How many carbs on keto? This question is central to understanding and successfully navigating the ketogenic diet. It delves into the nuances of different keto approaches, from calculating your daily carbohydrate allowance to choosing the right foods and tracking your intake effectively. This guide is designed to equip you with the knowledge and tools needed to make informed decisions about your carb intake and maximize your keto journey.
We’ll explore the various types of ketogenic diets, detailing their macronutrient ratios and intended goals. Next, we’ll dive into calculating your personalized carbohydrate allowance, considering factors like body weight and activity level. Furthermore, we’ll examine food sources, tracking methods, and portion control strategies. Finally, we’ll address specific considerations for different populations and provide practical application tips, including meal planning, recipe ideas, and visual representations of meal plans.
Defining Ketogenic Diets
The ketogenic diet, often abbreviated as keto, is a high-fat, moderate-protein, and very-low-carbohydrate eating plan. It’s designed to induce a metabolic state called ketosis, where the body burns fat for energy instead of glucose. This shift in fuel source has numerous potential health benefits, but also requires careful planning and monitoring.The ketogenic diet works by drastically reducing carbohydrate intake.
When carbohydrate intake is severely limited, the body’s glycogen stores deplete. This forces the body to look for alternative energy sources. The liver responds by breaking down fats into molecules called ketones, which can then be used as fuel for the brain and other organs. This process is known as ketosis.
Ketogenic Diet Types
Different variations of the ketogenic diet exist, each with its own approach to macronutrient ratios and intended goals. Understanding these variations helps individuals tailor the diet to their specific needs and preferences.
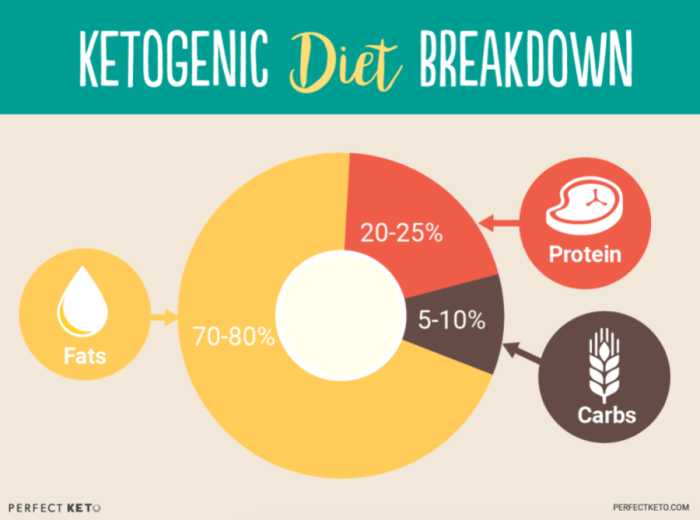
- Standard Ketogenic Diet (SKD): This is the most common form, characterized by a precise macronutrient ratio. It typically involves 70-80% of calories from fat, 15-20% from protein, and 5-10% from carbohydrates.
- Cyclical Ketogenic Diet (CKD): This approach allows for periods of higher carbohydrate intake, typically incorporated into a weekly or bi-weekly cycle. This allows for greater flexibility and potential for increased glycogen stores. It involves alternating high-carbohydrate days with ketogenic days, typically in a cycle.
- Targeted Ketogenic Diet (TKD): This variation allows for some carbohydrates to be consumed around exercise or specific activities. The key is to keep carbohydrate intake below the threshold for glucose to be the primary fuel source. It’s designed for individuals with higher activity levels.
