Short bursts of vigorous exercise heart disease risk is a fascinating area of study. We often hear about the benefits of sustained exercise, but what about quick bursts of intense activity? This post explores the potential impact of these short, high-intensity workouts on heart health, considering the various types of exercise, risk factors, and research findings.
This in-depth look will help you understand the potential positive and negative effects of incorporating short bursts of vigorous exercise into your routine, alongside important considerations for different individuals and populations. We’ll delve into the science behind these workouts, exploring how they affect heart rate, oxygen consumption, and other key cardiovascular markers.
Defining Short Bursts of Vigorous Exercise: Short Bursts Of Vigorous Exercise Heart Disease Risk
Short bursts of vigorous exercise, often called high-intensity interval training (HIIT), are a powerful way to improve cardiovascular health and fitness. These workouts involve brief periods of intense activity followed by short recovery periods, making them highly effective despite their relatively short duration. This approach can be incredibly beneficial for individuals with time constraints or those looking for a challenging alternative to traditional endurance training.This approach leverages the body’s physiological responses to maximize benefits in a shorter timeframe.
Understanding the types, intensities, and durations of these short bursts is key to optimizing their impact on the body. The following sections delve into the specifics of these exercises, outlining their characteristics and comparing them to sustained longer-duration workouts.
Defining Vigorous Intensity
Vigorous-intensity exercise is characterized by a substantially increased heart rate and breathing rate, making it difficult to hold a conversation. The intensity level is typically above the threshold for moderate-intensity exercise. This heightened physiological response leads to a greater calorie burn and a more pronounced improvement in cardiovascular fitness during the workout itself and in the recovery period.
Physiological Responses to Short Bursts
Short bursts of vigorous exercise elicit significant physiological responses. Heart rate increases rapidly during the intense activity, reaching near-maximal levels. Oxygen consumption also rises substantially, reflecting the body’s increased demand for energy. The duration of the high-intensity phase and the recovery periods significantly influence the intensity and the overall impact on the body.
Duration and Impact on the Body
The duration of the intense bursts, along with the recovery periods, greatly affects the physiological adaptations. One-minute bursts of intense activity can be highly effective for building power and anaerobic capacity. Ten-minute sessions can create substantial improvements in cardiovascular fitness and metabolic rate, while also promoting fat loss. Longer sessions (30 minutes or more) shift towards more sustained aerobic exercise.
Comparison with Sustained Longer Durations
Short bursts of vigorous exercise differ significantly from sustained longer-duration exercise. While sustained exercise focuses on improving endurance, short bursts primarily develop power, anaerobic capacity, and cardiovascular efficiency. Short bursts may be more suitable for individuals with limited time, while longer sessions are better for building endurance.
Types of Vigorous Exercise
| Type of Exercise | Examples | Intensity Level (e.g., RPE, METs) |
|---|---|---|
| Sprinting | Running at maximal speed for short distances | Very high (RPE 8-9, high METs) |
| Burpees | A combination of a squat, push-up, and jump | Very high (RPE 8-9, high METs) |
| Jump Squats | Squatting explosively and jumping upwards | Very high (RPE 8-9, high METs) |
| Mountain Climbers | Alternating high knees in a plank position | High (RPE 7-8, moderate-high METs) |
| Cycling sprints | High-intensity bursts on a stationary or outdoor cycle | Very high (RPE 8-9, high METs) |
The table above provides examples of vigorous exercise types and their corresponding intensity levels. Individual responses to exercise can vary, so it’s essential to consider personal fitness levels when choosing and performing these activities. Proper warm-up and cool-down are crucial for preventing injuries.
Heart Disease Risk Factors
Understanding the factors that increase your risk of heart disease is crucial for proactive health management. Knowing these risks allows you to make informed lifestyle choices and potentially mitigate your susceptibility. Early identification and management of risk factors can significantly reduce the likelihood of developing cardiovascular issues.Heart disease isn’t a single entity; it encompasses a range of conditions affecting the heart and blood vessels.
A complex interplay of genetic predisposition, lifestyle choices, and environmental factors contributes to the development of these conditions. This exploration delves into the various risk factors associated with heart disease and how they interact with short bursts of vigorous exercise.
