What causes bladder infections? This common issue affects many, and understanding its root causes is key to prevention and treatment. From bacteria to personal habits, a range of factors contribute to the development of urinary tract infections (UTIs). This in-depth exploration dives into the various culprits behind bladder infections, covering bacterial, host, and environmental influences. We’ll explore the role of bacteria, individual risk factors, and lifestyle choices in triggering these infections.
The urinary system is a complex network, and its delicate balance can easily be disrupted. Understanding how these infections develop is crucial for maintaining good health. This blog post will walk you through the various factors that contribute to bladder infections, shedding light on everything from bacterial colonization to hygiene practices and beyond. We will explore the specific mechanisms and conditions that make some individuals more prone to these infections, providing a comprehensive overview for better awareness and proactive care.
Introduction to Urinary Tract Infections (UTIs)
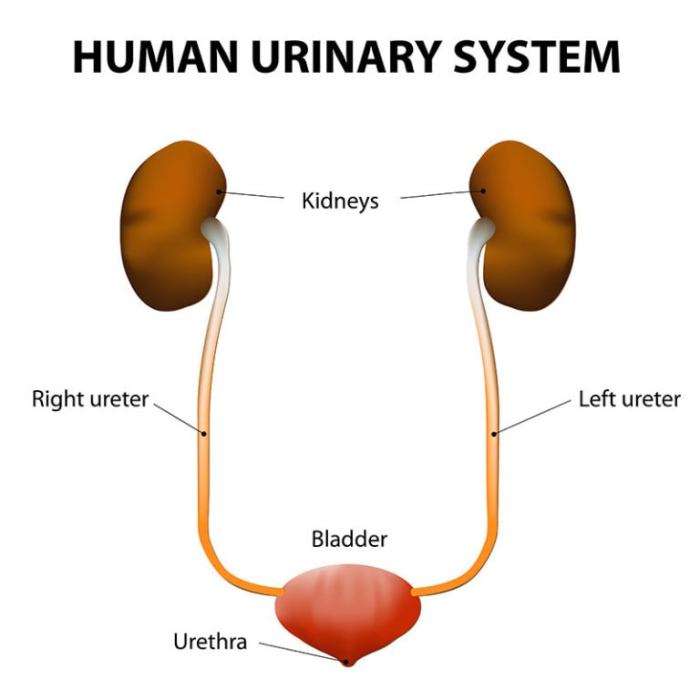
A urinary tract infection (UTI) is a bacterial infection that affects any part of the urinary system. A bladder infection, specifically, is an infection of the bladder, the organ that stores urine. These infections are quite common, affecting millions worldwide, and often present with easily recognizable symptoms. Understanding the urinary system and the symptoms of a UTI can help individuals recognize and seek appropriate treatment.The urinary system plays a vital role in eliminating waste from the body.
Its primary components filter blood, collect urine, and expel it from the body. A healthy urinary system functions seamlessly, preventing infection. However, disruptions in this process can create an environment conducive to bacterial growth, leading to infections.
Anatomy of the Urinary Tract (Focus on the Bladder)
The urinary tract is a complex system, including the kidneys, ureters, bladder, and urethra. The bladder is a hollow, muscular organ situated in the lower abdomen. Its primary function is to store urine temporarily until it’s expelled from the body. The bladder’s walls are lined with specialized tissues that stretch and contract to accommodate varying urine volumes.
The ability to hold urine is crucial for normal bodily function. The bladder’s smooth muscle layers contract to release urine through the urethra.
Normal Function of the Urinary System
The kidneys filter waste products from the blood, producing urine. The urine travels through the ureters, narrow tubes connecting the kidneys to the bladder. The bladder stores the urine until urination occurs. During urination, the bladder muscles contract, forcing urine through the urethra and out of the body. The normal flow of urine is essential to prevent bacterial buildup and infection.