Macronutrient Ratios in Different Ketogenic Approaches
The varying ratios of carbohydrates, protein, and fat in different ketogenic approaches significantly impact their effectiveness and potential outcomes.
| Diet Type | Carbohydrate (%) | Protein (%) | Fat (%) | Intended Goals |
|---|---|---|---|---|
| Standard Ketogenic Diet (SKD) | 5-10% | 15-20% | 70-80% | Weight loss, improved metabolic health, management of certain medical conditions. |
| Cyclical Ketogenic Diet (CKD) | Varying, higher on specific days | 15-20% | 70-80% | Increased glycogen stores, potentially improved athletic performance, and maintaining metabolic flexibility. |
| Targeted Ketogenic Diet (TKD) | 5-10%, potentially higher around exercise | 15-20% | 70-80% | Supporting exercise performance while maintaining ketosis, maintaining lean muscle mass. |
Calculating Carbohydrate Intake
Accurately estimating your daily carbohydrate allowance is crucial for success on a ketogenic diet. It allows you to tailor your macronutrient intake to your specific needs and goals, whether weight loss, improved energy levels, or managing specific health conditions. Understanding the methods and factors involved will empower you to make informed choices and maintain a sustainable ketogenic lifestyle.
Estimating Daily Carbohydrate Needs
A fundamental aspect of keto is the restriction of carbohydrates. To determine your daily carbohydrate allowance, consider factors like your total calorie needs, activity level, and individual metabolic response. Precise calculations provide a personalized approach, which is essential for optimal results.
Methods for Calculating Daily Carbohydrate Allowance
Several methods can be used to estimate your daily carbohydrate allowance. One common approach is to calculate a percentage of your total daily caloric needs. Another involves using a standardized formula based on factors like body weight and activity level.
Figuring out the perfect carb count on keto can be tricky, but it’s definitely manageable. If you’re experiencing shortness of breath when walking, this article might help you understand the underlying causes and solutions. Ultimately, the right amount of carbs on keto is a personalized journey, and you’ll find your ideal balance through experimentation and listening to your body.
Using a Percentage of Total Calories
A popular approach involves calculating a specific percentage of your total daily calorie intake as carbohydrates. For example, a ketogenic diet typically limits carbohydrates to 20-50 grams per day, which represents a small percentage of total calories. A lower percentage often results in a more stringent ketogenic state, while a higher percentage might be more suitable for those with specific metabolic needs.
Figuring out how many carbs to eat on keto can feel tricky, but it’s a crucial part of the process. A key to success, though, is a healthy metabolism. Learning how to boost metabolism can significantly impact your keto journey, helping your body efficiently burn fat. For detailed strategies on how to do that, check out this informative guide on how to boost metabolism.
Ultimately, understanding your body’s needs and finding the right carb intake within the keto framework is essential for optimal results.
Example: If your daily calorie needs are 2000 calories and you choose a 20% carbohydrate allocation, then your daily carbohydrate allowance would be 400 calories, equivalent to approximately 100 grams of carbohydrates.
Using Standardized Formulas
Several formulas can estimate carbohydrate intake based on body weight and activity level. These formulas provide a framework, but individual responses can vary, necessitating adjustments based on individual needs.
Example: A commonly used formula might calculate daily carbohydrate needs as a percentage of body weight. For a 150-pound individual, this calculation could suggest a lower carbohydrate intake compared to a 200-pound individual.
Examples of Daily Carbohydrate Allowances
Daily carbohydrate allowances vary based on individual factors, including body weight, activity level, and metabolic needs. Below are some examples, which are not exhaustive.
| Body Weight (lbs) | Activity Level | Estimated Carbohydrate Allowance (grams) |
|---|---|---|
| 130 | Sedentary | 20-40 |
| 150 | Moderately Active | 25-50 |
| 180 | Highly Active | 30-60 |
Adjusting Carbohydrate Intake
Adjusting your carbohydrate intake is crucial for maintaining a healthy ketogenic state and achieving your specific goals. Monitoring your body’s response to different carbohydrate levels is key. Changes in energy levels, appetite, and weight can signal the need for adjustments. If you experience persistent symptoms or do not see the desired results, consulting with a healthcare professional or registered dietitian is essential.
