When to expect covid 19 vaccination side effects – When to expect COVID-19 vaccination side effects? This guide provides a detailed timeline of when common side effects typically appear, helping you understand what to anticipate after getting vaccinated. We’ll explore the factors that influence side effect timing, such as individual differences, vaccine type, and pre-existing conditions. Furthermore, we’ll discuss the severity and duration of these effects, and importantly, when to seek medical attention.
Understanding the immune response to the vaccine will provide valuable insights into why some people experience certain side effects.
The information presented here is intended for educational purposes only and should not be considered medical advice. Always consult with your healthcare provider for personalized guidance. Different vaccines have slightly varying timelines for side effects, which is why it’s crucial to understand the range of expected onset times.
Timing of Side Effects
Understanding when COVID-19 vaccine side effects appear is crucial for managing expectations and ensuring individuals are aware of what to anticipate. This knowledge empowers individuals to distinguish between normal reactions and potential issues, promoting proactive health management following vaccination.The timing of side effects varies significantly, influenced by individual factors like age, health status, and the specific vaccine received. While some individuals experience no noticeable side effects, others may experience mild to moderate discomfort.
The key is to understand the typical timeframe for different reactions.
Generally, COVID-19 vaccine side effects like soreness or fatigue pop up within a few days of the shot. Sometimes, though, you might be grappling with much bigger decisions, like weighing the pros and cons of continuing dialysis. Navigating such tough choices requires careful consideration and a support system. If you’re considering stopping dialysis, it’s crucial to consult with your medical team to discuss the potential implications.
Ultimately, knowing when to anticipate those post-vaccine reactions is part of managing your overall health. Expect these effects to typically show up within a few days to a week after the injection.
Typical Onset Times for COVID-19 Vaccine Side Effects
Common side effects often manifest within a few days of vaccination. Some reactions are immediate, while others may develop over a longer period. The following table provides a general guideline, but individual experiences can differ.
| Side Effect | Typical Onset Time | Duration |
|---|---|---|
| Soreness | 1-2 days | 2-3 days |
| Fever | 1-2 days | 1-3 days |
| Fatigue | 1-3 days | 3-7 days |
| Headache | 1-2 days | 1-3 days |
| Muscle aches | 1-2 days | 2-5 days |
| Chills | 1-2 days | 1-2 days |
| Nausea | 1-3 days | 1-2 days |
| Swelling at injection site | 1-2 days | 1-7 days |
Comparison of Vaccine Onset Times
Different COVID-19 vaccines may have slightly varying timelines for side effect appearance. For example, some mRNA vaccines, like those from Pfizer-BioNTech and Moderna, might show more immediate reactions compared to some other types. However, general trends remain consistent across various vaccine platforms. Research findings consistently point to a similar range of onset times.
Individual Variations in Response
Individual responses to COVID-19 vaccines can vary widely. Factors such as pre-existing health conditions, overall immune response, and even stress levels can influence the experience. Some people may experience more pronounced side effects, while others might not experience any at all. The key is to understand the typical range and to monitor for any unusual or concerning symptoms.
Factors Influencing Side Effect Timing
Understanding when you might experience side effects from a COVID-19 vaccination is crucial for managing expectations and ensuring you’re not unduly alarmed. Beyond the general timeframe, various factors can influence the precise moment and intensity of these responses. These factors can range from individual differences in immune responses to the specific type of vaccine administered.While the majority of individuals experience mild to moderate side effects within a few days of vaccination, the timing and severity can vary significantly.
Generally, COVID-19 vaccination side effects, like soreness or fatigue, typically appear within a few days of the shot. However, some people experience lingering symptoms, and it’s crucial to understand that these symptoms can sometimes mimic other conditions. For example, if you’re experiencing persistent sinus pressure or congestion, you might wonder if it’s related to the vaccine or something else, like a sinus infection.
Learning about sinus infection symptoms and COPD can help differentiate between potential causes sinus infection symptoms and copd. Ultimately, it’s best to consult your doctor if you’re unsure about the source of any unusual symptoms after receiving the vaccine.
This variation is often due to complex interactions between the individual’s body, the vaccine’s characteristics, and potential underlying health conditions. Understanding these influences can help you anticipate potential side effects and manage any concerns proactively.
Individual Differences in Immune Response
Individual variations in immune responses play a significant role in shaping the timing and intensity of side effects. Some individuals may mount a stronger immune response than others, leading to more pronounced symptoms. This variability is a natural part of the human immune system’s complexity and is not necessarily indicative of a negative outcome. Factors such as age, overall health, and pre-existing conditions can all contribute to the individual’s unique immune response, affecting the onset and duration of side effects.
