What shots do you get at 16? This question explores the various vaccinations and health services available to 16-year-olds, taking into account legal, societal, and personal factors. Understanding these options is crucial for making informed decisions about your health and well-being during this important stage of life.
This guide delves into the legal frameworks, specific health services, age-related concerns, and available resources. We’ll also examine the importance of preventative care and the steps involved in accessing healthcare services at this crucial time.
Legal and Societal Considerations
Navigating the world of healthcare at 16 involves a complex interplay of legal frameworks, societal expectations, and personal autonomy. Different countries have varying approaches to health decisions made by adolescents, often reflecting cultural values and historical precedents. Understanding these nuances is crucial for both adolescents and their families to ensure access to appropriate care and support.The legal and societal landscapes surrounding healthcare choices for 16-year-olds are significantly shaped by a variety of factors.
These factors include the specific legal frameworks in place, the cultural norms and expectations surrounding health decisions, and the degree of autonomy granted to adolescents. The interplay of these elements can result in diverse healthcare options and experiences for young adults across the globe.
Legal Frameworks Surrounding Vaccinations and Health Services
Different countries have varying legal requirements regarding vaccinations and the provision of health services for 16-year-olds. Some countries may mandate specific vaccinations, while others might allow for parental consent or the individual’s consent, depending on the type of service. These differences reflect the diverse approaches to public health and individual autonomy.
So, what shots do you get at 16? Mostly routine vaccinations, but sometimes there are other health-related injections. It’s important to remember that factors like genetics can play a significant role in conditions like male or female pattern baldness, male or female pattern baldness , and these things can affect how a doctor approaches a patient’s health.
Still, the core shots remain pretty standard for that age group.
Societal Norms and Expectations
Societal norms and expectations significantly influence health decisions for 16-year-olds. Cultural values regarding the role of parents in healthcare decisions, the level of independence granted to adolescents, and the importance of individual autonomy can differ greatly. These norms are often deeply ingrained and influence the attitudes towards healthcare choices. For instance, in some cultures, a strong emphasis on parental authority in healthcare decisions might prevail.
In others, there might be greater emphasis on respecting the individual’s autonomy, even if they are still considered minors.
Autonomy Levels Granted to 16-Year-olds
The level of autonomy granted to 16-year-olds regarding healthcare choices varies considerably across jurisdictions. In some countries, 16-year-olds may have the right to make their own decisions about certain health issues, while in others, parental consent is still required for a wider range of services. This difference in autonomy reflects varying perspectives on adolescent maturity and the balance between parental rights and individual rights.
For example, some countries might allow 16-year-olds to consent to contraception or mental health services without parental involvement, whereas other countries might require parental consent for even routine check-ups.
Ethical Implications of Restrictions on Healthcare Access
Restrictions or limitations on healthcare access for 16-year-olds raise several ethical concerns. Denying adolescents appropriate care, particularly for issues like reproductive health or mental health, can have significant negative consequences. This is particularly relevant in situations where adolescents might face risks of harm if they cannot access the services they need. The potential long-term impact on their health and well-being needs to be considered.
Influence of Parental Consent Laws
Parental consent laws play a crucial role in shaping healthcare options for 16-year-olds. These laws can dictate whether a minor needs parental consent for specific procedures or services. The specific regulations can vary significantly across countries and even within different regions of a country. Understanding these variations is essential to ensure that adolescents receive the appropriate care, particularly when facing complex medical situations.
Examples include situations where a minor seeks contraceptive services or needs to undergo a specific treatment for a condition. This is where parental consent laws often come into play, defining the boundaries of decision-making authority for both the adolescent and their parents.
Specific Health Services

Navigating the complexities of health services at 16 can feel overwhelming. This section provides a structured overview of essential vaccinations, screenings, and preventative health considerations tailored to this crucial developmental stage. Understanding these services empowers young adults to make informed decisions about their well-being.