Carbohydrate Intake Recommendations for Different Keto Phases
Different ketogenic phases may have different carbohydrate intake recommendations. A transition phase might allow for a higher carbohydrate allowance compared to a more established ketogenic lifestyle.
| Keto Phase | Carbohydrate Intake (grams) |
|---|---|
| Transition Phase | 25-50 |
| Established Ketogenic Diet | 20-40 |
| Keto Cycling/Modified Keto | Varying, dependent on the specific protocol |
Food Sources and Tracking
Fueling your keto journey effectively involves understanding not just the
- what* but also the
- how* of your food choices. This section dives into the practical aspects of selecting keto-friendly foods and precisely tracking your carbohydrate intake to maintain ketosis. It’s crucial to remember that consistency and accuracy are key to success on this diet.
The ketogenic diet relies on a significant reduction in carbohydrate intake. This shift requires careful consideration of food sources and meticulous tracking to ensure you’re meeting your nutritional needs while staying within your carbohydrate limits. By mastering these techniques, you’ll gain a greater understanding of your body’s response to the ketogenic lifestyle.
Common Low-Carbohydrate Food Sources
A wide array of foods are compatible with ketogenic diets, providing essential nutrients without significant carbohydrate contributions. These include meats, fish, poultry, and various vegetables.
- Meats: Beef, pork, lamb, and chicken are excellent keto-friendly protein sources, offering a satisfying and nutritious foundation for meals. They are generally very low in carbohydrates.
- Fish and Seafood: Salmon, tuna, shrimp, and other fish are rich in protein and healthy fats, making them excellent additions to a ketogenic diet. They’re also low in carbohydrates.
- Poultry: Chicken, turkey, and duck are popular keto choices, providing lean protein and satisfying your hunger without hindering ketosis.
- Non-Starchy Vegetables: Leafy greens, broccoli, cauliflower, spinach, and peppers are excellent keto options. They are typically low in carbohydrates and high in vitamins and minerals.
Methods for Accurate Carbohydrate Tracking
Precise carbohydrate tracking is essential for maintaining ketosis. Various tools and techniques can help you monitor your intake effectively.
- Food Logging Apps: Numerous apps offer detailed nutritional information for thousands of foods, enabling you to input your meals and calculate carbohydrate content. These apps can provide accurate and consistent carbohydrate tracking, helping you stay within your daily limit.
- Nutrition Labels: Reading food labels carefully is crucial for understanding the carbohydrate content of packaged and processed foods. Pay close attention to serving sizes and carbohydrate counts per serving to avoid unexpected spikes in carbohydrate intake.
Importance of Understanding Portion Sizes
Portion control plays a vital role in carbohydrate management. A small difference in portion size can significantly affect your overall carbohydrate intake.
Accurate portion control is key to success on any diet, including keto.
Even seemingly low-carbohydrate foods can contribute substantial carbohydrates if consumed in excessive quantities. Understanding serving sizes and sticking to them is crucial for maintaining ketosis.
Examples of High-Carbohydrate Foods to Avoid
To maintain ketosis, it’s essential to limit high-carbohydrate foods. These include sugary drinks, processed foods, and starchy vegetables.
- Sugary Drinks: Sugary sodas, juices, and sweetened beverages are major contributors to carbohydrate intake and should be avoided on ketogenic diets.
- Processed Foods: Many processed foods contain hidden sugars and starches, significantly increasing carbohydrate content. These foods should be consumed sparingly or avoided altogether.
- Starchy Vegetables: Potatoes, corn, and peas are examples of starchy vegetables with relatively high carbohydrate counts. They should be included in moderation or excluded entirely on a ketogenic diet.
