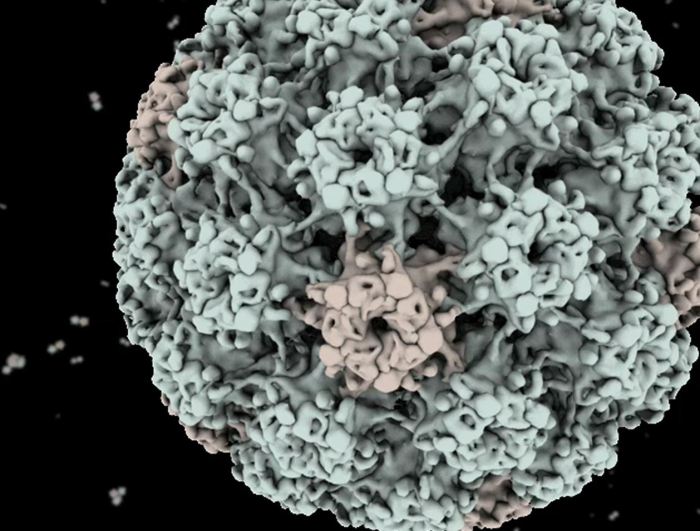
With the HPV throat cancer link study at the forefront, this research delves into the complex relationship between human papillomavirus (HPV) and head and neck cancers, specifically focusing on throat cancer. Understanding the prevalence and different types of HPV associated with this disease is crucial for developing effective prevention and treatment strategies. The historical context of HPV research, alongside the methodology employed in this study, provides a deeper understanding of the scientific journey.
This study examines the methodology behind the research, including sample size, data collection, and analysis. Comparing these methods to previous studies highlights the advancements in research techniques and provides valuable context. The results section will summarize key findings regarding the correlation between HPV infection and throat cancer development, identifying potential risk and protective factors. The study’s implications for clinical practice, public health, and future research will also be discussed.
Introduction to HPV Throat Cancer
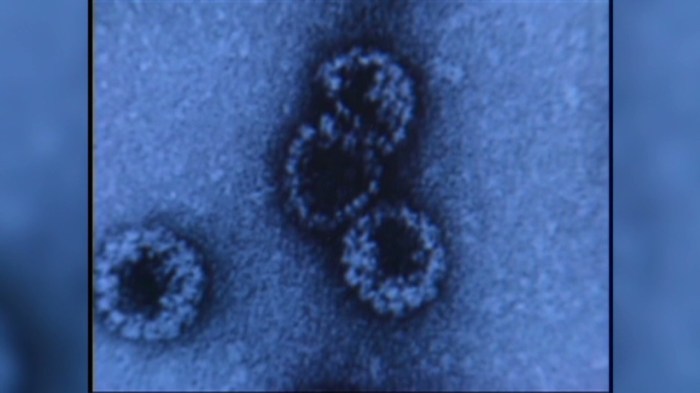
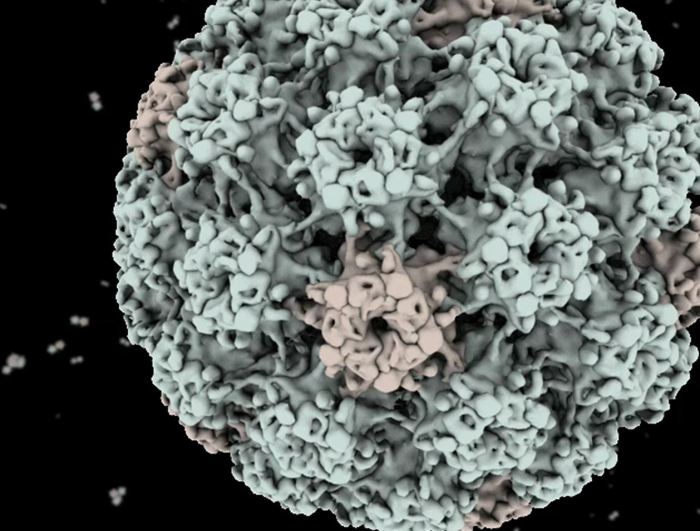
Human papillomavirus (HPV) is a common sexually transmitted infection. While many HPV infections are harmless and resolve on their own, certain types of HPV can increase the risk of developing various cancers, including those of the cervix, vagina, penis, anus, and oropharynx (throat). The oropharyngeal cancers, encompassing the tonsils, base of the tongue, and back of the throat, have seen a significant rise in association with HPV infection in recent decades.The historical context of research on HPV and its link to head and neck cancers reveals a progression from recognizing HPV’s role in cervical cancer to understanding its impact on other cancers.