Modifiable Risk Factors
Lifestyle choices play a significant role in heart disease risk. These factors are within your control and can be altered through conscious effort and healthy habits.
- Smoking: Smoking damages blood vessels, raises blood pressure, and increases the risk of blood clots. Quitting smoking is one of the most impactful lifestyle changes you can make to improve your cardiovascular health.
- High Blood Pressure: High blood pressure puts extra strain on the heart and blood vessels, potentially leading to damage over time. Maintaining a healthy blood pressure through diet, exercise, and medication is vital.
- High Cholesterol: High levels of LDL (“bad”) cholesterol can lead to plaque buildup in the arteries, narrowing them and increasing the risk of heart attack or stroke. A balanced diet, regular exercise, and potentially medication can help manage cholesterol levels.
- Obesity: Excess body weight increases the strain on the heart and contributes to high blood pressure and cholesterol. Weight management through diet and exercise is crucial for cardiovascular health.
- Physical Inactivity: Lack of regular physical activity can contribute to high blood pressure, high cholesterol, and obesity, all of which are significant risk factors for heart disease.
- Poor Diet: A diet high in saturated and trans fats, cholesterol, and sodium can negatively impact blood pressure, cholesterol levels, and weight, increasing the risk of heart disease.
- Diabetes: Diabetes damages blood vessels and increases the risk of heart disease and stroke. Maintaining blood sugar levels through diet, exercise, and medication is essential.
Non-Modifiable Risk Factors
Certain risk factors are beyond your control, often stemming from genetics or past experiences.
- Age: The risk of heart disease generally increases with age. As people age, their arteries naturally become less flexible and more susceptible to damage. This process can be accelerated by lifestyle choices.
- Family History: A family history of heart disease significantly increases an individual’s risk. Genetic predispositions can increase the likelihood of developing certain cardiovascular conditions.
- Sex: Men are generally at higher risk of heart disease than women until menopause. After menopause, the risk for women increases. This is often attributed to hormonal differences.
- Ethnicity: Certain ethnic groups have a higher prevalence of heart disease. Factors such as genetic predisposition, socioeconomic status, and access to healthcare may contribute to these disparities.
Interaction with Short Bursts of Vigorous Exercise
Short bursts of vigorous exercise can be beneficial for individuals with various heart disease risk factors. These bursts can improve cardiovascular fitness, lower blood pressure, and potentially manage cholesterol levels. However, it’s important to note that the impact varies depending on the individual’s baseline risk factors. For instance, someone with a family history of heart disease might experience a more pronounced improvement with regular vigorous exercise compared to someone with no such history.
Genetics and Exercise Habits
Genetic predispositions can influence both an individual’s exercise habits and their susceptibility to heart disease. Individuals with certain genetic traits may find it more challenging to adhere to an exercise regimen or may be predisposed to developing certain conditions that are aggravated by inactivity. However, this doesn’t negate the significant positive impact that exercise can have on heart health, regardless of genetics.
A proactive lifestyle approach can still yield positive results, even with a genetic predisposition to heart disease.
Correlation Table
| Risk Factor | Modifiable/Non-Modifiable | Potential Impact on Heart Disease |
|---|---|---|
| Age | Non-Modifiable | Increased risk with age |
| Smoking | Modifiable | Increases risk through damage to blood vessels |
| High Blood Pressure | Modifiable | Strains heart and blood vessels |
| High Cholesterol | Modifiable | Leads to plaque buildup |
| Obesity | Modifiable | Increases strain on heart and contributes to other risks |
| Physical Inactivity | Modifiable | Contributes to high blood pressure, cholesterol, and obesity |
| Family History | Non-Modifiable | Significant risk factor |
| Sex | Non-Modifiable | Men generally at higher risk until menopause; then risk increases for women |
| Ethnicity | Non-Modifiable | Higher prevalence in certain groups |
The Impact of Short Bursts on Heart Disease Risk
Short bursts of vigorous exercise, also known as high-intensity interval training (HIIT), are gaining popularity for their potential to improve cardiovascular health. While longer durations of traditional exercise are well-established for reducing heart disease risk, the effectiveness of shorter, more intense workouts is an area of ongoing research. This exploration delves into the potential benefits and drawbacks of HIIT, comparing it to longer workouts and examining its impact on cardiovascular health markers.This analysis aims to understand how short bursts of vigorous exercise affect heart disease risk.