Common Keto-Friendly Foods and Their Carbohydrate Content
This table provides approximate carbohydrate content per serving for common keto-friendly foods. Note that values may vary based on preparation methods and specific brands.
| Food | Approximate Carbohydrates (g/serving) |
|---|---|
| Beef | 1-3 |
| Chicken Breast | 0-1 |
| Salmon | 0-1 |
| Cauliflower | 3-5 |
| Broccoli | 4-6 |
| Spinach | 1-2 |
Considerations for Specific Populations: How Many Carbs On Keto
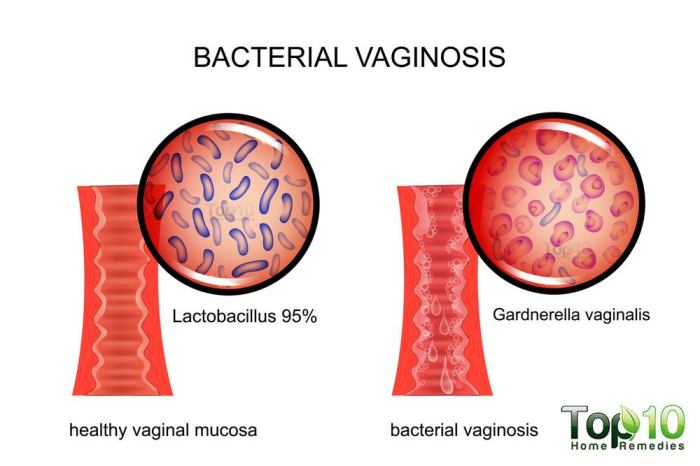
The ketogenic diet, while offering potential benefits for many, isn’t a one-size-fits-all approach. Individual needs and health conditions can significantly impact the suitability and safety of this dietary regimen. Careful consideration of specific circumstances is crucial for maximizing potential benefits and minimizing risks.Understanding how carbohydrate needs may vary for individuals with specific health conditions, along with the importance of professional guidance, potential risks, and possible interactions with medications, is essential for anyone contemplating a ketogenic lifestyle.
Variations in Carbohydrate Needs for Specific Health Conditions
Individuals with pre-existing health conditions, such as diabetes or kidney disease, require tailored dietary approaches. Carbohydrate restriction must be approached cautiously, with medical oversight. Diabetes management, for example, necessitates a careful balance between carbohydrate intake and insulin requirements. Kidney disease often necessitates a reduced protein intake, and a ketogenic diet may need to be adapted to accommodate these restrictions.
Importance of Consulting a Healthcare Professional
Before embarking on a ketogenic diet, consulting a healthcare professional is paramount. A healthcare provider can assess individual health status, identify potential risks, and tailor a safe and effective ketogenic plan. This includes a thorough evaluation of current medications, existing conditions, and potential interactions with the diet. This professional guidance is essential for safe and effective management of the diet.
Potential Risks and Side Effects of Restrictive Ketogenic Diets, How many carbs on keto
Restrictive ketogenic diets, while effective for some, can carry potential risks and side effects. These include, but are not limited to, nutritional deficiencies, constipation, headaches, and fatigue. The rapid shift in macronutrient intake can trigger initial discomfort. The keto flu, a temporary set of symptoms, is a common experience in the initial stages. Careful monitoring and adjustments are often needed to mitigate these potential issues.
Potential Interactions Between Ketogenic Diets and Medications
Certain medications can interact with a ketogenic diet. For example, some medications may affect blood sugar levels or electrolyte balance, which are particularly sensitive during the transition to a ketogenic diet. Individuals taking medications for conditions like diabetes, heart disease, or epilepsy should discuss potential interactions with their doctor before starting a ketogenic diet.
Table: Potential Challenges and Solutions for Managing Carbohydrate Intake in Specific Health Conditions
| Health Condition | Potential Challenges | Potential Solutions |
|---|---|---|
| Diabetes | Difficulty in managing blood sugar levels, potential for hypoglycemia or hyperglycemia, potential medication interactions. | Close monitoring of blood glucose levels, careful carbohydrate counting and adjustments in accordance with doctor’s instructions, and close communication with the healthcare team. |
| Kidney Disease | Managing protein intake, potential for electrolyte imbalances, risk of kidney stones. | Working closely with a registered dietitian and nephrologist, closely monitoring protein intake, and ensuring appropriate electrolyte balance. |
| Pregnancy and Lactation | Meeting nutritional needs of both the mother and the developing fetus/infant, potential for complications. | Close consultation with a healthcare professional, maintaining adequate intake of nutrients and micronutrients, and ensuring proper adaptation to meet the evolving needs. |
Practical Application and Tools
Embarking on a ketogenic journey requires more than just understanding the dietary principles. Successful implementation hinges on practical strategies for incorporating keto into daily life, effective meal planning, and the use of helpful tools. This section will delve into these practical aspects, providing you with actionable steps and resources to navigate the keto lifestyle smoothly.Understanding the practicalities of keto goes beyond simply counting macros.