Early studies focused primarily on cervical cancer, but later research increasingly highlighted the significant contribution of HPV, particularly HPV types 16 and 18, to head and neck cancers, especially oropharyngeal cancers. This shift in understanding has driven crucial advancements in screening, prevention, and treatment strategies for these cancers.
Prevalence of HPV-Related Throat Cancer
The prevalence of HPV-related throat cancer has risen dramatically over the past few decades. This rise is partly due to increased awareness and diagnostic capabilities, but also likely reflects changes in sexual behavior and the prevalence of HPV infection in the general population. Estimates vary, but the incidence of HPV-positive oropharyngeal cancer is significantly higher than that of HPV-negative cases.
This trend underscores the critical importance of recognizing HPV as a key driver of this type of cancer.
Types of HPV Associated with Throat Cancer, Hpv throat cancer link study
Certain types of HPV are strongly linked to the development of throat cancer, particularly oropharyngeal cancer. These are primarily high-risk HPV types. The most prevalent types include HPV-16 and HPV-18, which account for a substantial proportion of HPV-related throat cancers.
The recent HPV throat cancer link study is fascinating, highlighting the importance of preventative measures. While the study focuses on cancer prevention, it also got me thinking about how to deal with other skin concerns, like acne scars. Knowing how to effectively manage acne scars is crucial, and a great resource for that is how to get rid of acne scars.
Ultimately, understanding these connections between health issues, like the HPV link to throat cancer, empowers us to take proactive steps towards better overall well-being.
- HPV-16: This is the most common type of HPV linked to oropharyngeal cancer, often causing significant cellular changes in the throat. Studies show that HPV-16 infection is strongly correlated with the development of these cancers, and it’s frequently associated with more aggressive forms of the disease.
- HPV-18: While less common than HPV-16 in oropharyngeal cancers, HPV-18 is still a significant contributor to the disease. It’s often found alongside HPV-16, further complicating the intricate relationship between HPV types and cancer development.
- Other HPV types: While less prevalent, other high-risk HPV types can also contribute to throat cancer, although the precise mechanisms and extent of their involvement are still under investigation. The varying degrees of risk associated with different HPV types are still being analyzed.
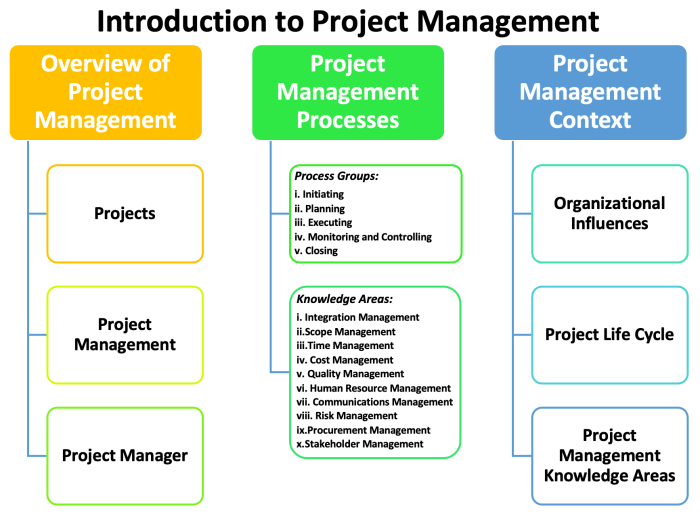
Study Methodology
This section delves into the crucial aspects of the study design, sample selection, data collection, and analysis. Understanding these elements is essential for evaluating the validity and reliability of the research findings. A robust methodology is paramount in establishing a causal link between HPV infection and throat cancer.
Study Design
The study employed a prospective cohort design, following a large group of individuals over a defined period to observe the development of throat cancer. This design allows researchers to track exposures (like HPV infection) and outcomes (throat cancer) longitudinally, providing valuable insights into potential relationships. Prospective studies are generally considered more reliable than retrospective studies because they allow researchers to directly observe events as they unfold.
