Can you outgrow asthma? This question sparks curiosity and concern for many, especially parents of young children. Understanding the complexities of asthma is key to navigating this condition, whether it’s a lifelong companion or a temporary visitor. From its various triggers and symptoms to potential treatments and long-term outlook, this exploration aims to demystify asthma and answer the crucial question of whether it can be outgrown.
Asthma, a chronic respiratory condition, affects millions worldwide. Its impact varies greatly depending on factors like age, lifestyle, and environmental triggers. While some individuals may experience remission or improved control over time, understanding the nuances of asthma progression and management is vital for maintaining overall health and well-being.
Understanding Asthma
Asthma is a chronic respiratory condition that affects millions worldwide. It’s characterized by inflammation and narrowing of the airways, making breathing difficult. This inflammation can be triggered by various factors, leading to symptoms ranging from mild discomfort to life-threatening episodes. Understanding asthma is crucial for effective management and prevention of its various complications.Asthma’s impact extends beyond just the respiratory system, affecting overall quality of life and potentially leading to long-term health concerns.
Its unpredictable nature and varying severity require careful attention to triggers, symptoms, and the unique ways it manifests in different individuals.
Asthma Triggers
Understanding the triggers that initiate an asthma attack is essential for preventative measures. Exposure to certain environmental factors can provoke inflammation in the airways, leading to the characteristic symptoms.
- Allergens: Substances like pollen, dust mites, pet dander, mold, and certain foods can trigger allergic reactions, which can manifest as asthma symptoms. For example, a child with a dust mite allergy might experience wheezing and shortness of breath when spending time in a dusty environment.
- Irritants: Certain substances, such as smoke (cigarette smoke, wood smoke), strong odors (perfumes, cleaning products), and air pollution, can irritate the airways and induce asthma symptoms. Exposure to these irritants can cause immediate reactions in susceptible individuals.
- Respiratory Infections: Viral infections, such as the common cold or the flu, can sometimes trigger asthma attacks in susceptible individuals. The body’s response to these infections can inflame the airways, making breathing more difficult.
- Exercise: Physical exertion can sometimes trigger asthma symptoms, especially in individuals with poorly controlled asthma. The increased breathing rate and demand on the lungs can lead to airway narrowing in some cases. This is often referred to as exercise-induced bronchospasm.
- Medications: Certain medications, such as aspirin or nonsteroidal anti-inflammatory drugs (NSAIDs), can sometimes trigger asthma attacks in susceptible individuals. It’s crucial to consult with a doctor if you suspect a medication is causing your asthma symptoms.
Asthma Symptoms
Asthma symptoms vary in severity and duration. Recognizing these symptoms is vital for prompt intervention and appropriate treatment.
- Wheezing: A whistling sound during breathing, particularly during exhalation. This is a common sign of airway narrowing.
- Shortness of Breath: Difficulty breathing, often accompanied by a feeling of tightness in the chest. This symptom can range from mild discomfort to severe distress.
- Chest Tightness: A sensation of pressure or constriction in the chest, often accompanied by shortness of breath. This can be a prominent symptom during an asthma attack.
- Coughing: A persistent cough, especially at night or early in the morning. This can be a dry or productive cough, depending on the underlying cause.
Asthma Types
Asthma can manifest in various forms, each requiring specific management strategies.
- Allergic Asthma: This type is often triggered by allergens such as pollen, dust mites, or pet dander. The immune system’s response to these allergens leads to inflammation and narrowing of the airways.
- Non-allergic Asthma: This type of asthma is not associated with allergies and can be triggered by irritants, infections, or exercise.
Asthma in Different Age Groups
Asthma can affect individuals at any age, though its presentation and management can differ based on developmental stages.
- Infants and Children: Asthma in young children can manifest with frequent coughing, wheezing, and difficulty breathing, particularly during nighttime. Recognition and management are critical in preventing long-term complications.
- Adolescents: Asthma in adolescents may exhibit symptoms similar to adults, but they can also present with challenges related to adherence to treatment plans and lifestyle choices.
