The benefits of mullein, a versatile plant with a rich history, are explored in this comprehensive guide. From its medicinal properties to traditional uses and modern research, we’ll uncover the many ways this plant can contribute to well-being. Discover how mullein has been used for centuries and whether modern science supports its purported advantages.
This in-depth look at mullein will cover everything from its botanical classification and historical context to detailed information on cultivation and potential side effects. Learn about the different types of mullein, their variations, and how they’ve been employed in various cultures throughout history. We’ll also discuss modern scientific research and safety precautions.
Introduction to Mullein
Mullein, a diverse group of flowering plants, holds a rich history of medicinal and practical applications. This versatile genus, belonging to the family Lamiaceae, encompasses a range of species, each exhibiting unique characteristics. From ancient remedies to modern herbal practices, mullein’s uses have transcended cultures and time periods. Understanding its various types and historical context provides a deeper appreciation for this remarkable plant.The common thread linking the different types of mullein is their remarkable ability to adapt to various environments.
This adaptability is reflected in their morphology, ranging from size to leaf structure. Furthermore, the specific environmental conditions often determine the variations in the plant’s appearance, growth patterns, and even medicinal properties.
Mullein’s got some impressive medicinal properties, like soothing coughs and easing respiratory issues. But if you’re concerned about skin cancers like melanoma, understanding the LDH test is crucial. Checking out this guide to the LDH test for melanoma will give you a clearer picture of how this blood marker is used in diagnosis. Ultimately, though, mullein remains a valuable natural remedy for various ailments.
Botanical Classification
Mullein plants are classified within the Lamiaceae family, a large and diverse group of flowering plants known for their medicinal and culinary uses. This classification places them alongside other well-known herbs and spices, reflecting their inherent medicinal potential.
Different Types of Mullein and Their Variations
Several species fall under the mullein genus, each exhibiting distinct traits. These differences stem from environmental factors, genetic makeup, and evolutionary pressures. The variations in size, leaf structure, and flowering patterns contribute to the overall diversity within the mullein family.
Historical Uses Across Cultures
Mullein’s historical use extends across diverse cultures, highlighting its recognized medicinal value. In traditional European practices, mullein was valued for its potential to alleviate respiratory ailments. Indigenous cultures also employed mullein for various purposes, including wound healing and treating inflammation. This wide-ranging application underscores the plant’s historical significance.
Common Names in Various Languages
The common names for mullein vary considerably across languages, reflecting its global recognition. Different communities have adapted their names based on the plant’s characteristics or its cultural significance. Understanding these diverse names provides insight into the global appreciation for mullein.
Mullein Species Overview
| Common Name | Scientific Name | Image Description |
|---|---|---|
| Common Mullein | Verbascum thapsus | A tall, robust plant reaching up to 5 feet in height. Its leaves are lanceolate and grow in a rosette pattern. The flowers are clustered in a dense spike, typically yellow or light brown, and have a fuzzy appearance. |
| Moth Mullein | Verbascum blattaria | A smaller plant, typically 1-3 feet tall. The leaves are oval-shaped and slightly hairy. The flowers are a deep yellow and clustered into a compact spike. |
| Hairy Mullein | Verbascum densiflorum | A shorter mullein species, often less than 2 feet in height. Its leaves are densely hairy, giving it a velvety texture. The flowers are yellowish-brown and arranged in a dense spike. |
Medicinal Properties of Mullein
Mullein, a common weed found in various parts of the world, has a long history of traditional medicinal use. Its purported healing properties are attributed to a variety of compounds within its different parts, including leaves, flowers, and roots. While scientific research is ongoing, numerous anecdotal accounts and traditional practices suggest potential benefits for various ailments.This exploration delves into the medicinal properties of mullein, focusing on the active compounds, different plant parts utilized, and potential applications for specific health concerns.
We’ll also touch upon potential variations in benefits between mullein species.