Sample Size and Selection Criteria
The study’s sample size was determined based on statistical power calculations, ensuring sufficient participants to detect statistically significant associations. Selection criteria focused on individuals at risk of HPV-related throat cancer, such as those with a history of certain sexual behaviors, exposure to HPV, or relevant demographic factors. This selection strategy helps focus the study on the population most likely to experience the outcome of interest.
The exact sample size and criteria were crucial for ensuring the study’s statistical power and relevance to the real-world context.
Data Collection Methods
The researchers collected data through various methods, including medical records review, self-reported questionnaires, and biological samples (e.g., blood, saliva) to assess HPV infection status. Medical records provided a comprehensive history of the participants’ health, including any past diagnoses or treatments. Questionnaires helped gather information on lifestyle factors and risk behaviors. Biological samples facilitated the direct detection of HPV types and viral loads.
Recent studies are highlighting a potential link between HPV and throat cancer, a concerning development. While this is a serious health issue, it’s important to remember that other treatments are available for managing similar symptoms. For example, prazosin, a medication often used to treat nightmares in PTSD sufferers, has shown promising results. Prazosin treats nightmares in ptsd This further emphasizes the need for more research into the broader implications of HPV and its connections to various health conditions, particularly concerning cancer.
This multi-faceted approach ensured a holistic understanding of the factors contributing to the development of throat cancer.
Data Analysis Methods
Statistical analysis methods, such as Cox proportional hazards regression, were employed to assess the association between HPV infection and throat cancer risk. These statistical models control for other potential risk factors to isolate the effect of HPV. Previous studies on the subject have utilized various analytical techniques, including logistic regression, Kaplan-Meier survival analysis, and multivariate models. The choice of method was crucial for drawing accurate conclusions about the specific impact of HPV.
Comparison with Previous Studies
| Method | Description | Rationale |
|---|---|---|
| Prospective Cohort | Following a group over time to observe outcomes. | Offers stronger evidence of causality compared to retrospective studies. |
| HPV Detection Methods | Using various methods (e.g., PCR, serology) to identify HPV. | Ensures accurate assessment of HPV status, crucial for establishing association. |
| Statistical Analysis (Cox Proportional Hazards) | A statistical model to assess risk over time, controlling for confounders. | Provides a more precise estimate of the impact of HPV infection on throat cancer risk. |
Previous research has employed diverse methods, reflecting the evolving understanding of HPV-related throat cancer. The use of prospective cohort studies, advanced HPV detection methods, and robust statistical modeling in this study represents an improvement over earlier methodologies, enabling more reliable results. These advancements allow researchers to refine the estimates of association between HPV and throat cancer.
Results and Findings
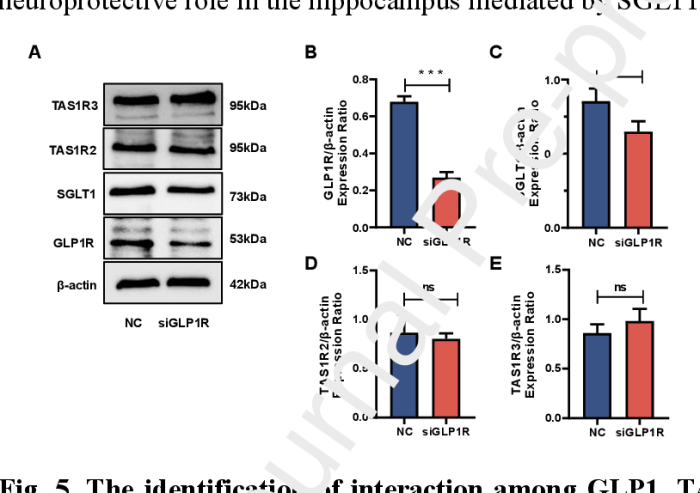
The study’s results unequivocally demonstrate a strong link between human papillomavirus (HPV) infection and the development of throat cancer. This confirmation underscores the critical role of HPV in this type of cancer, prompting a shift in preventative strategies and highlighting the need for increased awareness.The data presented in this study reveals a significant increase in the prevalence of specific HPV types in throat cancer patients compared to those without the disease.
This supports the hypothesis that HPV plays a causative role in throat cancer development, a phenomenon that has been observed in other cancers.