- Adults: Asthma in adults can be a chronic condition, often requiring long-term management and monitoring. Understanding triggers and maintaining adherence to prescribed medications are essential.
Asthma Progression
Asthma symptoms can vary significantly over time, from occasional episodes to persistent and severe conditions. Careful monitoring and proactive management are key to minimizing the impact of asthma.
Genetic and Environmental Factors
A combination of genetic predisposition and environmental factors contributes to asthma development. These factors interact in complex ways, influencing the severity and progression of the condition.
Asthma Diagnosis
Asthma diagnosis involves a combination of medical history evaluation, physical examination, and diagnostic tests. This comprehensive approach allows for an accurate assessment of the condition and appropriate management.
- Spirometry: This lung function test measures the amount of air a person can inhale and exhale, providing insights into airway obstruction.
- Allergy Testing: Identifying specific allergens can help pinpoint potential triggers for asthma symptoms.
Factors Influencing Asthma Progression
Asthma, a chronic respiratory condition, is not a static entity. Its progression and severity can be significantly impacted by various interconnected factors. Understanding these influences is crucial for effective asthma management and improving long-term outcomes. This exploration will delve into how lifestyle choices, treatment modalities, environmental factors, and mental health can shape the course of asthma.Lifestyle choices, treatment approaches, environmental exposures, and mental well-being are all key elements that play a dynamic role in the ongoing management of asthma.
These factors are not isolated; they interact and influence each other in complex ways. Recognizing these interactions is vital for optimizing asthma control and preventing exacerbations.
Lifestyle Choices and Asthma Control
Lifestyle choices exert a considerable influence on asthma management. Dietary habits, physical activity levels, and stress management techniques can all contribute to the overall control of asthma symptoms. A balanced diet rich in fruits, vegetables, and whole grains can potentially contribute to improved lung function and reduced inflammation. Regular physical activity, while potentially triggering symptoms in some individuals, can strengthen lung capacity and improve overall health, which can positively affect asthma control.
Furthermore, incorporating stress-reduction techniques like meditation or yoga may help manage anxiety and stress, both of which can exacerbate asthma symptoms.
Asthma Treatments and Their Impact on Growth
Various treatment approaches are available for asthma, each with its own potential impact on growth and development. Inhaled corticosteroids are a cornerstone of asthma treatment, known for their effectiveness in reducing inflammation in the airways. While generally considered safe and effective, long-term use of high-dose inhaled corticosteroids may potentially affect growth in some individuals. The potential impact on growth varies depending on the individual’s age, dosage, and overall health.
Leukotriene modifiers, another class of asthma medications, can help control inflammation and reduce symptoms, but their effect on growth remains less well-studied. Regular monitoring and communication with a healthcare provider are essential to address any potential concerns about growth.
Comparison of Treatment Approaches over Time
The efficacy of different asthma treatment approaches can vary over time, and a personalized approach is often necessary. For instance, inhaled corticosteroids have consistently demonstrated efficacy in controlling inflammation and reducing asthma exacerbations. However, the optimal approach may evolve as an individual’s asthma progresses or their response to treatment changes. The long-term effectiveness of a particular treatment strategy should be regularly assessed and adjusted based on the patient’s specific needs.
This personalized approach is crucial for maintaining asthma control throughout different life stages.
Environmental Factors and Asthma Management
Environmental factors play a significant role in asthma management. Exposure to allergens like pollen, dust mites, or pet dander can trigger asthma symptoms. Controlling indoor allergens through measures like using air purifiers, controlling humidity levels, and regularly cleaning can significantly improve asthma control. Outdoor air pollution, particularly particulate matter and ozone, has also been linked to increased asthma symptoms.
Reducing exposure to these pollutants through awareness and proactive measures is essential for effective asthma management.
Stress and Mental Health’s Influence on Asthma Symptoms
Stress and mental health conditions can significantly impact asthma symptoms. Chronic stress can trigger or worsen asthma symptoms by increasing inflammation and airway reactivity. Mental health conditions such as anxiety and depression can also contribute to the severity and frequency of asthma attacks. Effective management of stress and mental health conditions is essential for optimizing asthma control.