Common Types of UTIs
| Type of UTI | Description |
|---|---|
| Cystitis | Cystitis is a bacterial infection of the bladder. It is the most common type of UTI. |
| Pyelonephritis | Pyelonephritis is a more serious infection that involves the kidneys. It typically develops when a bladder infection spreads upward. |
This table contrasts cystitis and pyelonephritis, highlighting the location of the infection. Understanding these distinctions is vital for appropriate treatment.
Symptoms of a Bladder Infection
A bladder infection often presents with a range of symptoms. Common signs include frequent urination, a strong urge to urinate, and pain or burning sensation during urination. The pain can be localized to the lower abdomen or pelvic area. In some cases, blood in the urine (hematuria) might be observed. These symptoms, while often uncomfortable, are usually manageable with timely intervention.Frequent urination, also known as pollakiuria, is a common symptom.
Bladder infections, often annoying and uncomfortable, are usually caused by bacteria entering the urinary tract. Interestingly, while seemingly unrelated, some research suggests that a severe blow to the head, like those causing coup contrecoup brain injuries , can sometimes disrupt nerve signals affecting bladder control, potentially increasing the risk of infection. This is a complex area of study, but it highlights how interconnected our bodies are.
Ultimately, the most common culprits for bladder infections remain bacteria, so proper hygiene is key.
Patients may feel the need to urinate more frequently than usual.Urgency is characterized by a sudden and intense urge to urinate. This symptom can be quite distressing, causing individuals to seek immediate relief.Pain or burning during urination, often described as dysuria, is another prominent symptom. This discomfort can vary in intensity, ranging from mild to severe.Blood in the urine (hematuria) is a less common but significant symptom.
It indicates potential damage to the urinary tract. Any blood in the urine warrants immediate medical attention to rule out more serious conditions.
Causes of Bladder Infections
Bladder infections, or UTIs, are a common health concern affecting millions worldwide. Understanding the causes is crucial for prevention and effective treatment. A key element in managing these infections is recognizing the factors that increase susceptibility. This knowledge empowers individuals to take proactive steps towards avoiding UTIs.
Common Bacterial Culprits
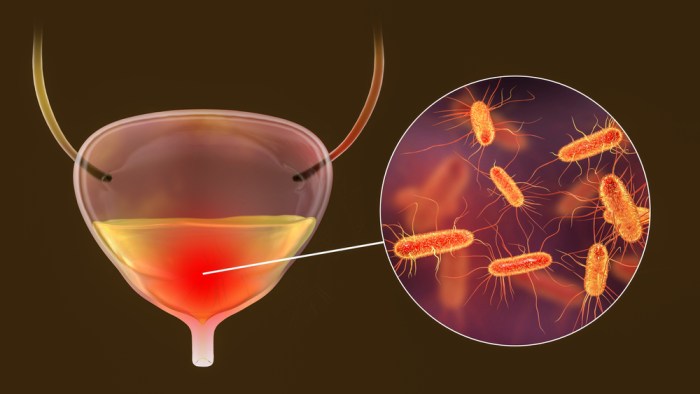
The most frequent culprits behind bladder infections are bacteria, specifically
- Escherichia coli* (E. coli). This bacterium naturally resides in the gut and can easily enter the urinary tract. Other less common bacterial causes include
- Staphylococcus saprophyticus* and various types of
- Enterococcus*. The specific bacteria involved can influence treatment approaches, making accurate identification vital.
Risk Factors for Bladder Infections: A Comparative Analysis
Several factors increase the risk of developing a bladder infection. Some risk factors are more prevalent in certain populations than others. Understanding these differences can help tailor preventive measures.
- Age: Children and older adults are more susceptible due to developmental differences in urinary tract structure and function in children and the increased prevalence of underlying health conditions in older adults. For example, in children, incompletely developed urinary tracts can hinder proper flushing, making them more prone to infection. In older adults, conditions like diabetes and weakened immune systems can make them more susceptible.
- Gender: Women are more prone to UTIs due to the shorter urethra in women. This shorter distance allows bacteria to reach the bladder more easily. This anatomical difference, coupled with other factors like sexual activity, contributes to the higher incidence rate in women.
