The Functional Independence Measurement (FIM) is a crucial tool in healthcare, providing a standardized way to assess a patient’s ability to perform daily tasks. From the initial stages of rehabilitation to discharge planning, the FIM plays a vital role in evaluating progress and tailoring treatment strategies. Understanding its components, scoring system, and applications is key to grasping its impact on patient outcomes.
This exploration delves into the FIM’s historical context, practical applications, and potential limitations, providing a comprehensive overview of this significant assessment tool.
This article explores the different aspects of the FIM, from its definition and purpose to the various ways it’s used in different healthcare settings. We’ll examine the detailed scoring system, the administration process, and the considerations for diverse patient populations. The discussion also touches upon the FIM’s strengths and weaknesses, comparing it to other assessment tools and highlighting its role in patient rehabilitation and discharge planning.
Introduction to the Functional Independence Measurement (FIM)
The Functional Independence Measurement (FIM) is a standardized assessment tool used extensively in healthcare settings to evaluate a patient’s ability to perform various activities of daily living (ADLs). It provides a quantitative measure of a patient’s functional status, facilitating comparisons across different patients and over time. This detailed evaluation is crucial for therapists and clinicians to track progress and tailor rehabilitation plans effectively.The FIM is widely applied in a multitude of healthcare contexts, including rehabilitation facilities, hospitals, and skilled nursing facilities.
Its objective nature makes it a valuable tool for documenting functional changes, monitoring treatment efficacy, and assessing the impact of interventions. Its comprehensive nature allows for a holistic view of a patient’s functional abilities, informing decisions about discharge planning and further care.
FIM Component Breakdown
The FIM assesses a wide range of functional abilities, categorized into specific components. This comprehensive approach enables a detailed picture of the patient’s overall functional status. The following table Artikels the key components and provides illustrative examples:
| FIM Component | Description | Example of Use |
|---|---|---|
| Self-Care | Activities related to personal hygiene and dressing. | Bathing, dressing, grooming, toileting. |
| Sphincter Control | Management of bowel and bladder functions. | Independent voiding, bowel management, using the toilet independently. |
| Mobility | Movement within the environment, including transfers and ambulation. | Getting in and out of bed, transferring from a chair, walking independently. |
| Communication | Verbal and nonverbal interaction. | Speaking, understanding spoken language, using assistive communication devices. |
| Social Cognition | Interactions with others, including comprehension of social cues and expressions. | Participating in group therapy, interacting with family members, responding appropriately to social situations. |
| Problem Solving | Cognitive skills involved in completing tasks and making decisions. | Managing medication, understanding instructions, performing tasks with planning. |
Historical Context of the FIM
The FIM’s development stemmed from the need for a standardized method to assess functional abilities across diverse patient populations. Initially, various, non-standardized methods were used to evaluate functional outcomes, leading to inconsistent and difficult-to-compare results. The FIM emerged as a solution, aiming to create a more objective and reliable assessment tool. Its evolution reflects the growing recognition of the importance of functional outcomes in healthcare.
Early versions of the FIM underwent extensive testing and refinement to ensure its reliability and validity. This iterative process resulted in the comprehensive and widely used instrument it is today.
The Functional Independence Measurement (FIM) is a great tool for assessing a patient’s ability to perform daily tasks. It’s particularly important in evaluating recovery after a stroke, where factors like diabetes can significantly impact functional independence. For instance, understanding the interplay between stroke and diabetes is crucial for tailoring rehabilitation plans, as detailed in this informative article on the stroke and diabetes connection.
Ultimately, the FIM helps healthcare providers create personalized plans to maximize a patient’s independence and quality of life after a stroke or other conditions.
Components and Scoring of the FIM
The Functional Independence Measurement (FIM) is a valuable tool for assessing the functional abilities of individuals, particularly those recovering from illness or injury. Understanding the different components and their scoring systems is crucial for accurate interpretation and effective treatment planning. This detailed look at the FIM’s structure will clarify how it measures independent functioning in various activities.The FIM provides a comprehensive evaluation of a patient’s ability to perform daily living activities.
