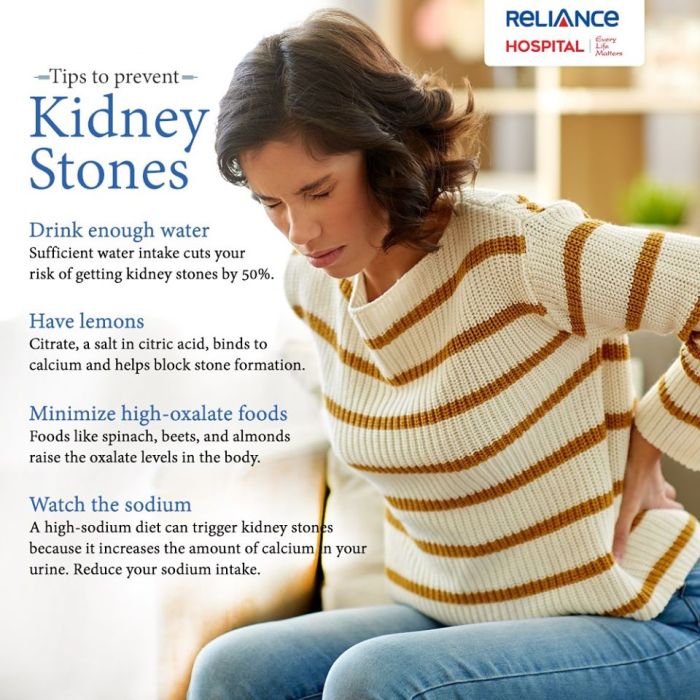
How to prevent kidney stones? This guide dives deep into the crucial aspects of diet, lifestyle, and medical management to help you understand and actively prevent kidney stones. We’ll explore dietary considerations, like the foods to limit and the ones to embrace, as well as the impact of exercise and weight management. You’ll also learn about medical treatments, hydration strategies, and the role of supplements in preventing these painful stones.
Get ready to take control of your kidney health!
Kidney stones, those painful crystals that form in your kidneys, can significantly impact your quality of life. Understanding the various risk factors and implementing preventative strategies is key to avoiding this common ailment. This comprehensive guide will equip you with the knowledge to make informed choices and reduce your risk, focusing on dietary changes, lifestyle modifications, and medical interventions.
Dietary Considerations for Kidney Stone Prevention: How To Prevent Kidney Stones
Kidney stones, painful mineral deposits that form in the kidneys, can be significantly impacted by dietary choices. Understanding which foods to limit and which to embrace is crucial for preventing their formation. This section dives into the specifics of dietary management for kidney stone prevention, covering everything from specific food groups to recommended daily intakes and detailed examples.Dietary factors play a vital role in kidney stone formation.
A balanced approach, focusing on limiting certain foods while incorporating beneficial nutrients, is key to preventing and managing kidney stones. This section details the dietary strategies that can significantly reduce the risk of developing these painful conditions.
Foods to Limit or Avoid
Certain foods contribute to the formation of kidney stones by increasing the concentration of minerals like calcium oxalate and uric acid in the urine. Reducing intake of these foods can significantly lower the risk of stone development. Foods to limit or avoid include high-oxalate foods, excessive sodium, and certain types of protein.
- High-Oxalate Foods: Many fruits, vegetables, and nuts contain high levels of oxalates. These compounds can combine with calcium in the urine to form kidney stones. While complete elimination isn’t necessary, moderation is key. Common culprits include spinach, rhubarb, beets, chocolate, nuts, and some berries. Careful portion control and strategic substitutions are crucial.
- Excessive Sodium: A high-sodium diet can lead to increased calcium excretion in the urine, which can promote stone formation. Processed foods, fast food, and many restaurant meals often contain high levels of sodium. Reading food labels carefully and choosing low-sodium alternatives can significantly reduce sodium intake.
- Animal Protein: Consuming excessive amounts of animal protein, particularly red meat and processed meats, can increase uric acid levels in the urine. High uric acid levels can contribute to the formation of certain types of kidney stones, such as uric acid stones. Substituting animal protein with plant-based protein sources like beans, lentils, and tofu can help reduce the risk.
Recommended Daily Intake of Nutrients
The recommended daily intake of calcium, sodium, and protein plays a significant role in kidney stone prevention. Maintaining a balance in these nutrient levels is crucial to avoiding stone formation.