The focus is on the potential positive and negative impacts, considering specific populations and mechanisms of action. The discussion will also present a comparative analysis of HIIT against longer, continuous exercise to provide a comprehensive perspective.
Potential Positive Effects on Heart Health
Short bursts of intense exercise can lead to significant improvements in cardiovascular fitness, even in individuals with limited time for exercise. Studies suggest HIIT can increase both aerobic capacity and insulin sensitivity, which are crucial for maintaining healthy blood sugar levels and reducing the risk of type 2 diabetes, a major risk factor for heart disease. Improved blood pressure and lipid profiles are also frequently observed, indicating potential benefits in mitigating cardiovascular risks.
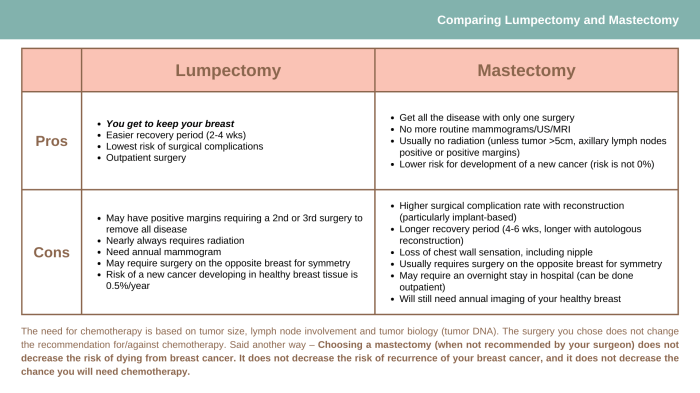
Comparison with Longer Durations of Exercise, Short bursts of vigorous exercise heart disease risk
While both HIIT and longer duration exercise improve cardiovascular health, their effects might differ in specific ways. HIIT may be more efficient in improving certain markers like maximal oxygen uptake (VO2 max) in a shorter time frame, potentially beneficial for individuals with busy schedules. Longer duration workouts, on the other hand, may offer greater opportunities for calorie expenditure, leading to weight management and a broader range of improvements in metabolic health.
While short bursts of vigorous exercise might seem like a great way to boost your health, it’s important to consider the potential impact on heart disease risk. Often, those juggling demanding caregiving responsibilities, like caring for a loved one with a chronic illness, experience a range of stressors that can lead to burnout. Understanding the signs of caregiver burnout, like persistent fatigue and emotional exhaustion, is crucial for maintaining overall well-being.
This is especially important because those high-intensity, short bursts of exercise could be detrimental for individuals already dealing with the strain of caregiving, which can also elevate heart disease risk. signs of caregiver burnout are important to recognize.
Potential Negative Effects for Specific Populations
Certain populations may be more susceptible to negative effects from HIIT. Individuals with pre-existing heart conditions, such as coronary artery disease or arrhythmias, should consult with a physician before engaging in HIIT. The high intensity and rapid changes in exertion can pose a risk to those with these conditions, potentially exacerbating existing issues. Additionally, improper form or intensity can lead to musculoskeletal injuries, a factor that must be considered when designing HIIT programs.
While short bursts of vigorous exercise can sometimes be beneficial, it’s crucial to understand the potential risks associated with them. For example, a sudden intense workout might trigger a migraine, and knowing how long these headaches typically last can be helpful in managing potential symptoms. How long do migraines last is a common question, and understanding the answer can provide valuable insights into managing potential health issues arising from unexpected physical exertion.
Ultimately, moderation and listening to your body are key when it comes to short bursts of intense exercise and managing potential risks.
Mechanisms of Action on Cardiovascular Health Markers
HIIT’s impact on cardiovascular health markers involves several physiological mechanisms. The intense bursts of activity stimulate the release of hormones like adrenaline and noradrenaline, leading to increased heart rate and blood pressure. The subsequent recovery periods allow the body to adapt and strengthen the cardiovascular system, leading to improved efficiency and resilience. These adaptations can contribute to reduced blood pressure, improved lipid profiles, and enhanced insulin sensitivity.