The Functional Independence Measurement (FIM) is a crucial tool for assessing a person’s ability to perform everyday tasks. It’s important to explore different approaches to maintaining independence, like the Wahls Protocol, for managing MS symptoms. This protocol, which focuses on dietary changes and lifestyle adjustments, could significantly impact your functional abilities. For more information on the benefits of the Wahls Protocol specifically for MS, check out this insightful article: reasons to try the wahls protocol for ms.
Ultimately, understanding and improving your functional independence is key to maintaining a high quality of life.
It’s designed to quantify the level of assistance needed for each task, ranging from complete independence to needing maximum assistance. This allows clinicians to track progress and tailor interventions to meet individual needs.
FIM Sections
The FIM is organized into several sections, each evaluating a specific set of activities. Understanding the distinct domains covered by the FIM is essential to interpret the assessment accurately. These sections cover a wide spectrum of functional skills, from basic self-care to complex mobility tasks.
- Self-Care: This section assesses the patient’s ability to perform personal care tasks like bathing, dressing, and eating. It includes grooming and toileting.
- Sphincter Control: This section focuses on the patient’s ability to control bowel and bladder function, including managing incontinence.
- Mobility: This section covers the patient’s ability to move around, including getting in and out of bed, walking, and using stairs. It encompasses the use of assistive devices like wheelchairs.
- Communication: This section evaluates the patient’s ability to communicate effectively, including verbal and nonverbal communication. It assesses the ability to express needs and understand instructions.
- Social Cognition: This section measures the patient’s ability to interact appropriately with others, including social cues and interactions. It evaluates how they perceive and respond to social situations.
Scoring System
Each section of the FIM uses a standardized scoring system to quantify the level of assistance required. The system typically ranges from 0 (maximum assistance) to 7 (complete independence).
| Score | Level of Assistance | Examples |
|---|---|---|
| 0 | Maximum Assistance | Complete assistance required from another person for the task. |
| 1 | Requires Supervision | Requires supervision and/or close monitoring for safety. |
| 2 | Moderate Assistance | Patient performs part of the task, but significant assistance is needed. |
| 3 | Moderate Supervision | Patient performs a significant portion of the task but needs assistance for safety or completion. |
| 4 | Minimal Assistance | Minimal assistance is needed to complete the task. |
| 5 | Supervision | Requires verbal cues or supervision but can complete the task mostly independently. |
| 6 | Modified Independence | Requires the use of assistive devices or adaptations. |
| 7 | Complete Independence | Patient performs the task completely independently without any assistance. |
Sample FIM Assessment, The functional independence measurement
A sample FIM assessment might show the following scores:
- Self-Care: 6 (Modified Independence)
- Sphincter Control: 7 (Complete Independence)
- Mobility: 5 (Supervision)
- Communication: 7 (Complete Independence)
- Social Cognition: 6 (Modified Independence)
This demonstrates a patient who is mostly independent in self-care and communication but requires supervision for mobility. The patient has complete control over their bowel and bladder function.
Calculating the FIM Total Score
The total FIM score is calculated by summing the scores across all sections. For example, with the scores above:
Total FIM = 6 + 7 + 5 + 7 + 6 = 31
The total score provides a general indication of the patient’s overall functional independence.
Administration and Interpretation of the FIM
The Functional Independence Measurement (FIM) is a crucial tool for assessing a patient’s functional abilities and guiding their rehabilitation. Proper administration and interpretation are vital to ensure accurate and reliable results, enabling clinicians to tailor interventions effectively and track progress objectively. This section delves into the practical aspects of administering and interpreting the FIM, highlighting considerations for diverse patient populations.The FIM assessment process is designed to be standardized, allowing for comparison across different settings and individuals.
It focuses on observing and documenting a patient’s performance in a range of activities of daily living (ADLs) and mobility tasks. Understanding the procedures, the assessor’s role, and population-specific considerations is key to obtaining meaningful results.