- Calcium: Calcium is essential for many bodily functions, but excessive intake can contribute to kidney stones. However, adequate calcium intake is necessary to prevent the body from drawing on calcium stores in the bones. The key is finding the right balance. Consult a healthcare professional to determine the appropriate daily calcium intake for your individual needs.
- Sodium: Limiting sodium intake is crucial for preventing kidney stones. The recommended daily intake of sodium varies based on individual needs and health conditions. A diet rich in fresh fruits and vegetables, whole grains, and lean proteins, and limiting processed foods, can effectively lower sodium intake.
- Protein: Protein is vital for maintaining healthy tissues, but excessive protein intake can increase the risk of kidney stones. Moderation is key. Focusing on lean protein sources and balancing protein intake with a diet rich in fruits, vegetables, and whole grains can help to prevent potential issues. The optimal protein intake varies based on individual factors and should be determined in consultation with a healthcare professional.
Different Types of Kidney Stones and Dietary Triggers
Kidney stones come in various forms, each with its own dietary triggers. Understanding these differences is important for personalized dietary interventions.
- Calcium Oxalate Stones: These are the most common type of kidney stone. High oxalate intake, insufficient calcium intake, and high sodium intake can all contribute to their formation.
- Uric Acid Stones: These stones form when there is too much uric acid in the urine. High consumption of animal protein and certain foods high in purines can increase uric acid levels.
- Struvite Stones: These stones are often associated with urinary tract infections. A diet that promotes a healthy urinary tract is crucial for prevention.
- Cystine Stones: These stones are less common and are caused by a genetic disorder that affects the way the body handles cystine.
Sample Weekly Meal Plan
A sample weekly meal plan designed to reduce kidney stone risk factors emphasizes a balanced intake of fruits, vegetables, lean proteins, and whole grains. Portion sizes should be adjusted based on individual needs and health conditions.
Preventing kidney stones involves a lot of lifestyle choices, like staying hydrated and eating a balanced diet. It’s also important to consider what you eat and avoid if you have immune thrombocytopenia (ITP), a condition affecting blood platelets. For instance, understanding the foods to eat and avoid with itp can significantly impact your overall health and help manage your kidney stone risk.
Ultimately, a combination of these strategies is key to good kidney health.
- Monday: Grilled chicken breast with steamed broccoli and quinoa, a side salad with vinaigrette dressing.
- Tuesday: Baked salmon with roasted asparagus and brown rice, a small portion of mixed berries.
- Wednesday: Lentil soup with whole-wheat bread, a side salad with light vinaigrette dressing.
- Thursday: Lean ground turkey with sweet potato and green beans.
- Friday: Chicken stir-fry with plenty of vegetables, brown rice.
- Saturday: Vegetarian chili with whole-wheat crackers, a side salad.
- Sunday: Lean beef stir-fry with mixed vegetables, brown rice.
High-Oxalate Foods and Alternatives
Avoiding high-oxalate foods entirely is often impractical. Strategic substitutions and portion control can help reduce oxalate intake without sacrificing flavor or nutrients.
- High-Oxalate Foods: Spinach, rhubarb, beets, chocolate, nuts, some berries, and tea.
- Alternative Options: Leafy greens like kale or collard greens can be substituted, as can other fruits and vegetables.
Role of Hydration in Preventing Kidney Stones
Adequate hydration is crucial for flushing out minerals and preventing the formation of kidney stones.
- Drinking plenty of water helps dilute the concentration of minerals in the urine, reducing the risk of crystal formation.
Lifestyle Modifications for Kidney Stone Prevention
Maintaining a healthy lifestyle is crucial in preventing kidney stones. Beyond dietary considerations, specific lifestyle modifications can significantly reduce the risk of stone formation. Regular exercise, weight management, and stress reduction all play a vital role in optimizing kidney health. These strategies, when implemented consistently, can lead to a substantial decrease in the likelihood of experiencing future kidney stone episodes.Effective prevention of kidney stones extends beyond diet alone.
Lifestyle choices influence kidney function and overall health, contributing to a lower risk of stone development. This section explores the vital connection between lifestyle factors and kidney stone prevention.
Regular Exercise and Kidney Stone Prevention
Regular physical activity is essential for overall health and plays a critical role in preventing kidney stones. Exercise helps maintain a healthy weight, regulates blood pressure, and promotes the excretion of certain substances that can contribute to stone formation. Physical activity also improves the function of the kidneys.