- Sexual Activity: Sexual activity can introduce bacteria into the urethra, increasing the risk of infection. The friction involved can disrupt the natural balance of bacteria in the area. Sexual intercourse can potentially disrupt the normal flora, making women more susceptible to infection. Proper hygiene practices, like wiping front to back after urination, are essential.
- Hygiene Practices: Inadequate hygiene practices, such as improper wiping after urination, can introduce bacteria into the urinary tract. For example, wiping back to front can spread fecal bacteria to the genital area, increasing the risk of infection.
Bacterial Colonization of the Urinary Tract
Bacteria can colonize the urinary tract through various routes. The most common pathway is ascending, where bacteria from the external environment enter the urethra and travel upward to the bladder. This process can be facilitated by factors such as sexual activity or inadequate hygiene.
The ascending route is the most common mechanism by which bacteria reach the bladder.
Proper hygiene and maintaining a healthy urinary tract environment are vital to prevent bacterial colonization.
Preventing Bladder Infections: Practical Strategies
Proactive measures can significantly reduce the risk of bladder infections. These measures include maintaining good hygiene, drinking plenty of fluids, and promptly addressing any urinary symptoms.
- Hydration: Drinking plenty of water helps flush bacteria out of the urinary tract, diluting the urine and making it less hospitable for bacteria to thrive. This helps to maintain a healthy urinary tract environment.
- Hygiene: Maintaining proper hygiene practices, especially after urination, is essential. Wiping from front to back after urination can prevent fecal bacteria from entering the urethra. This can prevent bacterial entry into the urinary tract, thus reducing the risk of infection.
- Avoiding Irritants: Certain products, like scented soaps or detergents, can irritate the urinary tract, increasing the risk of infection. Avoiding these products can help to prevent discomfort and reduce the risk of infection.
Risk Factors and Potential Impact on Infection
| Risk Factor | Potential Impact |
|---|---|
| Age (young children, older adults) | Immature or weakened immune systems, anatomical differences |
| Gender (women) | Shorter urethra, increased exposure to bacteria |
| Sexual Activity | Introduction of bacteria into the urethra |
| Hygiene Practices | Inadequate hygiene allowing bacterial entry |
| Underlying Health Conditions | Diabetes, weakened immune system increasing vulnerability |
Bacterial Factors
Understanding the specific characteristics of bacteria responsible for urinary tract infections (UTIs) is crucial for effective prevention and treatment. These bacteria, often residing in the gut flora, can gain access to the urinary tract and establish infections under certain circumstances. Their ability to adhere, evade the immune system, and produce virulence factors all contribute to the development of the infection.
Bladder infections, a common annoyance, are often caused by bacteria entering the urinary tract. Interestingly, certain health conditions, like type 1 vs type 2 diabetes , can increase the risk of these infections due to changes in the body’s immune response. This highlights how interconnected various health issues can be, even when seemingly unrelated. So, while the primary culprit is usually bacteria, underlying conditions can definitely play a role.
Bacterial Characteristics
Urinary tract infections are primarily caused by a select group of bacteria. The most common culprit is
- Escherichia coli* (E. coli), often found in the gut. Other bacteria, such as
- Staphylococcus saprophyticus*,
- Klebsiella pneumoniae*, and
- Proteus mirabilis*, can also cause UTIs. These bacteria possess unique traits that allow them to thrive in the urinary tract and cause infections. The presence of specific virulence factors, which are produced by the bacteria, plays a critical role in establishing the infection.
Adherence Mechanisms
Bacteria need to attach themselves to the urinary tract lining to establish a foothold. This adherence is mediated by specialized structures, called adhesins, that bind to specific receptors on the cells of the urinary tract. The exact receptors and adhesins involved vary depending on the bacterial species. For example,E. coli* often uses fimbriae, hair-like appendages, to bind to the uroepithelial cells lining the urinary tract.
These adhesins can help the bacteria to resist flushing and other natural defenses, enabling them to persist within the urinary tract.