Interventions such as stress-reduction techniques, therapy, and medication, when appropriate, can help individuals better manage their mental well-being and consequently improve their asthma outcomes.
Outgrowing Asthma
Asthma, a chronic respiratory condition, often presents significant challenges for individuals, particularly children. While it frequently persists throughout life, some individuals experience remission or significant improvement over time. Understanding the factors contributing to this phenomenon can provide valuable insights and reassurance.Asthma’s manifestation can differ greatly between childhood and adulthood. The triggers, severity, and treatment responses can vary, making a nuanced approach crucial.
The ability to outgrow asthma is a complex interplay of genetic predispositions, environmental factors, and lifestyle choices.
Conditions for Asthma Remission
Asthma remission, or the lessening or disappearance of asthma symptoms, is not guaranteed, but certain conditions can influence its likelihood. Factors like consistent adherence to medication regimens, effective environmental control, and a reduction in exposure to asthma triggers play crucial roles. Furthermore, a gradual decrease in airway inflammation over time can contribute to symptom reduction.
Comparison of Asthma in Children and Adults
Asthma in children often presents with different characteristics compared to adult-onset asthma. Children might experience more frequent exacerbations and display a higher sensitivity to environmental allergens. Adults, on the other hand, might experience more chronic symptoms and a greater predisposition to occupational or irritant-induced asthma. Recognizing these differences is vital for personalized treatment strategies.
Factors Contributing to Asthma Remission or Improvement
Several factors can contribute to asthma remission or improvement. These include a reduced exposure to environmental allergens, a positive response to medications, and lifestyle modifications that include regular exercise, a healthy diet, and stress management. Early diagnosis and appropriate intervention also play a pivotal role in managing asthma and potentially leading to remission.
- Reduced Exposure to Allergens: Controlling environmental allergens, such as dust mites, pet dander, and pollen, can significantly lessen asthma symptoms. This is often achieved through measures such as using allergen-proof bedding, regularly cleaning, and using air purifiers.
- Positive Response to Medications: Effective asthma medications, including inhaled corticosteroids, long-acting bronchodilators, and leukotriene modifiers, can reduce inflammation and improve lung function. Consistent use of these medications is essential for managing asthma symptoms and potentially achieving remission.
- Lifestyle Modifications: Adopting a healthy lifestyle that includes regular exercise, a balanced diet, and stress management techniques can contribute to overall well-being and potentially improve asthma control. Regular physical activity can strengthen the respiratory system and improve lung function.
Examples of Individuals Experiencing Asthma Remission
While definitive data on the percentage of individuals who outgrow asthma is not readily available, anecdotal evidence suggests that remission can occur. Many individuals who experienced asthma remission in childhood have maintained good lung health in adulthood, with symptoms controlled with minimal medication. Such cases highlight the complex interplay of factors that can lead to asthma improvement or remission.
Wondering if you can outgrow asthma? While some conditions do resolve, it’s not always the case. Interestingly, there’s a similar question around managing Irritable Bowel Syndrome (IBS) – a lot of people search for remedies like pepto bismol for ibs here. Ultimately, whether you can outgrow asthma depends on individual factors and the severity of the condition.
Consulting a doctor is always the best first step for personalized advice.
Regular Check-ups and Monitoring
Regular check-ups and monitoring are crucial for managing asthma and potentially influencing its progression. These visits allow healthcare providers to assess lung function, evaluate medication effectiveness, and adjust treatment plans as needed. This proactive approach can help identify and address potential problems early, thereby potentially improving long-term asthma outcomes. Early detection of exacerbations can also prevent severe complications.
Management and Prevention

Asthma management is crucial for maintaining a healthy life. Effective strategies, encompassing trigger avoidance and appropriate medication use, significantly reduce the frequency and severity of asthma attacks. Proactive steps can empower individuals to better control their condition and improve their overall well-being.