Active Compounds and Their Potential Effects
Mullein contains a range of compounds that may contribute to its purported medicinal effects. These include saponins, which are known for their potential anti-inflammatory properties; flavonoids, which have antioxidant and anti-inflammatory properties; and mucilage, a type of viscous carbohydrate that has been used for soothing and lubricating purposes. The presence of these compounds suggests potential benefits for respiratory conditions, skin irritations, and other ailments.
Parts of the Mullein Plant Used
Different parts of the mullein plant are traditionally used for various purposes. The leaves are often used for their purported medicinal properties, while the flowers, particularly the dried ones, are valued for their soothing and potentially expectorant qualities. The roots, while less commonly used, may also possess specific medicinal properties. The varying properties of these parts contribute to the diverse applications of mullein.
Comparison of Mullein Species
While most of the medicinal properties are generally attributed to all mullein species, there may be subtle differences in the concentration of active compounds. Further research is needed to determine the precise variations. The potential benefits generally remain similar across various species, but potential differences are worthy of note.
Potential Applications for Different Ailments
The following table Artikels potential applications of mullein for different ailments, based on traditional uses and available research. It’s important to note that this information is not a substitute for professional medical advice.
| Ailment | Part of Mullein Used | Method of Preparation |
|---|---|---|
| Cough and Bronchitis | Flowers, leaves | Infusion (steep dried flowers or leaves in hot water) |
| Sore Throat | Flowers, leaves | Gargle with an infusion or apply a poultice of crushed leaves to the throat. |
| Skin Irritations | Leaves | Apply a poultice of crushed leaves to the affected area. |
| Burns | Leaves | Apply a poultice of crushed leaves to the affected area. |
| Headaches | Leaves, Flowers | Apply a poultice of crushed leaves or flowers to the forehead. |
Traditional Uses and Practices
Mullein, a humble plant often overlooked, has held a significant place in traditional medicine for centuries. Its medicinal properties have been recognized and utilized across various cultures, leading to a rich tapestry of traditional uses and practices. These practices highlight the plant’s versatility and the deep understanding of its potential benefits by those who came before us.Traditional healers and communities have long valued mullein for its diverse applications, recognizing its ability to soothe and heal.
Their understanding of the plant’s unique properties and their careful observation of its effects have shaped the evolution of its use in various cultures.
Examples of Traditional Medicinal Uses
Mullein’s versatility extends to a wide range of ailments. Its soothing properties have traditionally been harnessed to address respiratory issues, skin conditions, and more. Early healers discovered that the plant’s compounds could effectively combat inflammation and provide relief from discomfort.
Preparation Methods in Traditional Medicine
Traditional preparation methods for mullein varied greatly, reflecting the diverse knowledge and resources available in different communities. These methods often involved using fresh or dried plant material, adapted to the specific needs and resources of each culture. These varied techniques, while not always scientifically documented, demonstrate a deep understanding of the plant’s properties and how to best extract its medicinal potential.
- Infusion: Steeping dried mullein leaves in hot water created a soothing tea, commonly used for respiratory ailments. The warm liquid, infused with the plant’s constituents, was believed to ease congestion and promote better breathing. The precise duration of steeping and the amount of water used likely varied among different communities, reflecting their individual knowledge and experiences.
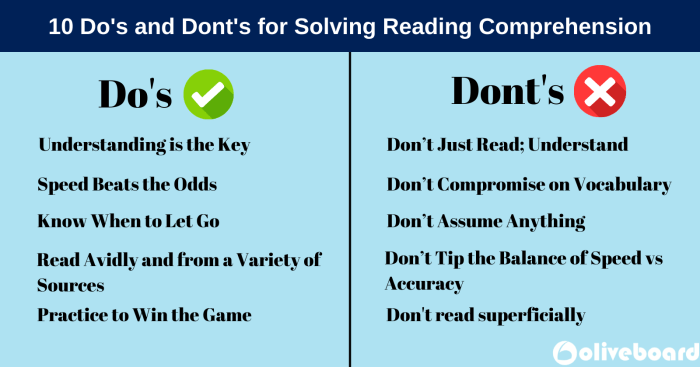
Mullein, a surprisingly versatile plant, boasts some impressive healing properties. Knowing the proper dos and don’ts when you’re under the weather is crucial, and following guidelines like those found on dos donts when sick can help you recover faster. This ancient remedy, when used correctly, can soothe coughs and congestion, making it a fantastic natural ally during illness.