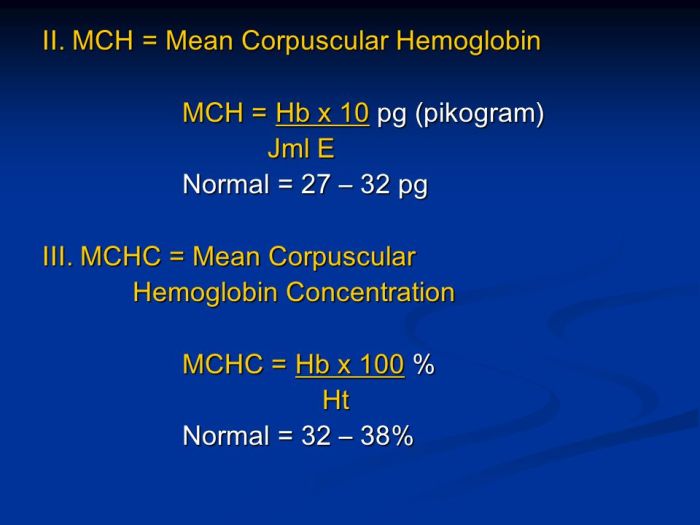
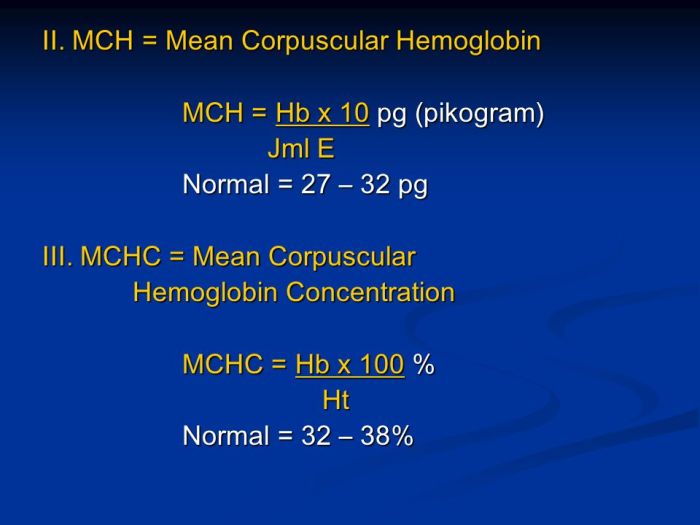
Vaccinations
Vaccinations play a critical role in maintaining a healthy immune system. The following table Artikels common vaccinations recommended or required for 16-year-olds, including booster doses. These immunizations help protect against serious diseases and are crucial for overall health.
| Vaccination | Schedule | Reason |
|---|---|---|
| Tdap (tetanus, diphtheria, pertussis) | Booster dose recommended, typically around 16 years old | Pertussis, or whooping cough, can be severe, especially in adolescents. A booster dose ensures ongoing protection. |
| Meningococcal | Booster dose recommended, especially for individuals at higher risk | Meningococcal disease can be life-threatening. Booster doses can help maintain immunity. |
| HPV (Human Papillomavirus) | Series of doses, often initiated in the pre-teen years | HPV vaccination can significantly reduce the risk of certain cancers later in life. |
| Flu (Influenza) | Annual vaccination recommended | Influenza is a highly contagious respiratory illness. Annual vaccination is essential for protection. |
Health Screenings
Regular health screenings are essential for early detection and prevention of potential health issues. The following table highlights common screenings appropriate for 16-year-olds. These screenings contribute to proactive health management.
| Screening | Frequency | Importance |
|---|---|---|
| Blood pressure | Annually or as recommended by a doctor | High blood pressure can develop in adolescence and is a risk factor for various health problems later in life. Early detection allows for timely intervention. |
| Cholesterol | Annually or as recommended by a doctor | High cholesterol can contribute to heart disease. Regular screenings help identify potential risks early on. |
| Vision and hearing | Annually or as needed | Changes in vision and hearing can occur during adolescence. Regular screenings ensure timely intervention and address any potential issues. |
Preventative Health Services
Preventative health services are crucial for overall well-being, including mental health. Addressing potential issues proactively can significantly improve quality of life. Early intervention for mental health issues is especially important in adolescence.Mental health services are vital at this stage. Many young adults experience anxiety, depression, or other mental health challenges. Access to counseling, therapy, or support groups can make a significant difference in navigating these issues.
School-based counseling programs and community mental health centers are often resources.
Reproductive Health Services
Reproductive health services, including contraception and STI testing, are important for young adults. Access to these services empowers them to make informed decisions about their sexual health. Contraception options include various methods like birth control pills, condoms, and long-acting reversible contraceptives.