Common Asthma Triggers and Avoidance Strategies
Understanding asthma triggers is essential for effective management. Identifying and avoiding these triggers can significantly reduce the risk of asthma attacks.
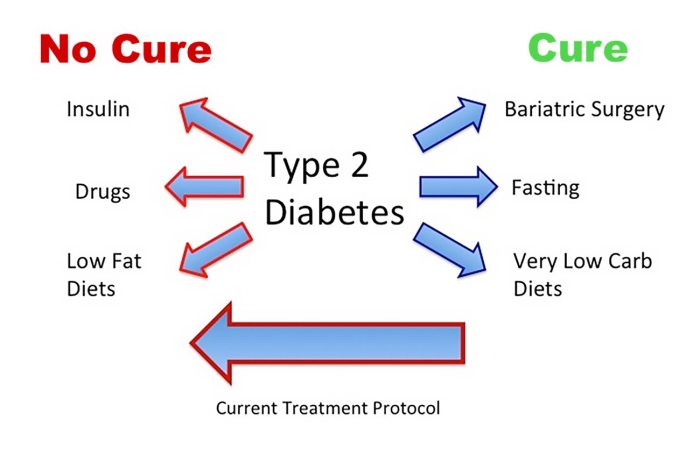
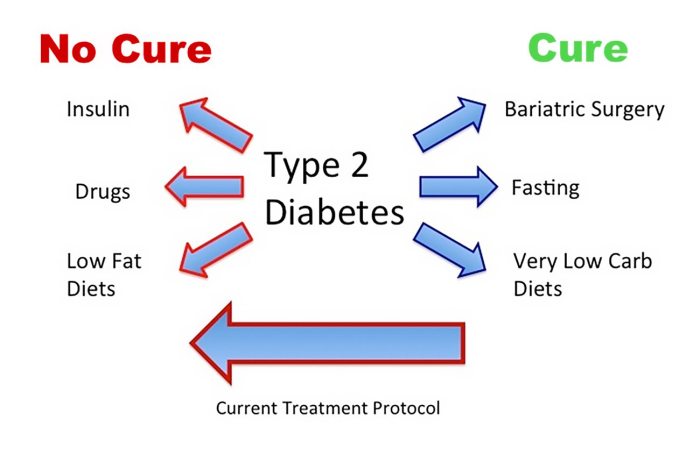
While some childhood conditions like asthma can sometimes improve or even disappear over time, it’s not a guaranteed outcome. Interestingly, research into natural remedies like the potential efficacy of cinnamon for diabetes treatment efficacy of cinnamon for diabetes treatment shows promising results in some cases. Ultimately, whether or not you “outgrow” asthma depends on individual factors and medical guidance.
| Trigger | Avoidance Strategies |
|---|---|
| Dust mites | Regularly wash bedding in hot water, use allergen-proof covers, and vacuum frequently. |
| Pet dander | Keep pets out of bedrooms, bathe pets regularly, and use air purifiers. |
| Mold | Address moisture problems in the home, use dehumidifiers, and avoid areas with visible mold. |
| Pollen | Monitor pollen counts and avoid outdoor activities during high pollen seasons. Wear a mask when necessary. |
| Smoke (cigarette, wood, etc.) | Avoid exposure to smoke, and ensure proper ventilation in areas where smoking occurs. |
| Cold air | Dress warmly, especially during winter, and use a scarf or mask to warm the air inhaled. |
| Respiratory Infections | Practice good hygiene, avoid close contact with infected individuals, and get vaccinated. |
| Strong Odors/Chemicals | Ventilate areas where strong odors or chemicals are used, and use appropriate protective gear when necessary. |
| Exercise | Warm up before exercise and use an inhaler as directed before strenuous activity. |
Comparison of Asthma Medications
Different asthma medications work in various ways to control symptoms. Understanding their differences helps in choosing the most suitable treatment plan.