Immune Evasion Strategies
The host’s immune system actively tries to eliminate the invading bacteria. However, certain bacteria have developed mechanisms to evade these defenses. Some bacteria produce substances that inhibit the complement system, a crucial part of the immune response. Others modify their surface structures to prevent recognition by immune cells. These strategies allow the bacteria to survive and multiply in the urinary tract, ultimately causing infection.
One notable example is the production of capsules by certain bacteria, which act as a shield against phagocytosis, a process where immune cells engulf and destroy bacteria.
Bacterial Virulence Factors
Bacterial virulence factors are traits that enhance the ability of bacteria to cause disease. These factors can include toxins, enzymes, or other substances that damage host tissues or disrupt immune responses. Examples include hemolysins, which damage red blood cells, and cytotoxins, which harm host cells. These factors help bacteria to proliferate and spread, ultimately contributing to the severity of the infection.
The specific virulence factors present can vary between bacterial species and strains, affecting the disease’s outcome.
Antibiotic Resistance
Antibiotic resistance is a significant concern in the treatment of UTIs. The overuse and misuse of antibiotics have driven the selection and spread of antibiotic-resistant bacteria. This means that antibiotics that were once effective in treating these infections are no longer able to kill the bacteria, rendering the treatment ineffective. Consequently, alternative or more potent antibiotics need to be considered, increasing treatment costs and complexity.
Antibiotic Resistance Profiles
| Bacterial Type | Common Antibiotic Resistance Profiles |
|---|---|
| *Escherichia coli* | Often resistant to multiple antibiotics, including fluoroquinolones and some cephalosporins. |
| *Staphylococcus saprophyticus* | Often resistant to penicillin and ampicillin. |
| *Klebsiella pneumoniae* | Frequently resistant to several broad-spectrum antibiotics, including penicillins and cephalosporins. |
| *Proteus mirabilis* | May exhibit resistance to various antibiotics, including aminoglycosides and trimethoprim-sulfamethoxazole. |
This table provides a general overview, and specific resistance profiles can vary depending on the bacterial strain and geographical location. Further investigation and testing are often necessary to determine the precise antibiotic susceptibility of a particular bacterial isolate.
Bladder infections, a common annoyance, often stem from bacteria entering the urinary tract. While the exact culprits vary, poor hygiene plays a significant role. Sometimes, it’s related to other health issues, such as acid reflux, which can affect the throat and potentially lead to infections elsewhere in the body. For those seeking relief from acid reflux sore throat remedies, checking out this resource might be helpful acid reflux sore throat remedies.
However, it’s crucial to remember that the best way to address bladder infections is by consulting a doctor for proper diagnosis and treatment.
Host Factors
Beyond the bacterial culprits, a multitude of host factors play a crucial role in susceptibility to bladder infections. These factors, intrinsic to the individual, influence the body’s ability to defend against and clear infections. Understanding these elements is essential for developing preventative strategies and personalized treatment plans.Host factors encompass anatomical characteristics, the immune system’s response, pre-existing medical conditions, and even hygiene practices.
These interwoven elements can significantly impact an individual’s risk of contracting a urinary tract infection (UTI).
Anatomical Factors
Certain anatomical features can increase the risk of bladder infections. For instance, women have a shorter urethra than men, which allows bacteria easier access to the bladder. This anatomical difference makes women more susceptible to UTIs. Additionally, structural abnormalities in the urinary tract, such as obstructions or blockages, can impede the natural flow of urine, creating an environment conducive to bacterial growth.
Immune System Impact
The immune system’s ability to fight off infections is a key factor. Individuals with weakened immune systems, due to conditions like diabetes or HIV, are more prone to UTIs. The body’s natural defense mechanisms, including the flushing action of urine and the presence of immune cells in the urinary tract, are compromised in these cases. Furthermore, individuals with compromised immune systems often exhibit slower recovery times from infections.