It’s important to remember that mullein should be used as part of a holistic approach to wellness.
- Poultices: A paste made from mullein leaves or flowers, applied directly to the skin, was a popular method for treating various skin conditions. The poultice’s gentle properties likely eased inflammation and discomfort, providing relief for ailments like burns, sores, and rashes. The consistency of the poultice and the addition of other ingredients would have been influenced by local traditions and available resources.
- Ointments and Salves: In some cultures, mullein was incorporated into ointments and salves for topical application. The extracted compounds were combined with other natural ingredients, often creating a medicated salve that was applied to wounds, sprains, or other skin ailments. These practices likely relied on local knowledge and understanding of the plant’s effects, and the exact composition of these preparations would have varied depending on the culture.
Mullein, a fascinating plant, boasts a surprising array of potential health benefits. Its traditional use often centers around respiratory issues, and understanding how it might interact with conditions like primary lung cancer is crucial. Learning about the specifics of what is primary lung cancer helps contextualize the potential benefits of mullein, particularly for those looking for natural approaches to respiratory health.
Ultimately, though, more research is needed to fully understand its effects, and always consult a medical professional before incorporating any new supplement into your routine.
Cultural Significance of Mullein
The use of mullein in traditional medicine often intertwined with the cultural beliefs and practices of the communities that utilized it. Its presence in rituals and ceremonies, its association with specific deities or spirits, and its incorporation into healing practices reflected the cultural significance and importance placed upon the plant.
Traditional Uses Across Different Cultures
The following table provides a glimpse into the diverse applications of mullein across various cultures, showcasing the plant’s enduring role in traditional medicine.
| Culture | Use | Preparation Method |
|---|---|---|
| Indigenous American Tribes (various) | Respiratory ailments, skin conditions | Infusion, poultices, and potentially incorporated into other remedies |
| European Herbalists | Cough, bronchitis, skin conditions, wounds | Infusion, poultices, and salves |
| Traditional Chinese Medicine | (Limited evidence of direct use of mullein, but similar plants with similar properties) Respiratory ailments, skin conditions | Potential incorporation into complex herbal formulas |
| African Traditional Medicine (specific examples needed) | (Specific uses require further research) | Varied methods depending on specific communities |
Safety and Precautions
While mullein offers potential health benefits, it’s crucial to approach its use with caution. Like any herbal remedy, mullein can have side effects and may interact with other medications. Understanding these potential risks and precautions is essential for safe and effective use.Thorough research and consultation with a healthcare professional are vital before incorporating mullein into any treatment plan.
This section will Artikel potential side effects, interactions, and precautions to ensure responsible use.
Potential Side Effects, The benefits of mullein
Mullein, while generally considered safe, can cause adverse reactions in some individuals. These reactions can vary in severity and range from mild discomfort to more serious complications. Understanding the potential side effects helps users make informed decisions.
Possible Interactions with Medications
Mullein can interact with certain medications, potentially altering their effectiveness or increasing the risk of side effects. For example, mullein might influence the liver’s ability to process medications, leading to unexpected outcomes. Careful consideration is necessary when combining mullein with prescription or over-the-counter drugs.
Precautions for Pregnant and Breastfeeding Women
Pregnant and breastfeeding women should exercise extreme caution when using mullein. The effects of mullein on a developing fetus or nursing infant are not fully understood. Consult a healthcare professional before using mullein during pregnancy or while breastfeeding.
When to Consult a Healthcare Professional
If you experience any unusual symptoms after using mullein, such as allergic reactions, severe digestive issues, or changes in your overall health, contact a healthcare professional immediately. This is especially important if you have underlying health conditions or are taking other medications. Professional guidance is essential for addressing potential complications.