It involves building sustainable habits, creating enjoyable meals, and utilizing tools to simplify the process. This approach fosters long-term adherence and allows you to enjoy the benefits of this dietary approach.
Figuring out the perfect carb count on keto can feel tricky, but it’s key to overall health. One factor often overlooked is how carb intake can indirectly influence high blood pressure causes. Understanding the interplay between these two is crucial for maintaining a balanced diet. For more on the various causes of high blood pressure, check out this informative article: high blood pressure causes.
Ultimately, finding the right keto carb count is a personalized journey, and your doctor can help you determine the best approach for your specific needs.
Incorporating Ketogenic Principles into Daily Life
Integrating keto into your routine requires mindful adjustments to your existing lifestyle. Start by gradually reducing your carbohydrate intake, paying close attention to food labels and portion sizes. Prioritize whole, unprocessed foods, such as vegetables, lean proteins, and healthy fats. Finding keto-friendly recipes and meal ideas that you genuinely enjoy is key to long-term adherence. This often involves experimenting with new flavors and cooking methods.
Regular exercise and sufficient sleep further support the body’s ability to adapt to ketosis.
Strategies for Meal Planning and Preparation
Effective meal planning is crucial for success on a ketogenic diet. Planning your meals in advance helps you stay on track, reduces impulsive food choices, and minimizes the risk of falling off the wagon. Consider using a meal prep strategy, where you cook multiple servings of keto-friendly meals on one day and store them for future consumption. This method saves time and effort, especially during busy weeks.
It allows you to focus on preparing your food ahead of time, optimizing the use of your time and resources.
Tools and Resources for Tracking Carbohydrate Intake
Numerous tools can simplify carbohydrate tracking and make managing your ketogenic diet easier. Food tracking apps, such as MyFitnessPal or Lose It!, allow you to input your meals and calculate carbohydrate content. These apps often have extensive food databases, making it easier to find and track foods. Similarly, dedicated ketogenic diet apps provide specific keto-friendly recipes and meal ideas.
Alternatively, you can use online calculators or utilize dedicated ketogenic diet websites for calculating carbohydrate intake. This variety of options allows users to select the most convenient and suitable method.
Examples of Keto-Friendly Recipes and Meal Ideas
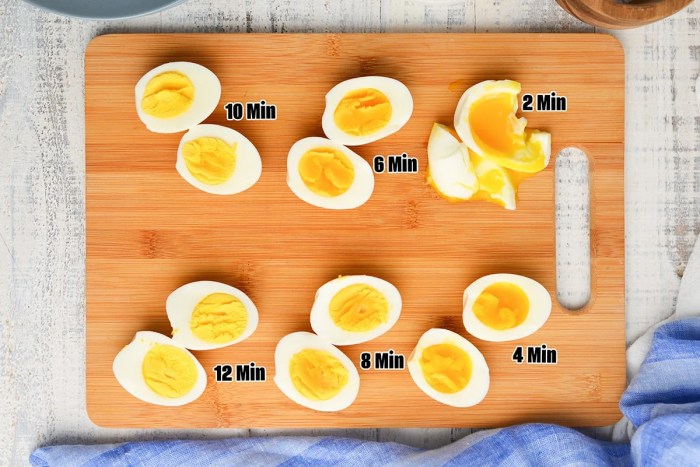
Keto-friendly meals encompass a wide range of delicious and satisfying options. Consider a breakfast of scrambled eggs with spinach and avocado. For lunch, a salad with grilled chicken or fish and a light vinaigrette is an excellent choice. A dinner could be a steak with roasted vegetables or a flavorful fish dish. These examples demonstrate the versatility of ketogenic meals.