Geographic Availability of Health Services
The availability and types of health services accessible to 16-year-olds can vary significantly based on geographic location. This difference often stems from factors like socioeconomic status, healthcare infrastructure, and access to transportation.
| Region | Available Services | Accessibility |
|---|---|---|
| Rural areas | Limited access to specialized services like mental health specialists or certain types of contraception. May require travel to urban areas. | Access can be challenging due to distance and transportation limitations. |
| Urban areas | Greater availability of specialized services, including mental health professionals and a wider range of reproductive health options. | Generally easier access to services, but potential for long wait times or higher costs. |
| Low-income communities | Limited access to preventative health services due to financial constraints or lack of insurance. | Financial barriers and lack of awareness can hinder access. |
Health Concerns Specific to Age 16
Navigating the complex landscape of adolescence often brings unique health challenges. Sixteen-year-olds are at a critical juncture, experiencing significant physical and emotional changes. Understanding the common health concerns at this age is crucial for parents, educators, and healthcare providers to ensure the well-being of this vulnerable population. Early detection and appropriate intervention can significantly impact long-term health outcomes.The transition to adulthood is marked by a myriad of physiological and psychological shifts.
Hormonal fluctuations, the burgeoning independence from parental guidance, and the pressures of peer relationships all contribute to a heightened vulnerability to specific health issues. This period demands proactive approaches to health maintenance, emphasizing both preventative care and prompt response to potential problems.
Common Physical Health Concerns
Physical development continues at a rapid pace during adolescence. Growth spurts, hormonal imbalances, and changes in body composition can lead to various physical health concerns. These include issues such as acne, menstrual irregularities in girls, and musculoskeletal problems like back pain and joint pain. Nutritional deficiencies can also arise, as teenagers often have erratic eating habits and prioritize social activities over healthy eating.
- Acne: Hormonal changes are a significant contributor to acne breakouts. The increased production of sebum, combined with the influence of hormones, clogs pores and leads to inflammation. Early intervention and proper skin care routines can help manage acne effectively.
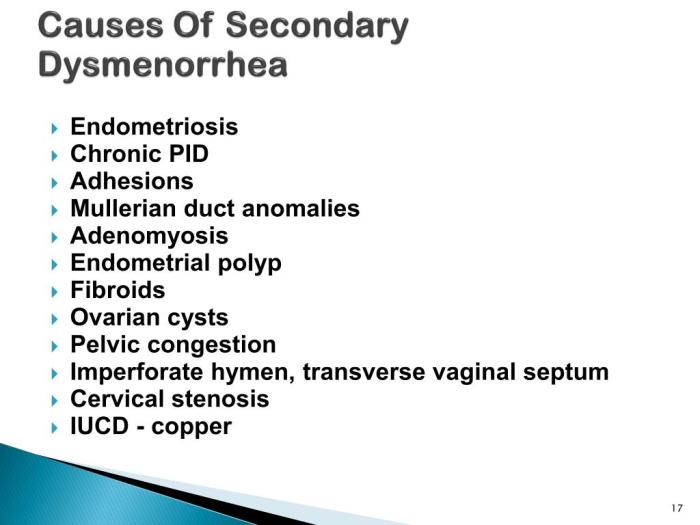
- Menstrual Irregularities (Girls): The onset of menstruation can be accompanied by various irregularities, including painful periods (dysmenorrhea), heavy bleeding, and irregular cycles. Understanding these changes and seeking appropriate medical advice is crucial for managing these issues.
- Musculoskeletal Issues: Rapid growth spurts can strain the musculoskeletal system, leading to back pain, joint pain, and even injuries. Maintaining good posture, engaging in regular physical activity, and seeking professional advice for any persistent pain are essential.
- Nutritional Deficiencies: Poor dietary choices, busy schedules, and social pressures can contribute to nutritional deficiencies. Inadequate intake of essential vitamins and minerals can lead to fatigue, weakened immunity, and other health problems. Encouraging a balanced diet and regular mealtimes is crucial.
Common Mental Health Concerns
The emotional landscape of adolescence is characterized by significant changes in mood, self-perception, and social interactions. This period can be marked by heightened vulnerability to mental health challenges. The prevalence of anxiety, depression, and substance use disorders is a growing concern.
Wondering what shots you get at 16? While some vaccinations are routine, others might depend on individual needs. For example, if you’re experiencing neck pain, it’s important to consider if it could be connected to your jaw joint, like is your neck pain related to your jaw joint. Ultimately, your doctor can best advise you on any necessary shots based on your health history and current situation.