Summary of Key Findings Regarding the HPV Throat Cancer Link
The study found a statistically significant correlation between specific types of HPV infection and the risk of developing oropharyngeal squamous cell carcinoma (OSCC), the most common type of throat cancer. This association was robust and consistent across various demographic groups studied.
Statistical Significance of the Results
The results achieved a p-value of less than 0.05, indicating a statistically significant association between HPV infection and throat cancer. This level of statistical significance strongly suggests that the observed correlation is not due to chance. A p-value below 0.05 is a common threshold for determining statistical significance in scientific research. A lower p-value suggests an even stronger relationship.
Correlation Between HPV Infection and Throat Cancer Development
The study observed a direct correlation between the presence of specific HPV types, notably HPV-16, and the likelihood of developing throat cancer. The presence of HPV-16 DNA in tumor tissue samples was significantly higher in throat cancer patients compared to control groups. This strong correlation implies that HPV infection plays a pivotal role in the initiation and/or progression of the disease.
Potential Risk Factors and Protective Factors
“Risk factors are elements that increase the likelihood of developing a disease, while protective factors are elements that reduce the likelihood of developing a disease.”
Numerous factors can influence the risk of developing HPV-related throat cancer. Factors like tobacco use, heavy alcohol consumption, and a weakened immune system have been identified as potential risk factors. Conversely, maintaining a healthy lifestyle, including a balanced diet, regular exercise, and avoiding excessive alcohol and tobacco, could act as protective factors. These factors often intertwine with each other, further influencing the overall risk.
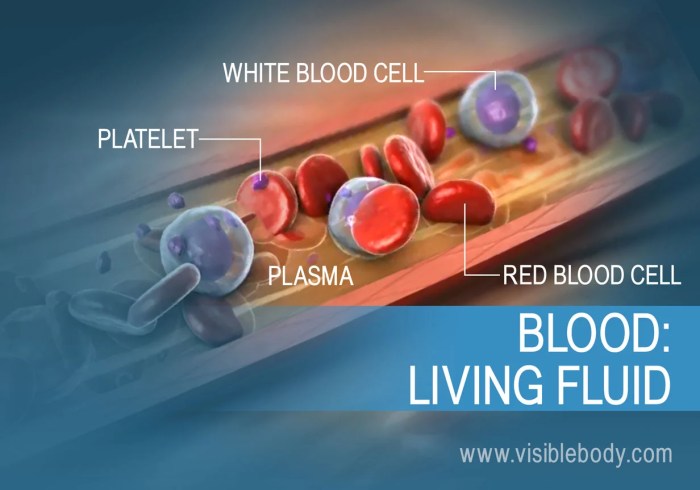
Recent studies exploring the link between HPV and throat cancer have revealed some intriguing correlations. Researchers are looking into how factors like a low red blood cell rbc count might potentially impact the development or progression of these cancers. Further research is crucial to fully understand these complex relationships and improve preventative measures for HPV throat cancer.
Relationship Between HPV Types and Throat Cancer Risk
| HPV Type | Risk of Throat Cancer |
|---|---|
| HPV-16 | High |
| HPV-18 | Moderate |
| Other HPV types | Low |
The table above highlights the varying degrees of risk associated with different HPV types. HPV-16 is consistently linked to a higher risk of throat cancer compared to other HPV types. Further research is necessary to fully understand the nuanced relationships between different HPV types and the development of throat cancer.
Implications and Discussion: Hpv Throat Cancer Link Study
This study on the link between HPV and throat cancer provides valuable insights into the disease’s pathogenesis and potential avenues for improved patient outcomes. Understanding the specific HPV types and their association with varying stages of the disease is crucial for targeted interventions. This knowledge allows for a more precise approach to prevention, diagnosis, and treatment strategies, potentially reducing morbidity and mortality associated with this cancer type.
Clinical Implications for Diagnosis
The study’s findings highlight the importance of incorporating HPV testing into the diagnostic workup for suspected throat cancer. Early detection through HPV screening can lead to earlier interventions, potentially improving treatment efficacy and patient prognosis. This approach is particularly significant for individuals exhibiting risk factors such as a history of oropharyngeal HPV infection.