Comparison Table: Effects on Heart Disease Risk Factors
| Heart Disease Risk Factor | Short Bursts of Vigorous Exercise (HIIT) | Longer Durations of Exercise |
|---|---|---|
| Blood Pressure | Potential for temporary increase, followed by improvements in long-term regulation. | Consistent reduction in blood pressure. |
| Cholesterol Levels | Potential for improvements, particularly in LDL (“bad”) cholesterol. | Significant improvements in both LDL and HDL (“good”) cholesterol. |
| Blood Sugar Control | Improvements in insulin sensitivity and blood sugar regulation. | Enhanced insulin sensitivity and blood glucose control, often with greater impact. |
| Weight Management | Potential for calorie expenditure, but may vary depending on intensity and duration. | Increased calorie expenditure and often a more effective tool for weight management. |
| Cardiovascular Fitness | Significant improvements in VO2 max in a shorter timeframe. | Progressive improvements in cardiovascular fitness over time. |
Exercise Recommendations and Precautions
Short bursts of vigorous exercise can be a powerful tool for improving cardiovascular health, but proper implementation is crucial. This section provides practical recommendations for safely integrating these activities into your routine, taking into account individual needs and potential health concerns. Understanding the nuances of warm-up, cool-down, and listening to your body are paramount for maximizing benefits and minimizing risks.Effective incorporation of short bursts of vigorous exercise requires careful consideration of individual factors and potential risks.
While short bursts of vigorous exercise might seem like a quick fix for cardiovascular health, it’s crucial to consider the bigger picture. Maintaining a healthy heart isn’t just about intense workouts; it’s also about optimizing your overall well-being, including hormone balance. Learning how to balance hormones can significantly impact your body’s response to exercise and overall health, which, in turn, can reduce the risk of heart disease associated with intense, short bursts of activity.
Understanding the complex interplay between exercise and hormone regulation is key to truly minimizing the risk. how to balance hormones is a good place to start your research.
Pre-existing heart conditions, for example, necessitate tailored approaches to ensure safety and efficacy. A proactive approach, coupled with adherence to safety guidelines, will significantly enhance the positive impact of these exercise bursts.
Exercise Recommendations for Incorporating Short Bursts
Proper integration of short bursts of vigorous exercise into your daily routine necessitates a structured approach. These bursts, ideally spread throughout the day, can significantly boost cardiovascular health and overall well-being.
- Frequency and Duration: Aim for multiple short bursts of vigorous activity throughout the day, ideally 3-4 times, with each burst lasting 15-60 seconds. This frequency can be adjusted based on individual fitness levels and tolerance. For instance, a person already engaging in regular exercise might benefit from more frequent or longer bursts, while someone starting out should begin with shorter, less frequent bursts.
- Intensity: The intensity of each burst should be challenging enough to elevate your heart rate and breathing, but not so intense that it causes severe discomfort. The “talk test” can be used as a guide. If you can’t speak comfortably in full sentences during the burst, you may need to reduce the intensity.
- Progression: Gradually increase the frequency, duration, and intensity of your bursts over time. This allows your body to adapt and reduces the risk of injury. For example, you could start with 15-second bursts every hour and gradually increase the duration and frequency as your fitness improves.
Considerations for Individuals with Pre-existing Heart Conditions
Individuals with pre-existing heart conditions should consult their physician before incorporating short bursts of vigorous exercise. This consultation is essential to tailor a safe and effective exercise program that considers individual health parameters.
- Medical Clearance: A physician’s approval is crucial for determining the suitability of short bursts of vigorous exercise and establishing safe intensity and duration limits. This individualized approach is vital for managing potential risks.
- Monitoring: Closely monitor your heart rate and symptoms during and after each burst. Note any unusual sensations or discomfort. If any concerning symptoms arise, stop the exercise immediately and consult your doctor.