- Anxiety Disorders: Anxiety disorders, such as generalized anxiety disorder and panic disorder, are relatively common among adolescents. These disorders are often characterized by excessive worry, fear, and physical symptoms. Early recognition and treatment are essential to prevent the progression and impact of anxiety on daily life.
- Depression: Depression is another significant mental health concern among teenagers. Symptoms include persistent sadness, loss of interest in activities, changes in appetite and sleep patterns, and feelings of hopelessness. Early intervention and professional support are crucial in managing and alleviating the effects of depression.
- Substance Use Disorders: The experimentation with and use of substances, including alcohol and drugs, can have devastating effects on adolescent health and well-being. These can lead to physical and psychological dependence and a wide range of other issues, including risky behaviors and academic difficulties. Education and early intervention are vital in mitigating these risks.
Importance of Early Intervention and Preventative Care
Early intervention for both physical and mental health concerns is paramount. Addressing these issues promptly can prevent the development of long-term health problems and significantly improve quality of life. Proactive strategies are crucial in fostering healthy habits and promoting well-being during this transformative period.
- Regular Check-ups: Regular check-ups with healthcare providers are essential for monitoring physical and mental health. These visits allow for early detection of potential issues and facilitate the implementation of preventative measures.
- Open Communication: Open communication between teenagers, parents, and healthcare providers is vital for addressing concerns and fostering a supportive environment. Creating a safe space for discussion can help teenagers feel comfortable seeking help when needed.
Educational Resources and Information
Navigating the world of health information at 16 can feel overwhelming. There’s a wealth of resources available, but knowing where to start and how to evaluate them critically is key. This section provides a roadmap for finding reliable information and making informed decisions about your health.Reliable sources are crucial when seeking health information. This section offers a selection of reputable websites, highlighting key aspects of health and well-being for teenagers, and practical steps for evaluating information to ensure its accuracy and relevance.
Reputable Online Resources for Health Information
Finding credible health information online is essential for 16-year-olds. Reliable websites provide accurate, evidence-based information, helping you make informed decisions.
| Website | Topic | Audience |
|---|---|---|
| Mayo Clinic | Comprehensive health information, including diseases, treatments, and wellness | General public, including teens |
| National Institutes of Health (NIH) | Extensive research, studies, and publications on various health conditions | Researchers, healthcare professionals, and the public |
| American Academy of Pediatrics (AAP) | Child and adolescent health topics, including developmental stages, vaccinations, and mental health | Parents, healthcare providers, and teens |
| Cleveland Clinic | Information on a wide range of medical conditions, treatments, and procedures | General public, including teens |
| WebMD | Symptom checkers, health conditions, and treatment options | General public, including teens (but requires critical evaluation) |
Key Points About Health and Well-being for 16-Year-olds
Understanding key health and well-being aspects is crucial for navigating this stage of life. This section provides essential information to support teenagers in their development.
- Physical Health: Maintaining a balanced diet, getting sufficient sleep, and regular exercise are essential for overall physical health. Regular check-ups with a doctor are vital for early detection of any potential issues.
- Mental Health: Recognizing and addressing mental health concerns is paramount. Feeling overwhelmed, anxious, or depressed are common experiences, and seeking help from a trusted adult or professional is a positive step.
- Healthy Relationships: Building and maintaining healthy relationships, both with friends and family, contributes significantly to emotional well-being. Understanding healthy communication and boundaries is important.
- Decision-Making Skills: Developing strong decision-making skills is essential for navigating various situations and making informed choices, including those related to health.
Accessing and Evaluating Reliable Health Information
Evaluating the reliability of health information is critical. This involves checking the source’s reputation, author’s credentials, and the overall quality of the information.
- Source Reputation: Look for reputable organizations or institutions, like those mentioned in the table. These are usually backed by evidence-based research and expert opinions.
- Author Credentials: Ensure the author is qualified to provide the information. Doctors, researchers, and other qualified professionals are usually the best sources.
- Evidence-Based Information: Look for information backed by scientific research and clinical studies. This demonstrates the validity of the claims.
- Bias Detection: Be mindful of potential biases. Information from commercial sites might have an underlying agenda.
Resources for Informed Decisions
Accessing various resources can assist 16-year-olds in making informed decisions about their health.
Wondering what shots you get at 16? Well, it’s a bit more complex than just a simple answer. While some vaccinations are routine, a deeper understanding of preventative health often involves exploring holistic approaches like traditional Chinese medicine, which focuses on balancing the body’s energy flow. Learning about traditional Chinese medicine overview might give you a broader perspective on overall health and how preventative measures can be tailored to individual needs.