Medical Conditions and UTI Risk
Certain medical conditions can significantly increase the likelihood of UTIs. For example, diabetes impairs the body’s ability to fight infection, making individuals more vulnerable. Neurological conditions, such as spinal cord injuries, can lead to urinary retention, creating a breeding ground for bacteria. Kidney stones can also obstruct urine flow, raising the risk.
| Medical Condition | Likelihood of UTI | Explanation |
|---|---|---|
| Diabetes | High | Impaired immune function, frequent urination, and elevated blood sugar levels contribute to the risk. |
| Neurological conditions (e.g., spinal cord injury) | High | Urinary retention, reduced bladder emptying, and impaired immune response. |
| Kidney stones | High | Obstruction of urine flow, allowing bacteria to accumulate. |
| Pregnancy | Moderate | Hormonal changes and pressure on the bladder increase risk. |
| Prostatitis | Moderate | Inflammation of the prostate can cause urinary retention and obstruction. |
Hygiene Practices, What causes bladder infections
Maintaining good hygiene plays a critical role in UTI prevention. Proper hygiene practices include regular urination, particularly after sexual activity, and maintaining clean perineal areas. Maintaining proper hydration by drinking plenty of fluids helps flush bacteria out of the urinary tract.
Demographic Differences in UTI Risk
Studies have shown variations in UTI risk across different demographic groups. Women are generally more susceptible than men due to anatomical differences. Elderly individuals are also at increased risk due to potential medical conditions and changes in urinary habits.
Environmental Factors: What Causes Bladder Infections
Bladder infections, or UTIs, aren’t just about bacteria; environmental conditions can play a significant role in their development. From personal hygiene practices to sexual activity, various external factors influence the risk of infection. Understanding these elements can help in proactive prevention strategies.Environmental factors encompass a broad range of conditions that can influence the likelihood of developing a UTI.
These factors interact with bacterial factors and host factors, creating a complex interplay that determines an individual’s susceptibility. Factors like water temperature, water quality, and exposure to certain chemicals can all affect the microbial balance within the urinary tract.
Sexual Activity and Practices
Sexual activity, particularly vaginal intercourse, can introduce bacteria into the urethra, increasing the risk of infection. Unprotected sex, or sex with multiple partners, can expose individuals to a broader range of bacteria and increase the likelihood of developing a UTI. Using barriers like condoms during sexual activity can significantly reduce the risk of introducing pathogens.
Personal Hygiene
Proper personal hygiene is crucial in preventing UTIs. Maintaining cleanliness in the genital area helps prevent the growth and spread of bacteria. Improper hygiene, including inadequate cleaning after urination or bowel movements, can create an environment conducive to bacterial colonization, potentially leading to infection. Regular and thorough cleansing with water and mild soap, along with paying attention to the cleanliness of underwear and bedding, is essential.
Sexual Orientation and Gender Identity
Sexual orientation and gender identity do not directly cause UTIs, but certain social and behavioral factors associated with these identities may influence UTI risk. For instance, stigma or discrimination can impact access to healthcare and sanitation, potentially increasing vulnerability. Cultural norms and societal expectations surrounding hygiene and sexual practices can also affect UTI risk.
Environmental Conditions
Environmental conditions, such as water quality and temperature, can influence the presence and activity of certain bacteria. Water contaminated with bacteria can contribute to the risk of infection. The temperature of the water can affect the bacterial growth rates.
Impact of Different Environmental Factors on UTI Occurrence
| Environmental Factor | Impact on UTI Occurrence | Example |
|---|---|---|
| Sexual Activity (unprotected) | Increased risk due to introduction of bacteria. | Sexual intercourse without barrier protection. |
| Poor Personal Hygiene | Increased risk due to bacterial colonization. | Insufficient cleansing after urination or bowel movements. |
| Contaminated Water | Increased risk due to introduction of bacteria. | Swimming in water with high bacterial content. |
| Stress and Mental Health | Potentially increased risk due to weakened immune system. | Chronic stress can impact immune function. |
Diagnosis and Treatment
Bladder infections, while often treatable, require prompt and accurate diagnosis to ensure effective treatment and prevent complications. Proper identification of the causative bacteria and a tailored treatment plan are crucial for a speedy recovery and a reduction in the risk of recurrence. This section delves into the diagnostic procedures, treatment options, and the importance of completing the prescribed course of antibiotics.Accurate diagnosis and appropriate treatment are vital to prevent potential complications.