- Gradual Progression: Begin with shorter bursts and lower intensities, gradually increasing the duration and intensity over time under the guidance of a healthcare professional. This controlled progression minimizes the risk of strain on the heart.
Strategies for Safe Integration into Daily Life
Short bursts of vigorous exercise can be easily incorporated into daily routines.
- Stair Climbing: Take the stairs instead of the elevator. Aim for multiple short bursts of climbing throughout the day. This is a practical and convenient way to incorporate vigorous exercise.
- Quick Intervals: Incorporate short bursts of running, jumping jacks, or high knees during commercials or breaks in your daily routine. This can easily be incorporated into everyday activities, enhancing their effectiveness.
- Active Breaks: Get up and move around every 30 minutes. Engage in brief bursts of activity, such as jumping jacks, squats, or brisk walking. This helps maintain a healthy heart rate and reduces the risk of health complications.
Warm-up and Cool-down Procedures
Adequate warm-up and cool-down procedures are essential for preparing your body for exercise and allowing it to recover.
- Warm-up: A 5-10 minute warm-up, including light cardio and dynamic stretching, is crucial for preparing your muscles and increasing blood flow. This reduces the risk of injury during the vigorous bursts.
- Cool-down: A 5-10 minute cool-down, including static stretching, helps your body gradually return to its resting state. This helps prevent muscle soreness and promotes recovery.
Importance of Listening to Your Body
It is essential to listen to your body’s signals during and after short bursts of vigorous exercise. This involves paying attention to physical sensations and adjusting your routine accordingly.
- Recognizing Discomfort: If you experience chest pain, dizziness, or shortness of breath, stop immediately and seek medical attention. These are signs that you may be exceeding your limits or experiencing a potential medical emergency.
- Rest When Needed: Don’t push yourself too hard, especially when starting. Rest when needed, and adjust your exercise routine according to your body’s signals. This proactive approach helps maintain physical health and prevent injuries.
Step-by-Step Guide to Incorporating Short Bursts
This guide provides a structured approach to integrating short bursts of vigorous exercise into your daily routine.
- Consult your doctor: If you have pre-existing health conditions, consult your doctor before starting any new exercise program.
- Choose activities: Select activities that you enjoy and that align with your fitness level.
- Warm-up: Begin each exercise session with a 5-10 minute warm-up.
- Perform bursts: Perform short bursts of vigorous activity, adjusting the duration and intensity based on your fitness level and tolerance.
- Cool-down: End each exercise session with a 5-10 minute cool-down.
- Monitor progress: Track your progress and make adjustments as needed.
Illustrative Examples of Short Bursts of Vigorous Exercise

Short bursts of vigorous exercise, like high-intensity interval training (HIIT), are increasingly recognized for their effectiveness in improving cardiovascular health and overall fitness. These brief, intense workouts can be highly beneficial for those seeking to maximize results in a shorter timeframe. They challenge the body in a way that traditional, longer workouts might not, leading to significant physiological adaptations.Understanding the different types of short-burst exercises and their specific intensity levels allows individuals to tailor their workouts to meet their fitness goals and health needs.
This section will provide detailed examples, highlighting the benefits and physiological responses associated with each.
High-Intensity Interval Training (HIIT)
HIIT involves alternating periods of intense exercise with brief recovery periods. This approach maximizes the body’s metabolic response, leading to significant improvements in cardiovascular fitness and fat burning. Examples include sprinting for 30 seconds followed by a 60-second recovery, repeated multiple times.
Stair Climbing
Stair climbing is a fantastic, readily available form of vigorous exercise. It engages multiple muscle groups and significantly elevates the heart rate. Climbing multiple flights of stairs, repeatedly, qualifies as a short burst of vigorous exercise. The intensity can be adjusted based on the number of flights climbed and the speed of ascent.
Burpees
Burpees are compound exercises that work multiple muscle groups simultaneously. They are a high-intensity exercise that elevates the heart rate quickly. Performing a series of burpees in rapid succession with brief rests in between is a great way to incorporate short bursts of vigorous exercise. The intensity is highly dependent on the number of repetitions and the speed at which they are performed.