FIM Assessment Procedure
The FIM assessment typically involves a trained professional observing the patient’s performance in various tasks. The assessor should be familiar with the specific scoring criteria for each task. The assessment environment should be conducive to the patient’s comfort and ability to perform the tasks. Prior to the assessment, the assessor should ensure the necessary equipment is available.
Detailed documentation of the patient’s performance is critical, including any observed limitations, adaptations, or assistive devices used.
Assessor’s Role in the FIM Process
The assessor plays a pivotal role in the FIM assessment. They are responsible for accurately observing and documenting the patient’s performance, ensuring a standardized approach across assessments. Their understanding of the scoring criteria is paramount to accurate evaluation. Furthermore, the assessor should provide a supportive and encouraging environment to help the patient feel comfortable and perform to their best ability.
Their observation should also note any environmental factors that might influence the patient’s performance.
Considerations for Different Patient Populations
Different patient populations require specific considerations during the FIM assessment. For example, patients with cognitive impairments may require modifications to the assessment, potentially including simplification of instructions or alternative methods of communication. Patients with physical limitations may require assistive devices or adjustments in the environment. Cultural sensitivities and communication barriers must also be considered, and the assessor should be mindful of potentially influencing factors.
Comparison of Assessment Approaches
| Assessment Approach | Description | Strengths | Limitations |
|---|---|---|---|
| Direct Observation | Assessor directly observes the patient performing the task. | High reliability, allows for detailed observation of technique. | May be time-consuming, potential for bias from observer. |
| Self-Report | Patient reports their ability to perform the task. | Can be useful for certain tasks, less time-consuming. | Susceptible to recall bias, may not accurately reflect true ability. |
| Combination of Observation and Self-Report | Combines direct observation with self-report. | Maximizes information, mitigates bias. | More complex to administer and interpret. |
Scoring Criteria for Each Task
Correct scoring of each task is crucial for accurate FIM interpretation. The FIM manual provides detailed descriptions of the specific criteria for each task, including the level of assistance required. Assessor training is critical to ensuring consistency in scoring across various settings. For example, for the “Transfers” section, scores are given based on the degree of assistance required (e.g., “Independent” means the patient can perform the transfer unaided, while “Total Assistance” means the patient requires complete assistance from another person).
Applications and Uses of the FIM
The Functional Independence Measurement (FIM) is more than just a scoring system; it’s a powerful tool used across various healthcare settings to understand and track a patient’s progress during rehabilitation. Its ability to quantify functional abilities allows for objective assessments, facilitating better patient care planning and outcomes. This detailed look at the FIM’s applications will illuminate its versatility in measuring independence, guiding rehabilitation, and improving patient discharge planning.The FIM’s versatility stems from its comprehensive approach to evaluating functional abilities.
By measuring performance across multiple areas, the FIM provides a holistic picture of a patient’s recovery journey. This holistic perspective allows healthcare professionals to tailor interventions and support systems that are precisely aligned with the patient’s individual needs. This enables more effective and efficient rehabilitation strategies, leading to better outcomes and quicker recovery times.
Measuring Functional Abilities
The FIM meticulously assesses a patient’s abilities in 18 specific tasks, categorized into motor and cognitive skills. This detailed evaluation allows healthcare providers to understand the extent of a patient’s functional independence. The scoring system provides a quantifiable measure of a patient’s progress, allowing for comparison across different patients and over time. This consistent measurement provides valuable data for tracking recovery and evaluating the effectiveness of treatment plans.
Role in Patient Rehabilitation Planning
The FIM plays a pivotal role in developing personalized rehabilitation plans. By identifying areas of weakness and strength, the FIM helps to tailor interventions to address specific needs. For instance, if a patient demonstrates difficulty with mobility, the rehabilitation plan can include exercises and therapies focused on improving that specific area. The FIM’s data-driven approach ensures that interventions are targeted and effective, ultimately maximizing the patient’s potential for recovery.
Furthermore, the FIM’s continuous monitoring throughout the rehabilitation process helps in adjusting the plan as needed, ensuring optimal outcomes.