Misdiagnosis or incomplete treatment can lead to more serious health issues.
Diagnostic Procedures for UTIs
Diagnosis of a urinary tract infection (UTI) typically begins with a thorough medical history and physical examination. A key part of this process involves collecting a urine sample for laboratory analysis.
- Urine Tests: A urinalysis, a simple test that examines the physical and chemical properties of the urine, is often the first step. A cloudy appearance, abnormal color, or the presence of blood or pus can suggest an infection. Further investigation may include a urine culture. This test identifies the specific bacteria causing the infection, crucial for selecting the most effective antibiotic.
Treatment Options for Bladder Infections
Effective treatment for bladder infections hinges on identifying the causative bacteria and prescribing the most appropriate antibiotic.
- Antibiotics: Antibiotics are the cornerstone of UTI treatment. The choice of antibiotic depends on the results of the urine culture, as well as the individual patient’s medical history. Common antibiotics used to treat UTIs include trimethoprim/sulfamethoxazole (TMP/SMZ), nitrofurantoin, and fluoroquinolones. These drugs work by targeting and killing the bacteria causing the infection.
Importance of Completing the Full Course of Antibiotics
Failure to complete the full course of antibiotics can lead to treatment failure and potential antibiotic resistance.
- Completing the Course: Even if symptoms improve, it is crucial to finish the entire prescribed course of antibiotics. This ensures that all the bacteria are eradicated, preventing the infection from recurring or developing into a more severe condition. Not completing the full course can lead to persistent infection and antibiotic resistance.
Potential Complications of Untreated UTIs
Left untreated, UTIs can progress to more serious complications.
- Complications: Untreated UTIs can spread to the kidneys, causing pyelonephritis, a serious kidney infection. In severe cases, this can lead to sepsis, a life-threatening condition. Untreated UTIs can also cause chronic pain and discomfort.
Diagnostic Tests and Their Implications
The table below Artikels various diagnostic tests and their implications in diagnosing UTIs.
| Test | Description | Implications |
|---|---|---|
| Urinalysis | Examination of urine for physical characteristics (color, clarity) and chemical components (pH, presence of blood, protein, glucose). | Indicates possible infection if abnormal findings are present, but not definitive. |
| Urine Culture | Cultivation of urine sample to identify causative bacteria. | Provides the specific bacterial identification for targeted antibiotic treatment and prevents inappropriate antibiotic use. |
| Urine Microscopy | Microscopic examination of urine to identify presence of white blood cells and bacteria. | Provides evidence of infection and the level of infection. |
Antibiotic Treatments for UTIs
The table below compares various antibiotic treatments for UTIs.
| Antibiotic | Mechanism of Action | Advantages | Disadvantages |
|---|---|---|---|
| Trimethoprim/Sulfamethoxazole (TMP/SMZ) | Inhibits bacterial growth by interfering with DNA synthesis. | Effective against a wide range of bacteria, often a first-line treatment. | Potential side effects like nausea, rash, and allergic reactions. |
| Nitrofurantoin | Interferes with bacterial cell function. | Effective against some bacteria, often used for uncomplicated UTIs. | Can cause gastrointestinal upset. |
| Fluoroquinolones | Inhibit bacterial DNA replication. | Effective against a broad range of bacteria, often a good choice for complicated infections. | Potential side effects like tendon rupture, and risk of central nervous system effects. Should be used with caution in certain populations. |
Final Review
In conclusion, what causes bladder infections is a multifaceted question with a variety of contributing factors. While bacteria are often the primary culprit, individual predispositions, lifestyle choices, and environmental elements play crucial roles. Understanding these intricate connections empowers individuals to take proactive steps toward prevention. From practicing good hygiene to recognizing personal risk factors, this knowledge is invaluable in safeguarding your urinary health.
By combining awareness and preventative measures, you can significantly reduce your susceptibility to bladder infections.