Role of Pre-existing Health Conditions
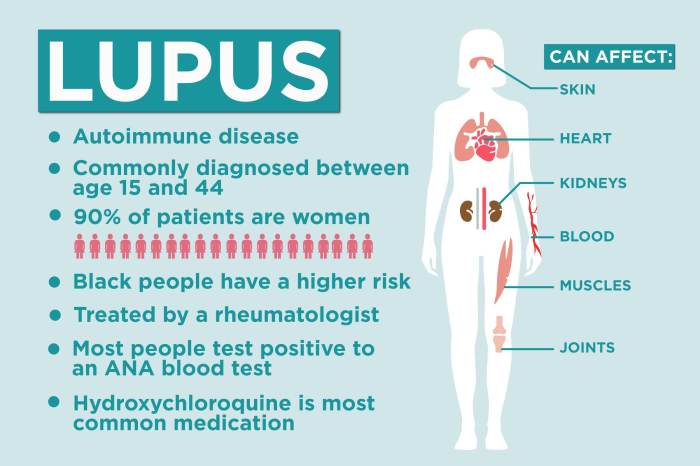
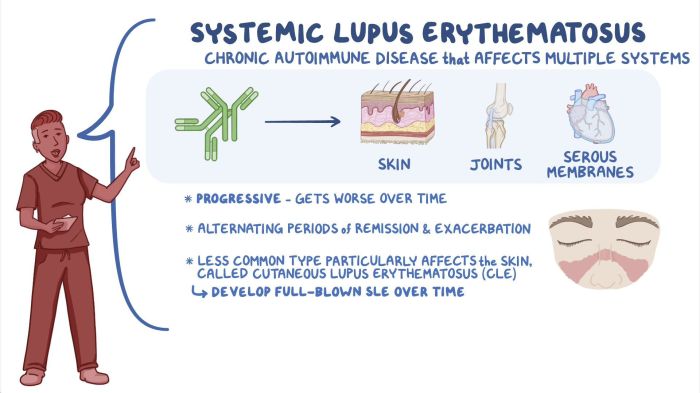
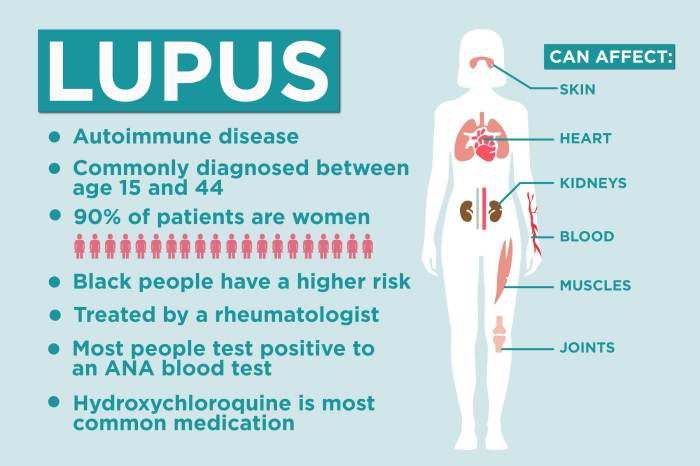
Pre-existing health conditions can potentially influence the timing and severity of vaccine side effects. Individuals with certain medical conditions, such as autoimmune disorders or weakened immune systems, might experience side effects sooner or later than those without such conditions. For example, someone with a compromised immune system might experience a delayed response, while someone with an acute inflammatory condition might experience symptoms earlier than anticipated.
It’s important to discuss any pre-existing conditions with your healthcare provider to better understand how they might affect your response to the vaccine.
Vaccine Type and Dosage
The specific type of COVID-19 vaccine can also influence the timing and intensity of side effects. Different vaccines use various technologies to stimulate an immune response, which can lead to different patterns of reactions. For example, mRNA vaccines often trigger a quicker immune response compared to some other types, potentially leading to symptoms appearing earlier. Similarly, the dosage of the vaccine can also influence the intensity and duration of side effects.
It’s important to remember that these variations are typical and not necessarily a cause for concern.