| Medication Type | Mechanism of Action | Examples | Potential Side Effects |
|---|---|---|---|
| Quick-relief inhalers (bronchodilators) | Quickly open airways to relieve sudden symptoms. | Albuterol, Levalbuterol | Mild tremors, nervousness, headache, and sometimes rapid heart rate. |
| Long-acting controllers | Reduce inflammation and prevent long-term symptoms. | Inhaled corticosteroids, Leukotriene modifiers | Inhaled corticosteroids: potential for oral thrush (yeast infection in the mouth), difficulty swallowing. Leukotriene modifiers: possible stomach upset or headache. |
| Combination inhalers | Combine quick-relief and long-acting medications in one device. | Various combinations | May combine potential side effects of both types of medication. |
| Oral medications | Reduce inflammation systemically. | Theophylline, montelukast | Potential for significant side effects, depending on the medication and dosage. |
Common Asthma Symptoms and Potential Causes
Recognizing asthma symptoms and their potential triggers helps in prompt diagnosis and treatment.
| Symptom | Potential Causes |
|---|---|
| Wheezing | Narrowing of the airways, often triggered by allergens or irritants. |
| Shortness of breath | Difficulty breathing due to restricted airflow, often related to inflammation and constriction of airways. |
| Chest tightness | Inflammation of the airways, leading to a feeling of pressure or constriction in the chest. |
| Coughing | Irritation and inflammation of the airways, often triggered by allergens, irritants, or respiratory infections. |
Steps to Take if Asthma Symptoms Worsen
A worsening asthma condition necessitates immediate action.
| Step | Action |
|---|---|
| Assess the severity | Determine if symptoms are mild, moderate, or severe. |
| Use quick-relief inhaler | Administer the prescribed dose as directed. |
| Monitor symptoms | Pay close attention to how symptoms respond to the medication. |
| Seek medical attention | If symptoms do not improve or worsen, contact a doctor or emergency services immediately. |
Managing Asthma Triggers in Different Environments
Effective asthma management involves tailoring strategies to specific environments.
Home
Maintain a clean and dust-free environment. Use air purifiers and dehumidifiers to control allergens. Keep pets out of bedrooms. Avoid strong odors and chemicals.
School
Communicate with teachers and school staff about asthma. Have an action plan readily available. Avoid areas with high allergen concentrations. Ensure access to quick-relief inhalers.
Public Spaces
Be aware of potential triggers in public spaces, such as air quality and allergens. Use personal protective measures, like masks. Identify areas with potential triggers and plan accordingly.
Potential Complications and Considerations

Asthma, if not properly managed, can lead to a range of complications impacting quality of life and overall health. Understanding these potential consequences is crucial for developing effective strategies for prevention and treatment. A proactive approach, emphasizing early intervention and consistent management, is vital in minimizing the risk of these complications.Poorly managed asthma can significantly impact daily life, leading to decreased productivity and overall well-being.
This is often due to frequent exacerbations and the resulting symptoms, such as shortness of breath and coughing. Recognizing the link between asthma and other health conditions is also essential for comprehensive care.
While some childhood conditions like asthma can improve or even disappear, it’s not a guarantee you’ll outgrow it. Factors like genetics and environmental triggers play a significant role. Understanding the potential causes of high blood pressure, which can sometimes be related to underlying health conditions, is crucial in managing overall health. For more information on high blood pressure causes, check out this helpful resource: high blood pressure causes.
Ultimately, whether or not you outgrow asthma depends on individual circumstances and ongoing medical care.
Potential Complications from Poorly Managed Asthma
Uncontrolled asthma can result in various complications. These include frequent hospitalizations due to severe asthma attacks, and long-term lung damage, potentially leading to chronic obstructive pulmonary disease (COPD). Untreated asthma can also increase the risk of developing other respiratory conditions.
Link Between Asthma and Other Health Conditions
Asthma is often linked with other health issues. For instance, individuals with uncontrolled asthma may experience heightened anxiety and depression due to the frequent and unpredictable nature of their symptoms. Asthma can also negatively affect cardiovascular health, increasing the risk of heart problems. Further research is needed to fully understand the complex interplay between these conditions.