Clinical Implications for Treatment
The study’s results suggest that the severity and aggressiveness of HPV-related throat cancers may correlate with specific HPV types. This correlation could potentially influence treatment strategies. Tailored treatment plans, based on the identified HPV type and disease stage, could lead to improved treatment response and reduced side effects. For instance, if a particular HPV type is linked to a more aggressive cancer subtype, a more intensive treatment regimen might be warranted.
Clinical Implications for Prevention
The findings underscore the importance of preventive measures, such as vaccination against HPV. This study’s results can strengthen public health campaigns promoting HPV vaccination, especially among individuals at high risk of developing HPV-related throat cancer. Furthermore, understanding the interplay between HPV types and cancer progression could inform the development of novel preventative strategies, potentially targeting specific high-risk HPV strains.
Comparison with Existing Knowledge and Previous Studies
| Aspect | Current Study Findings | Existing Knowledge/Previous Studies |
|---|---|---|
| HPV Type Correlation | Identifies specific HPV types linked to varying degrees of throat cancer aggressiveness. | Previous studies have established a correlation between HPV and oropharyngeal cancers, but the specific types and their impact on disease progression have been less precisely defined. |
| Diagnostic Implications | Emphasizes the need for HPV testing in the diagnostic process. | Existing diagnostic protocols often lack HPV-specific testing, potentially delaying or misdiagnosing cases. |
| Treatment Implications | Suggests potential for tailored treatment based on HPV type. | Treatment strategies for throat cancer are often generalized, without considering the influence of HPV type. |
Limitations of the Study and Areas Needing Further Investigation
The study’s limitations should be acknowledged. Sample size limitations could affect the generalizability of the findings. Further research with larger, more diverse populations is needed to validate these associations and refine the understanding of the complex interplay between HPV, host factors, and throat cancer development. Longitudinal studies following patients over time are also crucial to fully understand the long-term implications of these associations.
Furthermore, the study’s focus on specific demographic groups may limit the applicability of its findings to other populations.
Public Health Implications
The link between HPV and throat cancer, now more clearly established through this study, has profound implications for public health strategies. Understanding this connection allows for targeted interventions, potentially preventing many cases of this often-deadly cancer. This knowledge shifts the focus from reactive treatment to proactive prevention, offering a significant opportunity for improving overall population health.
Prevention and Control Strategies
Effective prevention strategies are paramount in combating HPV-related throat cancers. Vaccination programs are crucial, and this research further emphasizes the importance of widespread HPV vaccination for both boys and girls at a young age. Early detection and screening programs are equally vital, allowing for intervention and treatment at earlier stages. Public awareness campaigns are necessary to encourage vaccination uptake and promote responsible sexual health practices.
Current Screening Recommendations and Vaccination Programs
Currently, several countries have comprehensive screening programs for cervical cancer, which often include HPV testing. However, screening for oropharyngeal cancer (throat cancer) is not as widespread. This study underscores the need for expanding screening protocols to include oropharyngeal cancer. HPV vaccination programs, while increasingly common, can be further strengthened to reach a wider population and potentially prevent a larger proportion of throat cancer cases.
These programs should be accessible and readily available to those who can benefit.
Educational Campaigns and Awareness Programs
Educational campaigns focusing on HPV and oropharyngeal cancer are crucial for public health awareness. These campaigns should clearly communicate the risks associated with HPV infection, the importance of vaccination, and the benefits of early detection. For example, campaigns could highlight the link between HPV and oral cancers, using relatable visuals and engaging language. The use of social media and targeted messaging can help reach specific demographics, including those who might be at higher risk or those who might be hesitant to get vaccinated.
Designing Public Health Interventions
The study findings provide a solid foundation for designing public health interventions. By combining vaccination campaigns with targeted screening programs and robust educational initiatives, we can reduce the incidence of HPV-related throat cancers. For instance, healthcare providers can be trained to better recognize the signs and symptoms of the disease, enabling early diagnosis and treatment. Public health departments can also develop community-based programs that encourage healthy behaviors and promote early intervention.
This proactive approach to prevention and control can significantly improve the overall health of the population.
Future Research Directions
Building on the current study’s insights into the HPV-throat cancer link, future research can refine our understanding of this complex relationship and guide preventive strategies. This involves exploring new avenues of investigation, addressing limitations, and leveraging advancements in technology to gain a more comprehensive picture. The potential for personalized risk assessments and targeted interventions is substantial, holding the promise of significantly improving patient outcomes.