Ultimately, talking to your doctor is still the best way to find out what shots you should be getting at 16.
- Family Doctors: Discussing health concerns and options with your family doctor is crucial. They can provide personalized guidance and connect you with relevant specialists.
- School Counselors: School counselors can offer support and resources for navigating academic, social, and emotional challenges. They can connect you with local services.
- Community Health Centers: Community health centers offer affordable and accessible healthcare services, including preventative care, mental health support, and more.
Navigating the Health System, What shots do you get at 16
Understanding how the health system works is vital for 16-year-olds. It helps them find the right resources and support.
- Insurance Coverage: Understand your insurance coverage to know what services are covered and the procedures for claiming them.
- Healthcare Providers: Research and choose healthcare providers who align with your needs and preferences.
- Appointment Scheduling: Learn how to schedule appointments effectively and follow up as needed.
Illustrative Examples and Case Studies: What Shots Do You Get At 16
Navigating the healthcare system at 16 can be a complex process, involving personal responsibility, parental involvement, and often, the intricate details of healthcare policies and procedures. This section explores real-world scenarios to shed light on the practical aspects of accessing healthcare services during adolescence.Understanding the challenges and triumphs faced by 16-year-olds seeking healthcare is crucial for both healthcare providers and families.
This section will provide hypothetical examples and case studies to illustrate the process, highlighting potential obstacles and successful outcomes.
Hypothetical Scenario: A 16-Year-Old Seeking Mental Health Services
A 16-year-old, Sarah, experiences increasing anxiety and depression. She feels unable to confide in her parents and seeks help independently. She knows that her local health department offers mental health services, and she decides to investigate how to access them. This scenario underscores the importance of readily available information about services for adolescents, including clear guidelines on privacy and confidentiality.
Steps Involved in Accessing Healthcare Services at Age 16 (Example: A Local Community Health Center)
Accessing healthcare at 16 involves several steps, varying depending on the specific healthcare facility and location. For example, at a community health center, the process might include:
- Initial Contact: Sarah calls the health center to inquire about mental health services and scheduling.
- Intake Assessment: A counselor conducts an initial assessment to understand Sarah’s needs and concerns.
- Referral/Appointment Scheduling: If necessary, a referral to a therapist or psychiatrist may be provided, and an appointment schedule will be made.
- Treatment Plan Development: The therapist collaborates with Sarah to create a tailored treatment plan that addresses her specific needs.
- Follow-up Appointments: Regular appointments and ongoing support are crucial for monitoring progress and adjusting the treatment plan as needed.
Case Study: Successful Health Outcome
A 16-year-old, David, experienced persistent headaches and nausea. After several doctor visits and diagnostic tests, a diagnosis of migraine was confirmed. Through proper medication and lifestyle adjustments, David successfully managed his migraines, reducing their frequency and intensity. This highlights the importance of persistence in seeking medical care, and the positive impact of a clear diagnosis and treatment plan.
Considerations When Discussing Healthcare Options
When discussing healthcare options with a 16-year-old, open communication is key. Important considerations include:
- Emphasize Confidentiality: Explain the importance of privacy in medical consultations and encourage open communication.
- Active Listening: Encourage the adolescent to express their concerns and questions.
- Providing Choices: Present various healthcare options, ensuring the adolescent understands the potential benefits and drawbacks of each.
- Respecting Autonomy: While parental involvement is important, acknowledge the adolescent’s growing independence and decision-making capabilities.
Potential Challenges Faced by 16-Year-Olds
Several challenges can hinder a 16-year-old’s access to healthcare.
- Lack of Awareness: Limited knowledge about available services or procedures can impede seeking necessary care.
- Transportation Issues: Geographic limitations or lack of transportation can make accessing healthcare facilities difficult.
- Financial Constraints: Cost of services, co-pays, and insurance coverage can create significant barriers.
- Social Stigma: Fear of judgment or embarrassment about mental health or other conditions can discourage adolescents from seeking help.
- Parental Barriers: Conflicting opinions or lack of support from parents can complicate the process.
Final Wrap-Up

Navigating the world of healthcare at 16 can be complex. This guide has provided a comprehensive overview of the available shots, screenings, and services. By understanding the legal landscape, specific health needs, and available resources, 16-year-olds can take an active role in their health management. Remember, open communication with healthcare providers and trusted adults is key to making informed decisions.