Table of Potential Side Effects and Precautions
| Side Effect | Cause | Precaution |
|---|---|---|
| Allergic Reactions (hives, rash, itching) | Hypersensitivity to mullein components | Discontinue use immediately and seek medical attention if symptoms worsen. |
| Gastrointestinal Upset (nausea, vomiting, diarrhea) | Potential irritation of the digestive tract | Use mullein in moderate doses and with food. Stop use if symptoms persist. |
| Liver Dysfunction | Possible interaction with other medications or high doses of mullein | Consult a healthcare professional before using mullein if you have liver problems or are taking other medications. |
| Skin Irritation | Direct contact with mullein plant material | Use caution when handling mullein. Wear gloves if necessary. |
| Interactions with Medications | Mullein’s potential to alter the metabolism of other drugs | Inform your doctor about all medications and supplements you are taking before using mullein. |
| Uncertain Effects on Pregnancy and Breastfeeding | Limited research on effects during pregnancy and breastfeeding | Avoid using mullein during pregnancy or breastfeeding unless advised by a healthcare professional. |
Growing and Harvesting Mullein
Mullein, a versatile medicinal plant, thrives in various environments. Understanding its growing needs and harvesting practices is crucial for obtaining high-quality, potent extracts. Proper cultivation and harvesting methods ensure the plant’s health and the efficacy of its medicinal properties.
Optimal Growing Conditions
Mullein is a robust plant, adaptable to a range of conditions. It prefers well-drained soil, but tolerates a variety of compositions. Full sun exposure is ideal, though mullein can survive in partial shade. The plant is drought-tolerant once established, but consistent moisture during its early growth phase promotes healthy development. A slightly acidic soil pH (6.0-7.0) is generally beneficial.
Best Time to Harvest
For optimal medicinal benefits, harvest mullein during the plant’s flowering stage. This is when the plant’s concentration of active compounds is highest. The specific timing may vary slightly depending on the region and the weather conditions. Early morning is often recommended for harvesting, as this is when the plant’s constituents are at their peak concentration.
Proper Harvesting Techniques
Carefully cut the flowering stalks, leaving the base of the plant intact. This allows the plant to regenerate and produce new growth. Avoid excessive harvesting, which can weaken the plant and diminish its overall health.
Storing Harvested Mullein
Proper storage is essential for preserving the quality and potency of the harvested mullein. Store the dried leaves and flowers in airtight containers in a cool, dark, and dry place. Avoid exposure to direct sunlight and high humidity, as these can degrade the plant’s medicinal properties. Freezing is also an option, ensuring the integrity of the plant material.
Step-by-Step Guide for Growing and Harvesting Mullein
- Seed Starting: Sow mullein seeds directly into the ground in spring or start them indoors 6-8 weeks before the last expected frost. Ensure the soil is well-prepared and lightly moist. A seed starting mix is recommended for optimal germination. Cover the seeds lightly with soil and keep the area consistently moist until germination occurs. Thin seedlings to allow for proper space.
This ensures adequate space for the plants to grow. A healthy plant starts with good care in its early stages.
- Planting: Transplant seedlings or direct-sown seeds to their final location after all danger of frost has passed. Choose a sunny location with well-drained soil. Space plants about 18-24 inches apart to allow for ample growth. Water consistently, especially during dry periods, until the plants are established. The plants will be more resistant to drought once established.
- Watering: Consistent watering is essential for young plants. Water deeply and less frequently, allowing the soil to dry slightly between waterings. Once established, mullein is drought-tolerant. Regular watering is needed during the initial stages of growth.
- Fertilizing: If necessary, a balanced fertilizer can be applied in spring to enhance growth. Use a low-nitrogen fertilizer to promote healthy development. Too much nitrogen can lead to excessive foliage growth and reduce the concentration of medicinal compounds. Avoid over-fertilizing.
- Monitoring: Watch for pests and diseases. Monitor the plant’s growth and address any issues promptly. Healthy plants are more resilient to pests and diseases. Regular monitoring can prevent serious issues.
- Flowering Stage: Harvest mullein when the flowers begin to bloom. This is the peak time for the medicinal compounds. Cut the flowering stalks carefully, leaving the base of the plant intact. The timing of flowering can vary slightly depending on the specific variety.