Areas of Healthcare Use
The FIM is widely used in various healthcare settings, including inpatient rehabilitation facilities, hospitals, skilled nursing facilities, and outpatient clinics. Its applicability across diverse healthcare settings makes it a valuable tool for understanding and managing patients’ functional capabilities. Its adaptability allows for its use in various patient populations and clinical scenarios, promoting consistent standards of care and patient-centered approaches.
Discharge Planning
FIM data is crucial in discharge planning. The comprehensive evaluation of a patient’s functional abilities enables healthcare professionals to determine the appropriate level of support needed after discharge. This assessment allows for the identification of potential challenges and the development of strategies to address them. The FIM’s quantifiable data facilitates communication between healthcare providers and the patient’s family or caregiver, ensuring a smooth transition back to home.
This facilitates coordination of care and reduces the risk of readmission.
Examples of Application in Healthcare Settings
Consider a patient recovering from a stroke. The FIM can be used to assess the patient’s ability to perform activities of daily living (ADLs), such as eating, dressing, and transferring. The FIM data can be used to inform the development of a rehabilitation plan that includes exercises to improve motor skills, occupational therapy for ADLs, and speech therapy to address communication difficulties.Another example involves a patient with a spinal cord injury.
The FIM can be used to measure the patient’s functional independence in activities such as mobility, self-care, and communication. The FIM’s data can inform the development of a plan that includes assistive devices, adaptive equipment, and vocational training. This personalized approach to rehabilitation is possible due to the detailed assessment of the FIM.
FIM Use in Different Clinical Contexts
| Clinical Context | FIM Use |
|---|---|
| Inpatient Rehabilitation | Assessing functional abilities, guiding rehabilitation plans, tracking progress |
| Hospital Discharge Planning | Determining appropriate level of support after discharge, facilitating communication |
| Skilled Nursing Facilities | Evaluating functional status, developing individualized care plans |
| Outpatient Clinics | Monitoring progress, assessing effectiveness of therapies |
Limitations and Criticisms of the FIM
The Functional Independence Measurement (FIM) is a widely used tool for assessing and measuring functional abilities. However, like any assessment tool, it has limitations and criticisms that need careful consideration. Understanding these aspects allows for a more nuanced application of the FIM and a more complete picture of a patient’s functional status.
Potential Limitations of the FIM
The FIM relies heavily on the observer’s interpretation and judgment. Variations in how different therapists administer and score the FIM can lead to inconsistencies in results. Furthermore, the FIM’s focus on observable behaviors may not fully capture the complexities of an individual’s functional abilities. For instance, a patient might be able to perform a task independently but with significant effort, a factor the FIM may not adequately reflect.
Cultural and environmental factors can also influence performance, potentially affecting the accuracy of the FIM assessment.
Criticisms of the FIM’s Scoring System
Some critics argue that the FIM’s scoring system lacks sensitivity for subtle differences in performance. The scoring categories may not adequately distinguish between different levels of independence, especially in individuals with mild or moderate disabilities. Furthermore, the FIM’s reliance on a standardized set of tasks might not be appropriate for all patients. Certain patients may require alternative tasks that are more relevant to their specific needs or environments.
The scoring system may not be sensitive to the patient’s overall effort or strategies used in performing the task.
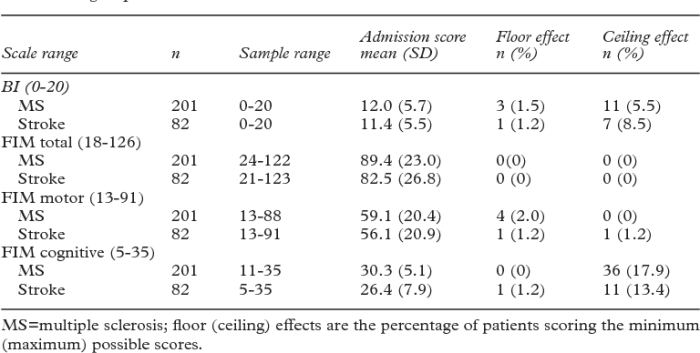
Comparison to Alternative Assessment Tools
Several alternative assessment tools exist, each with its own strengths and weaknesses. The Barthel Index, for example, focuses primarily on activities of daily living, while the Modified Barthel Index provides a more detailed assessment of specific activities. The FIM, while comprehensive, may not capture the nuances of performance that these alternative tools address. The choice of tool should depend on the specific needs of the assessment.