The possibilities are endless!
Keto-Friendly Meal Prep Ideas
| Meal | Approximate Carbohydrates (per serving) |
|---|---|
| Keto Chicken Stir-Fry with Broccoli and Cauliflower Rice | 5g |
| Salmon with Roasted Asparagus and Zucchini | 3g |
| Beef and Cabbage Skillet | 4g |
| Keto Shepherd’s Pie with Cauliflower Mash | 6g |
| Shrimp Scampi with Zucchini Noodles | 2g |
Visual Representations of Carbohydrate Intake
Seeing is believing, and visualizing your ketogenic meal plan can significantly aid in your journey. A clear representation of your carbohydrate intake helps you understand your progress and makes sticking to the diet more manageable. This section dives into practical ways to visualize your carbohydrate intake, from sample meal plans to interpreting food labels.
Sample Ketogenic Meal Plan
A typical ketogenic meal plan focuses on high-fat, moderate-protein, and very-low-carbohydrate foods. Here’s a sample daily menu, highlighting the carbohydrate breakdown:
- Breakfast (approx. 5g carbs): Scrambled eggs with spinach and avocado. A handful of almonds.
- Lunch (approx. 8g carbs): Chicken salad sandwich on lettuce wraps with a side of sliced bell peppers.
- Dinner (approx. 10g carbs): Baked salmon with roasted broccoli and cauliflower mash.
- Snacks (approx. 2g carbs): A handful of mixed nuts and a small portion of cheese.
Step-by-Step Keto Meal Planning
This structured approach to meal planning can ease the transition to keto:
- Determine your daily carbohydrate allowance. This depends on your individual needs and activity level. Consult a healthcare professional or registered dietitian for personalized guidance.
- Choose keto-friendly protein sources. Examples include chicken, fish, beef, pork, eggs, and tofu.
- Select low-carbohydrate vegetables. Cruciferous vegetables, leafy greens, and non-starchy options are excellent choices.
- Prioritize healthy fats. Avocados, nuts, seeds, olive oil, and coconut oil are vital for a ketogenic diet.
- Prepare meals in advance. This can help manage cravings and ensure adherence to the diet.
Interpreting Nutritional Labels
Understanding nutritional labels is crucial for accurately assessing carbohydrate content. Look for the “Total Carbohydrate” section, and then break it down further:
- Total Carbohydrate: This is the sum of all carbohydrates in the food.
- Dietary Fiber: This type of carbohydrate is not fully absorbed and is subtracted from the total.
- Net Carbohydrate: Subtracting dietary fiber from total carbohydrate gives you the net carbohydrate content, a more accurate representation of the carbs your body will process.
Visual Examples of Low-Carbohydrate Foods
Imagine a plate with grilled chicken breast, a large portion of broccoli florets, and a side of sliced avocado. Another image could showcase a bowl of mixed greens with grilled shrimp and a light vinaigrette dressing. A third could depict a stack of cauliflower “rice” topped with a flavorful tomato sauce and a serving of lean ground beef.
Comparison of Carbohydrate Content Across Food Groups
This table provides a comparative view of carbohydrate content in different food groups relevant to ketogenic diets.
| Food Group | Example Food | Approximate Carbohydrate (per 100g) |
|---|---|---|
| Vegetables | Broccoli | 5-10g |
| Fruits | Berries | 8-15g |
| Grains | White Bread | 40-50g |
| Legumes | Beans | 10-20g |
| Dairy | Greek Yogurt | 5-10g |
Last Point
In conclusion, determining the right carbohydrate intake on keto is a personalized journey that requires careful consideration of your individual needs and goals. By understanding the different ketogenic approaches, calculating your daily carbohydrate allowance, and choosing the right foods, you can effectively manage your carb intake and experience the benefits of this dietary strategy. Remember to consult with a healthcare professional before starting any new diet, especially if you have underlying health conditions.