Impact of Uncontrolled Asthma on Daily Activities
Uncontrolled asthma can significantly limit daily activities. A person might miss school or work due to frequent asthma attacks. Even simple tasks, like playing with children or engaging in hobbies, can become challenging. This can lead to social isolation and reduced quality of life. For example, an athlete struggling with poorly managed asthma may not be able to train or compete effectively, impacting their athletic performance and aspirations.
Role of Preventative Measures in Minimizing Exacerbations
Implementing preventative measures is crucial in minimizing asthma exacerbations. These measures include avoiding known triggers, such as allergens or irritants, and adhering to a prescribed medication regimen. Furthermore, regular monitoring of symptoms and prompt treatment of early warning signs are key. Recognizing and avoiding triggers can greatly reduce the frequency and severity of attacks.
Importance of Early Intervention and Consistent Management
Early intervention and consistent management play a pivotal role in preventing severe complications associated with asthma. By promptly identifying and addressing asthma triggers, and by diligently following prescribed treatment plans, individuals can significantly reduce the likelihood of severe attacks and long-term health issues. Early intervention is critical because it helps to establish healthy habits and effective management strategies, which will positively impact the patient’s life in the long run.
For example, early diagnosis and treatment can significantly reduce the need for emergency room visits and hospitalizations. Consistent medication adherence and avoidance of known triggers will enable better long-term control.
Long-Term Outlook and Prognosis
Living with asthma doesn’t mean a life sentence of constant struggle. A well-managed approach can significantly impact the long-term outlook and prognosis, leading to a fulfilling and active life. Understanding the potential variations and factors that influence long-term management is crucial for individuals with asthma and their healthcare providers.Asthma’s long-term trajectory is not a one-size-fits-all scenario. While some individuals may experience relatively mild symptoms and infrequent flare-ups, others may face more challenging periods of worsening symptoms and increased healthcare needs.
Factors such as the severity of initial symptoms, adherence to treatment plans, and the presence of other health conditions all contribute to the individual’s unique long-term experience.
Factors Influencing Long-Term Asthma Management
Effective long-term asthma management relies on a combination of factors. Consistent adherence to prescribed medications, regular monitoring of symptoms, and proactive communication with healthcare providers are vital. Early intervention for worsening symptoms is key to preventing more serious complications.
Lifestyle Changes for Improved Asthma Control
Lifestyle modifications can significantly improve long-term asthma control. A balanced diet rich in fruits, vegetables, and whole grains can contribute to overall health and well-being, potentially impacting asthma management. Regular physical activity, while carefully managed to avoid triggers, can enhance lung function and overall health. Stress management techniques, such as mindfulness or yoga, can help minimize the impact of stress on asthma symptoms.
Avoiding known triggers, like smoke or allergens, is also crucial.
Creating a Long-Term Asthma Management Plan, Can you outgrow asthma
Developing a comprehensive plan for monitoring and managing asthma over time is essential. This plan should include a detailed record of symptoms, triggers, and medication responses. Regular check-ups with healthcare providers are crucial for adjusting treatment plans as needed. The plan should incorporate strategies for managing potential flare-ups and emergency situations. A detailed asthma action plan, including specific actions to take during different symptom levels, is a valuable tool.
Planning for Potential Future Needs and Complications
Anticipating potential future needs and complications is an important part of long-term asthma management. Regular communication with healthcare providers can help identify and address potential problems early on. Having a clear understanding of available resources, such as support groups or educational materials, can also be helpful. For example, individuals with severe asthma may need to consider long-term care options or accommodations to ensure their safety and well-being.
Preparing for potential exacerbations, such as hospitalizations, is an important part of the overall management strategy.
Ending Remarks: Can You Outgrow Asthma
Ultimately, the answer to “can you outgrow asthma” isn’t a simple yes or no. While some experience remission, asthma remains a chronic condition for many. This discussion highlighted the importance of understanding the factors influencing asthma progression, the role of lifestyle choices, and the crucial role of consistent medical care. Ultimately, proactive management and a deep understanding of individual needs are essential for navigating the long-term journey with asthma.