Situations Where the FIM Might Not Be Suitable
The FIM may not be the ideal assessment tool in certain situations. For example, individuals with cognitive impairments might find it difficult to perform tasks as expected, and the FIM’s reliance on motor skills may not adequately reflect their functional abilities. Furthermore, patients with severe communication difficulties may be assessed inaccurately due to misinterpretations of their responses.
Strengths and Weaknesses of the FIM
| Aspect | Strengths | Weaknesses |
|---|---|---|
| Objectivity | Provides a standardized and objective measure of functional ability. | Reliance on observation can introduce inter-rater variability. |
| Comprehensive | Assesses a wide range of functional skills. | May not be sensitive enough to subtle differences in performance. |
| Ease of Administration | Relatively easy to administer and score. | Limited sensitivity to cognitive or communication impairments. |
| Wide Applicability | Applicable to a variety of patient populations. | May not capture the complexities of functional performance for specific populations. |
| Standardization | Established norms allow for comparisons across different settings. | Standardized tasks may not be appropriate for all patients. |
Relationship between the FIM and Other Measures: The Functional Independence Measurement

The Functional Independence Measurement (FIM) is a valuable tool for assessing functional abilities, but its utility is often enhanced by incorporating other assessment methods. Understanding the relationships between the FIM and other measures allows for a more comprehensive picture of a patient’s recovery and progress. This section delves into comparisons with similar tools, highlights overlaps and differences, and explores the advantages of using the FIM alongside other outcome measures.Comparing the FIM to other functional assessment tools reveals both similarities and divergences in their approaches.
While many tools focus on specific aspects of function, the FIM provides a broader, more encompassing view of a patient’s independence in various activities. This holistic approach allows for a more nuanced evaluation of recovery trajectories, as opposed to isolated measures of a specific skill.
Comparison to Similar Functional Assessment Tools
Various functional assessment tools exist, each with its own strengths and limitations. The FIM often overlaps with tools like the Barthel Index, the Modified Barthel Index, and the Katz Activities of Daily Living Scale. These measures also evaluate functional abilities, but their scope and emphasis may differ. For example, the Barthel Index primarily focuses on activities of daily living (ADLs), while the FIM encompasses a wider range of motor and cognitive skills.
The Katz Scale, in contrast, focuses more specifically on basic ADLs.
Overlap and Differences Between the FIM and Other Measures
The FIM and other measures often share overlapping components. For instance, both the FIM and the Barthel Index assess self-care abilities, mobility, and communication. However, the FIM’s more detailed breakdown of tasks within each area allows for a more precise evaluation of a patient’s independence level. Differences arise in the level of detail, the specific activities included, and the weighting assigned to various tasks.
Correlation Between the FIM and Other Outcome Measures
A direct correlation exists between the FIM and other outcome measures, particularly in assessing rehabilitation progress. A higher FIM score generally corresponds to improved function and better outcomes in other domains. However, the degree of correlation can vary depending on the specific measures used and the population being studied.
Table Demonstrating Correlation
| Outcome Measure | Correlation with FIM | Description |
|---|---|---|
| Barthel Index | High | Measures basic ADLs. A strong correlation exists as both tools assess functional independence. |
| Katz Activities of Daily Living Scale | Moderate | Focuses on basic ADLs. Correlation is moderate as the scope differs slightly. |
| Glasgow Coma Scale | Low | Assesses level of consciousness. Correlation is low as these tools measure different aspects of function. |
| Patient Reported Outcome Measures (PROMs) | Moderate to High | Focus on the patient’s subjective experience of their condition and function. A moderate to high correlation exists when the PROMs address similar domains as the FIM. |
Advantages of Using the FIM in Conjunction with Other Measures
Using the FIM in conjunction with other measures offers several advantages. It provides a more comprehensive view of a patient’s recovery, as the FIM addresses a broader spectrum of functional abilities than other tools might. This comprehensive approach can also facilitate more precise assessments of individual needs and tailor rehabilitation programs. Furthermore, the combined use of multiple measures can increase the reliability and validity of the overall evaluation.