Situations Where Side Effects Might Appear Earlier or Later
In some situations, side effects may appear earlier or later than the typical timeframe. For example, individuals who have recently experienced significant stress or illness may experience a heightened immune response, leading to earlier onset of symptoms. Conversely, individuals with a suppressed immune system might not experience side effects until significantly later. Furthermore, the timing can vary based on the individual’s overall health, including their nutritional status, sleep habits, and hydration levels.
| Factor | Possible Impact on Timing |
|---|---|
| Pre-existing conditions | Potential for earlier or later onset, different severity |
| Individual immune response | Varying degrees of response, influencing symptom presentation |
| Vaccine type | Potentially impacting the timing and intensity of side effects |
| Dosage | Potentially impacting the timing and intensity of side effects |
| Stress levels | Potential for earlier onset and increased severity |
| Nutritional status | Potential for altered immune response |
Severity and Duration of Side Effects
Understanding the potential range of side effects from COVID-19 vaccines is crucial for managing expectations and ensuring informed decisions. While the vast majority of individuals experience mild or moderate reactions, knowing the spectrum of possible responses can help you navigate any concerns that may arise.The severity and duration of side effects can vary significantly depending on several factors, including the specific vaccine received, an individual’s overall health, and their immune response.
This section delves into the typical severity and duration of common side effects, providing examples to illustrate the range of potential experiences.
Typical Severity and Duration of Common Side Effects
The most common side effects from COVID-19 vaccines are generally mild and resolve within a few days. These reactions are a sign that your immune system is responding to the vaccine, building protection against the virus. Severe side effects are rare.
Examples of Mild, Moderate, and Severe Side Effects
Mild side effects are often described as minor discomforts that are easily manageable. Examples include soreness at the injection site, fatigue, or mild headache.Moderate side effects can be more noticeable but usually do not require medical intervention. Examples include fever, chills, muscle aches, or swelling at the injection site. These are usually temporary and resolve within a few days.Severe side effects are less common and may require medical attention.
Symptoms might include difficulty breathing, severe allergic reactions (anaphylaxis), or prolonged or high fever. In the event of a severe reaction, immediate medical attention is crucial.
So, you’ve gotten your COVID-19 vaccine – now, when can you expect those potential side effects? Generally, you might notice them within a few days of the shot, but sometimes they can linger for a bit longer. Interestingly, the duration of some side effects can be comparable to how long marijuana stays in your system, which can vary significantly depending on factors like metabolism and individual body composition.
how long does marijuana stay in your system Ultimately, the best advice is to listen to your body and keep an eye out for any unusual symptoms. Hopefully, you’ll experience a speedy recovery with minimal side effects!
Comparison of Severity and Duration Across Vaccine Types
The following table summarizes the typical severity and duration of common side effects across different COVID-19 vaccine types. Note that these are general observations, and individual experiences may vary.
| Side Effect | Severity (Mild/Moderate/Severe) | Duration |
|---|---|---|
| Soreness | Mild | 2-3 days |
| Fever | Moderate | 1-3 days |
| Headache | Mild | 1-2 days |
| Fatigue | Mild/Moderate | 1-5 days |
| Chills | Moderate | 1-2 days |
| Nausea | Mild/Moderate | 1-2 days |
| Muscle pain | Mild/Moderate | 1-3 days |
| Swelling at injection site | Mild | 1-7 days |
| Allergic reaction (anaphylaxis) | Severe | Immediate (requires immediate medical attention) |
When to Seek Medical Attention: When To Expect Covid 19 Vaccination Side Effects

Knowing when to seek medical attention for COVID-19 vaccination side effects is crucial for ensuring your well-being. While most side effects are mild and resolve on their own, some require immediate medical intervention. This section Artikels the situations warranting prompt medical evaluation and the procedures for reporting concerns.
Recognizing Serious Side Effects
Understanding the potential range of side effects is essential. Mild reactions, like soreness at the injection site or fatigue, are common and usually temporary. However, some side effects may signal a more serious underlying issue. Prompt medical attention is vital for severe or unusual reactions.
Symptoms Requiring Immediate Medical Evaluation
Certain symptoms necessitate immediate medical evaluation. These symptoms could indicate a serious allergic reaction, a more severe infection, or other complications. Timely intervention can significantly improve the outcome.
- Difficulty breathing or shortness of breath. This can be a sign of a severe reaction or other respiratory complications. Rapid or labored breathing warrants immediate medical evaluation.
- Severe allergic reaction, including hives, swelling of the face, lips, tongue, or throat, difficulty swallowing, or wheezing. These symptoms may indicate anaphylaxis, a potentially life-threatening allergic reaction requiring immediate medical intervention.