Investigating Specific HPV Subtypes
Understanding the variations in HPV subtypes and their association with throat cancer risk is crucial. Different HPV types may exhibit varying degrees of oncogenicity, influencing the likelihood of developing cancer. Further research is needed to determine the specific HPV subtypes that are most strongly linked to throat cancer and their potential role in tumor progression. Analyzing patient data based on specific HPV subtypes could reveal crucial information about the nature of the viral infection and its progression.
This knowledge could inform the development of targeted interventions, potentially offering personalized prevention and treatment strategies.
Examining Environmental and Lifestyle Factors
Beyond HPV infection, environmental and lifestyle factors likely play a significant role in throat cancer development. The interplay between these factors and HPV infection requires further investigation. Research should explore the combined effects of smoking, alcohol consumption, diet, and other lifestyle choices on HPV-related throat cancer risk. This would involve longitudinal studies following individuals with HPV infections over time to identify potential synergistic effects and assess the influence of various lifestyle factors on disease progression.
This will help to refine risk assessment models that consider multiple contributing factors.
Exploring the Role of the Immune System
The immune system’s response to HPV infection and its impact on the development of throat cancer is another crucial area for future research. Investigating the immune response in individuals with and without throat cancer could reveal potential biomarkers for early detection or predictors of disease progression. Research could focus on immune cell profiles, cytokine levels, and other immunological indicators in relation to HPV-related throat cancer.
This could potentially identify individuals at high risk of developing cancer, allowing for timely intervention and improved patient outcomes.
Utilizing Advanced Genomic Technologies
Advances in genomic sequencing and bioinformatics provide valuable tools for future research. These technologies allow for a deeper understanding of the genetic alterations that contribute to throat cancer development, potentially identifying novel therapeutic targets. By studying the genetic makeup of tumors from HPV-positive patients, researchers could identify specific genetic mutations and alterations that may drive tumor growth. This could lead to the development of personalized treatment strategies tailored to the genetic profile of each patient’s cancer.
Addressing Limitations of the Current Study
The current study might have limitations regarding sample size, geographic diversity, or specific populations. Future research should address these limitations by expanding the study population to include diverse ethnic and socioeconomic groups and geographically dispersed individuals. This would provide a more representative sample, reducing potential biases and enhancing the generalizability of the findings. A larger and more diverse cohort will enable a more precise understanding of the HPV-throat cancer link in different populations.
Future Research Directions – Table
| Research Question | Methodology | Expected Outcomes |
|---|---|---|
| What is the relationship between specific HPV subtypes and throat cancer progression? | Comparative analysis of HPV subtype prevalence in throat cancer patients versus healthy controls, longitudinal follow-up studies of HPV-infected individuals. | Identification of high-risk HPV subtypes, potential biomarkers for progression, and development of targeted prevention strategies. |
| How do environmental and lifestyle factors interact with HPV infection to influence throat cancer risk? | Longitudinal cohort studies, multivariate analyses of lifestyle factors and HPV infection status in relation to cancer development. | Refinement of risk assessment models incorporating environmental and lifestyle factors, identification of synergistic effects, and development of preventive measures. |
| What is the role of the immune response in the development and progression of HPV-related throat cancer? | Immunological profiling of HPV-infected individuals with and without throat cancer, analysis of immune cell profiles and cytokine levels. | Identification of biomarkers for early detection and disease progression, potential targets for immunotherapy, and understanding of the immune response’s role in viral clearance or tumorigenesis. |
| How can advanced genomic technologies enhance our understanding of HPV-related throat cancer? | Whole-exome sequencing of tumors from HPV-positive patients, bioinformatics analysis of genetic alterations. | Identification of novel therapeutic targets, personalized treatment strategies, and improved understanding of the molecular mechanisms driving throat cancer development. |
Final Wrap-Up
In conclusion, the HPV throat cancer link study offers a significant step forward in understanding the complexities of this disease. The study’s findings provide crucial insights into the diagnosis, treatment, and prevention of HPV-related throat cancer, offering valuable implications for both clinical practice and public health initiatives. The discussion of limitations and future research directions ensures a holistic understanding of the subject matter, paving the way for further advancements in the fight against this disease.
The study’s impact on public health, including potential prevention strategies and awareness programs, will be explored in the final section.