- Drying: Hang the harvested stalks upside down in a well-ventilated area, away from direct sunlight. Allow them to air dry completely. This process can take several days to weeks. Drying is crucial for preservation.
- Storage: Store the dried mullein in airtight containers in a cool, dark, and dry place to maintain its potency. Avoid exposure to moisture and sunlight. Storing mullein properly is essential for preserving its medicinal qualities.
Mullein and Other Complementary Therapies

Combining mullein with other complementary therapies can potentially enhance its benefits or introduce potential risks. Understanding the interplay between mullein and various approaches is crucial for informed decision-making. Careful consideration of individual needs and potential interactions is vital when integrating mullein into a broader holistic health plan.A holistic approach to health often involves a combination of therapies. Mullein, with its demonstrated anti-inflammatory and expectorant properties, can complement other therapies that address similar concerns.
However, combining therapies can introduce potential interactions and risks, requiring careful consideration. This section explores potential combinations, emphasizing the importance of professional guidance when implementing these strategies.
Potential Complementary Therapies
Integrating mullein with other complementary therapies requires careful evaluation of potential benefits and risks. A wide range of therapies, from herbal remedies to lifestyle changes, may be considered. Understanding the mechanisms of action of both mullein and the complementary therapy is crucial to predict potential interactions.
Examples of Combined Therapies
Combining mullein with other therapies can offer potential benefits, but potential risks must be assessed. Examples of potential combinations include:
- Herbal Remedies: Combining mullein with other expectorants, such as thyme or eucalyptus, may enhance respiratory support. Using mullein alongside herbs known for immune support, like echinacea or elderberry, might synergistically boost the body’s defense mechanisms.
- Acupuncture: Acupuncture can address various health concerns, potentially complementing mullein’s effects on respiratory or musculoskeletal conditions. The combined approach may promote overall well-being by addressing the root cause of discomfort.
- Homeopathy: Combining mullein with homeopathic remedies could offer a unique approach to treating conditions. The homeopathic remedies are generally considered safe, and their combined use with mullein may enhance the effectiveness of the treatment plan.
- Yoga and Meditation: Yoga and meditation practices can improve overall well-being, potentially complementing the benefits of mullein. The stress reduction and relaxation aspects of these practices might work synergistically with mullein’s ability to support respiratory health.
Potential Benefits and Risks of Combinations
The combined effects of mullein with other therapies are often unpredictable. Potential benefits include enhanced effectiveness, broader therapeutic scope, and a more holistic approach to health. Risks can include interactions between substances, exacerbating existing conditions, and allergic reactions. Individual responses to combinations can vary widely, emphasizing the need for professional guidance.
Combining Mullein with Other Therapies: A Table
The following table provides a simplified overview of potential combinations. This information is not exhaustive and should not be interpreted as medical advice. Always consult with a healthcare professional before combining mullein with any other therapy.
| Complementary Therapy | Method of Combination | Potential Benefits | Potential Risks |
|---|---|---|---|
| Herbal Remedies (e.g., Thyme) | Infusion, topical application | Potentially enhanced respiratory support | Possible allergic reactions, interactions with medications |
| Acupuncture | Simultaneous application | Potentially improved pain relief and overall well-being | Potential for bruising or discomfort at the acupuncture points |
| Homeopathy | Concomitant administration | Potentially enhanced therapeutic effect | Lack of scientific evidence for some combinations |
| Yoga and Meditation | Integrative lifestyle approach | Potentially improved stress reduction, enhanced well-being | Potential for worsening existing conditions if not properly integrated |
Conclusion: The Benefits Of Mullein

In conclusion, mullein’s multifaceted history and potential benefits are remarkable. While further research is always needed, the evidence suggests a plant with significant historical and potential medicinal applications. Understanding its uses, both traditional and modern, and taking necessary precautions is key to harnessing the potential of this remarkable herb safely and effectively. We hope this comprehensive guide empowers you to make informed decisions about incorporating mullein into your life, whether for medicinal purposes, or simply for its historical and cultural significance.