- Severe chest pain or tightness. This symptom could signal a heart-related issue or other serious conditions. Any chest pain, especially if accompanied by shortness of breath, should be addressed immediately.
- Severe dizziness or lightheadedness, accompanied by fainting or loss of consciousness. These could indicate a serious cardiovascular or neurological issue, requiring prompt medical attention.
- Persistent or severe headache, particularly if accompanied by fever or stiff neck. These symptoms could suggest meningitis or other infections, necessitating urgent medical attention.
- Sudden onset of weakness or numbness in an arm or leg. This can be a sign of a stroke or other neurological condition. Seek immediate medical attention if you experience these symptoms.
Importance of Reporting Unusual Side Effects
It’s crucial to report any unusual or concerning side effects to your healthcare provider. Your healthcare provider can assess the situation, determine if further evaluation is needed, and provide appropriate guidance. This includes symptoms not listed in this guide but that cause concern. Trust your instincts; if something feels wrong, seek medical advice.
Reporting Procedures for Side Effects, When to expect covid 19 vaccination side effects
Reporting side effects to the relevant health authorities is essential for monitoring the safety and efficacy of the COVID-19 vaccine. This process helps track potential issues and ensure that public health officials have a comprehensive understanding of vaccine safety. Follow your healthcare provider’s instructions for reporting any concerns. Check your local health department’s website for specific procedures or contact information.
| Symptom | Action |
|---|---|
| Difficulty breathing | Seek immediate medical attention |
| Severe allergic reaction | Seek immediate medical attention |
| Severe chest pain | Seek immediate medical attention |
| Sudden weakness or numbness | Seek immediate medical attention |
| Persistent severe headache with fever or stiff neck | Seek immediate medical attention |
Understanding the Immune Response
The COVID-19 vaccines don’t inject the virus itself. Instead, they teach your immune system to recognize and fight off the virus. Understanding how this works is crucial for comprehending potential side effects. This process, while designed to protect you, can sometimes trigger a noticeable response.The immune response to the COVID-19 vaccine is a complex series of events. It’s a carefully orchestrated process that involves multiple cell types and signaling pathways.
This sophisticated response is essential for generating lasting protection against the virus.
The Normal Immune Response to the COVID-19 Vaccine
The COVID-19 vaccines, whether mRNA or viral vector, stimulate the immune system to create an adaptive response. This response, unique to each individual, involves several crucial steps. First, the vaccine introduces pieces of the virus, like the spike protein, into the body. These pieces are harmless, but they trigger an initial immune response. This initial response activates various immune cells, particularly lymphocytes.
How the Immune Response Can Lead to Side Effects
The activation of immune cells and the subsequent production of antibodies and other immune factors can lead to side effects. The immune system’s vigorous response to the vaccine components is responsible for these side effects, which are a sign that the body is working to develop immunity. These responses, while sometimes unpleasant, are temporary and are a measure of the vaccine’s effectiveness.
How the Immune System Builds Protection Against the Virus
The immune system creates a defense against the virus by generating memory cells. These memory cells “remember” the virus and can quickly respond if the body encounters the actual virus in the future. The immune system learns to identify and destroy the virus much more efficiently during a future infection. This rapid response is the foundation of long-term protection.
This sophisticated system is crucial in preventing serious illness from COVID-19.
The Role of Antibodies in the Immune Response
Antibodies are a key component of the immune response to the COVID-19 vaccines. They are specialized proteins produced by the immune system to neutralize the virus. These antibodies bind to the virus, preventing it from entering and infecting healthy cells. This binding is a crucial part of the immune system’s strategy to eliminate the threat of the virus.
Comparison of Immune Responses to Different COVID-19 Vaccines
| Vaccine | Immune Response Mechanism | Typical Side Effects |
|---|---|---|
| mRNA Vaccine | Induces production of viral spike protein to trigger immune response | Soreness, fever, fatigue |
| Viral Vector Vaccine | Uses a harmless virus to deliver genetic material | Soreness, fatigue, mild fever |
The table above highlights the different approaches used by mRNA and viral vector vaccines to elicit an immune response. The resulting immune response and side effects can vary slightly, but both types of vaccines are highly effective in generating protection against COVID-19.
Conclusive Thoughts
In conclusion, understanding the timing, severity, and duration of COVID-19 vaccination side effects empowers you to prepare for potential symptoms and know when to seek medical attention. By considering individual factors and the specific vaccine, you can better manage your expectations and ensure a smooth post-vaccination experience. Remember, while side effects are common, they are generally mild and temporary.
If you have any concerns, always consult your doctor.