solely on the hormonal aspect while ignoring the importance of diet and exercise. These simplifications often result in an inaccurate understanding of the mechanisms involved.
Accurate vs. Inaccurate Information
| Aspect | Accurate Information | Inaccurate Information |
|---|---|---|
| Insulin’s Role | Insulin is essential for glucose uptake and utilization, and plays a role in fat storage, but it’s not the sole determinant of weight gain. | Insulin is the primary driver of fat storage, regardless of other factors. |
| Carbohydrate Consumption | High carbohydrate intake, if combined with excess calories and insufficient physical activity, can contribute to weight gain, but it doesn’t automatically lead to excessive insulin secretion or weight gain in everyone. | High carbohydrate intake invariably leads to excessive insulin release and weight gain. |
| Individual Variation | Metabolic responses to carbohydrates and insulin vary significantly between individuals, influenced by genetics, lifestyle, and health conditions. | Metabolic responses are uniform, and everyone reacts similarly to insulin and carbohydrate intake. |
Future Research Directions
Unraveling the intricate relationship between insulin, weight, and related factors demands further exploration. Current research provides a solid foundation, but significant knowledge gaps remain, particularly regarding the complex interplay of genetics, lifestyle, and environmental influences. Future studies can refine our understanding and ultimately lead to more effective strategies for weight management and prevention of insulin resistance.
Investigating the Role of Gut Microbiota
The human gut microbiome plays a crucial role in metabolism and energy regulation. Emerging evidence suggests a strong correlation between gut microbiota composition and insulin sensitivity. Future research should focus on characterizing the specific microbial communities associated with insulin resistance and weight gain. Studies employing metagenomic sequencing and functional analyses of gut microbiota can shed light on the mechanisms by which these communities influence insulin action.
For instance, research could investigate the impact of prebiotics and probiotics on insulin sensitivity in individuals with varying degrees of weight and insulin resistance.
Exploring the Epigenetic Mechanisms
Epigenetic modifications, such as DNA methylation and histone modifications, can influence gene expression without altering the underlying DNA sequence. These modifications can be influenced by environmental factors, lifestyle choices, and even stress. Future research should investigate the role of epigenetic factors in mediating the link between insulin, diet, and weight. Studies examining the epigenetic profiles of individuals with different weight statuses and insulin sensitivities could reveal potential biomarkers for early detection and targeted interventions.
Developing Personalized Interventions
Recognizing the diversity in individual responses to interventions is crucial. Future research should move towards personalized approaches to weight management and insulin resistance prevention. This includes developing predictive models that identify individuals at high risk for developing insulin resistance based on their genetic predispositions, lifestyle factors, and gut microbiome profiles. These models could then be used to tailor interventions, such as dietary recommendations, exercise regimens, and pharmacological strategies, to maximize effectiveness.
This approach is already evident in cancer treatment and could be equally beneficial in managing metabolic disorders.
Addressing the Challenges in Research
Conducting research on insulin, weight, and related factors presents several challenges. These include the complexity of the human metabolic system, the difficulty in isolating specific factors, and the ethical considerations associated with long-term studies. Furthermore, the cost of advanced technologies like metagenomic sequencing and sophisticated modeling can pose a barrier to progress. Robust and longitudinal studies are needed to adequately address these complexities.
Potential Implications for Insulin Resistance and Weight Management
Advancements in understanding the mechanisms linking insulin, weight, and related factors will have significant implications for insulin resistance and weight management. This knowledge can lead to the development of more targeted and effective interventions, reducing the risk of developing chronic diseases associated with these conditions. Improved understanding of the intricate interactions between diet, lifestyle, and the human metabolic system may lead to more personalized and sustainable weight management strategies.
For example, individuals at risk of developing insulin resistance could receive personalized dietary recommendations and lifestyle modifications to prevent disease progression.
Last Word
In conclusion, the relationship between insulin and weight gain is a multifaceted one, far beyond a simple yes or no answer. Insulin’s role in regulating blood sugar and influencing fat storage is undeniable. However, lifestyle factors, genetics, and overall health significantly impact how insulin functions in the body. The key takeaway is that a balanced approach involving diet, exercise, and potentially medical interventions is crucial for managing weight and maintaining overall health.
Understanding the nuances of this relationship is essential for individuals seeking to manage their weight effectively.

Leave a Reply