The Functional Independence Measurement (FIM) assesses a person’s ability to perform daily tasks. While it focuses on broader functional abilities, it’s important to consider specific issues like skin irritation and diarrhea, which can significantly impact a person’s independence. For example, managing skin irritation and diarrhea can be crucial for someone’s ability to maintain hygiene and mobility, which are key components of the FIM.
Check out these helpful tips on tips treating skin irritation diarrhea to see how these issues relate to overall functional independence.
For example, combining the FIM with patient-reported outcomes (PROMs) provides a richer understanding of the impact of functional limitations on the patient’s quality of life.
Trends and Future Directions of the FIM
The Functional Independence Measurement (FIM) has been a cornerstone of rehabilitation assessment for decades, consistently demonstrating its value in quantifying functional abilities. However, like any assessment tool, the FIM is subject to ongoing evolution and refinement, adapting to the ever-changing landscape of healthcare and research. This section explores the trajectory of the FIM, examining current research and potential future developments.The FIM’s enduring popularity stems from its comprehensive approach to measuring functional independence across multiple domains.
Its ability to track progress, evaluate treatment efficacy, and inform resource allocation has made it a vital tool in rehabilitation settings. This article dives into the future of the FIM, discussing potential improvements and areas for further development.
Evolution of the FIM
The FIM has undergone several revisions and adaptations since its inception. These revisions reflect advancements in understanding functional limitations, technological advancements, and evolving healthcare needs. Early versions focused primarily on motor skills, while later versions incorporated cognitive and communication aspects, providing a more holistic assessment. These updates underscore the ongoing commitment to enhancing the FIM’s sensitivity and comprehensiveness.
Current Research on the FIM
Research utilizing the FIM continues to yield valuable insights into its application and limitations. Studies are exploring the FIM’s predictive validity in diverse populations, including those with specific neurological conditions, and investigating the tool’s sensitivity to change over time. This research is crucial in refining the FIM’s application and improving its effectiveness in various clinical settings. Furthermore, ongoing studies investigate the correlation between FIM scores and other outcome measures, helping to establish more robust benchmarks for rehabilitation success.
Potential Future Developments for the FIM
Future developments in the FIM might include incorporating emerging technologies. Imagine a future where wearable sensors could automatically track functional performance, providing real-time data to clinicians and patients. This integration could lead to more personalized interventions and a more dynamic assessment process. Another area of potential development is adapting the FIM for use with diverse populations, including those with cultural or language barriers.
This adaptation could enhance the tool’s cultural sensitivity and improve its applicability in various global contexts.
Recent Studies Using the FIM
- A study published in the Journal of Rehabilitation Medicine (2022) examined the predictive validity of the FIM in stroke patients, finding a strong correlation between initial FIM scores and long-term functional outcomes. This reinforces the FIM’s value in anticipating future performance and guiding treatment strategies.
- A research article in the Archives of Physical Medicine and Rehabilitation (2023) explored the effectiveness of a new rehabilitation program for individuals with traumatic brain injury. The study employed the FIM to assess the program’s impact on functional independence, demonstrating a significant improvement in scores over the course of the intervention.
- Research published in the Disability and Rehabilitation journal (2021) investigated the feasibility of using the FIM in a telehealth setting, showing the tool’s potential to support remote rehabilitation programs. This suggests a promising avenue for expanding access to rehabilitation services.
Last Word
In conclusion, the Functional Independence Measurement stands as a valuable tool for assessing functional abilities in healthcare. Its comprehensive approach, detailed scoring system, and practical applications make it a key component in patient rehabilitation and discharge planning. While limitations and criticisms exist, the FIM’s adaptability and potential for improvement make it a relevant assessment tool for various healthcare contexts.
Further research and development in this area promise to refine and enhance its future applications.