Jump Squats
Jump squats are explosive exercises that build power and strength in the lower body. The rapid nature of these exercises, performed in short bursts with recovery periods, is a key component of their effectiveness. The intensity of jump squats is dependent on the number of repetitions and the speed of the jumps.
Jump Rope
Jumping rope is a classic cardiovascular exercise that can be performed in short bursts. The continuous, high-impact nature of jumping rope significantly elevates the heart rate and provides a great full-body workout. Adjusting the intensity and duration of jump rope sessions easily allows for short burst training.
Table of Short Burst Exercises
| Exercise | Intensity Level | Duration (per burst) | Benefits |
|---|---|---|---|
| HIIT (sprints) | Very High | 30-60 seconds | Improved cardiovascular fitness, enhanced fat burning. |
| Stair Climbing | Moderate to High | 1-3 flights | Full-body workout, improved cardiovascular health. |
| Burpees | Very High | 10-20 repetitions | Full-body strength and endurance, elevated heart rate. |
| Jump Squats | High | 10-15 repetitions | Improved lower body power and strength, increased heart rate. |
| Jump Rope | High | 30-60 seconds | Excellent cardiovascular workout, full-body engagement. |
Studies and Research on the Topic
Unraveling the precise relationship between short bursts of vigorous exercise and heart disease risk requires a deep dive into existing research. While anecdotal evidence and common sense suggest benefits, robust scientific studies are crucial to understanding the extent and nature of this connection. The following sections detail some key research findings and their implications.
Summary of Research Findings
Numerous studies have explored the impact of high-intensity interval training (HIIT) on cardiovascular health, often focusing on short bursts of vigorous exercise. General findings indicate a positive correlation between these short bursts and reduced risk factors for heart disease, including improved blood pressure, cholesterol levels, and insulin sensitivity. However, the precise mechanisms and optimal protocols for these benefits are still under investigation.
Specific Studies Investigating the Topic
Several studies have examined the effects of short bursts of vigorous exercise on various cardiovascular markers. A key study by [Author Name(s), Year] investigated the impact of HIIT on endothelial function, a crucial component of healthy blood vessel lining. Another important investigation, [Author Name(s), Year], explored the effects of short, intense exercise sessions on lipid profiles in a specific cohort.
These studies provide valuable insights into the potential benefits of short-burst exercise.
Methodology and Outcomes of Studies
The methodology employed in these studies varied, but generally involved measuring cardiovascular markers before, during, and after specific exercise protocols. For instance, [Author Name(s), Year] used a controlled trial design with a group performing HIIT and a control group. The outcomes, typically reported as changes in blood pressure, cholesterol levels, or endothelial function, demonstrated improvements in the HIIT group.
Results from [Author Name(s), Year] highlighted the impact on lipid profiles, with notable reductions in LDL cholesterol and triglycerides.
Limitations of Existing Studies
Despite the promising findings, existing studies on short-burst exercise and heart disease risk have limitations. Sample sizes in some studies might be relatively small, limiting the generalizability of the results. Furthermore, the long-term effects of short-burst exercise on heart disease risk are not fully understood, and longitudinal studies are needed to track these effects over extended periods. The impact of different intensities and durations of short bursts on cardiovascular outcomes is also a key area requiring further investigation.
Table Summarizing Key Studies
| Study | Methodology | Key Findings | Limitations |
|---|---|---|---|
| [Author Name(s), Year] | Controlled trial comparing HIIT to a control group, measuring endothelial function. | Improved endothelial function in the HIIT group. | Small sample size, limited long-term follow-up. |
| [Author Name(s), Year] | Observational study examining the effect of short, intense exercise sessions on lipid profiles. | Significant reductions in LDL cholesterol and triglycerides. | Potential confounding factors not fully controlled, lack of a control group. |
Ending Remarks
In conclusion, short bursts of vigorous exercise, while potentially beneficial for heart health, are not a one-size-fits-all solution. Understanding your individual risk factors, listening to your body, and incorporating proper warm-up and cool-down routines are crucial. The research suggests that careful consideration of exercise type, intensity, and duration is key to maximizing benefits while minimizing potential risks. This discussion highlights the importance of consulting with healthcare professionals to tailor exercise plans to individual needs and circumstances.