Obesity and Kidney Stone Risk
Obesity is a significant risk factor for kidney stones. Excess body weight, particularly abdominal obesity, increases the risk of several metabolic abnormalities, such as hyperuricosuria, which promotes the formation of uric acid stones. Moreover, obesity often leads to an increase in calcium excretion, further increasing the chance of calcium-based kidney stone formation.
Optimal Weight Management Strategies
Effective weight management strategies are crucial for kidney stone prevention. A gradual, sustainable weight loss approach, typically no more than 1-2 pounds per week, is recommended. This approach focuses on a balanced diet and regular exercise rather than extreme measures. A registered dietitian or healthcare professional can help develop a personalized weight management plan. Combining diet with regular exercise, tailored to individual needs and preferences, can significantly reduce the risk of developing kidney stones.
This approach considers individual factors, dietary habits, and current fitness levels to promote sustained weight loss and overall health.
Exercise Plan for Kidney Stone Prevention
An exercise plan for individuals prone to kidney stones should prioritize low-impact activities. This approach minimizes stress on the kidneys while maximizing their function. A sample plan might include:
- Cardiovascular Exercise: 30 minutes of brisk walking, swimming, or cycling most days of the week. These activities improve cardiovascular health, regulate blood pressure, and promote healthy kidney function.
- Strength Training: Two or three times per week, focusing on exercises that target major muscle groups. Strength training helps maintain muscle mass, which is essential for overall health and can positively impact kidney function.
- Flexibility and Balance Exercises: Incorporating stretching and balance exercises, such as yoga or tai chi, helps improve flexibility and reduce the risk of falls. Improved flexibility can indirectly contribute to kidney stone prevention.
It’s crucial to consult with a healthcare professional before starting any new exercise program, especially if there are existing health conditions. A personalized exercise plan tailored to individual needs and abilities is essential.
Stress Management Techniques
Stress can indirectly influence kidney stone formation. High levels of stress can lead to fluctuations in hormone levels, which may affect calcium and oxalate metabolism. Stress management techniques can help mitigate these effects. Practices such as meditation, deep breathing exercises, yoga, or spending time in nature can help regulate stress levels.
Staying hydrated and eating a balanced diet are key to preventing kidney stones. Plus, just like keeping your body internally clean, taking care of your scalp’s health contributes to overall well-being. Exfoliating your scalp, for example, can help remove dead skin cells and promote healthy hair growth. Check out this guide on how to exfoliate your scalp for clean healthy hair for some helpful tips.
This, in turn, indirectly supports a healthier body, further reducing your risk of kidney stones.
Maintaining a Healthy Weight for Kidney Stone Prevention
Maintaining a healthy weight is a crucial aspect of kidney stone prevention. By maintaining a healthy weight, individuals can reduce their risk of developing metabolic conditions that contribute to stone formation. Weight management is not only about reducing risk, but it also improves overall health and well-being. A healthy weight contributes to improved blood pressure, reduced calcium excretion, and a decreased risk of developing conditions like hyperuricosuria.
Staying hydrated is key to preventing kidney stones, along with a balanced diet low in sodium and oxalate-rich foods. But beyond physical well-being, building self-esteem is crucial, especially when facing a health condition like vitiligo. Learning to embrace your unique beauty and focusing on inner strength can significantly impact your overall health journey. For more insights on how to navigate vitiligo and build self-esteem, check out this helpful resource: vitiligo building self esteem.
Ultimately, a proactive approach to kidney stone prevention, coupled with a positive mindset, is vital for a healthier life.
Medical Treatments and Management
Kidney stones, while often preventable through dietary and lifestyle changes, sometimes require medical intervention. Understanding the role of medications and various treatment procedures is crucial for individuals at risk or experiencing stone formation. This section delves into the medical approaches to managing kidney stones, focusing on prevention and treatment strategies.Medical interventions for kidney stones vary greatly depending on the size, location, and type of stone, as well as the patient’s overall health.
Some stones pass spontaneously, while others may necessitate more aggressive treatment. The goal of medical management is to ensure the stone’s passage or to remove it safely, minimizing discomfort and potential complications.
Medications for Kidney Stone Prevention
Certain medications can effectively reduce the risk of kidney stone formation by altering the body’s chemical balance. These medications primarily target the factors contributing to stone formation, such as calcium excretion and pH levels in the urine. Careful monitoring and consultation with a healthcare professional are essential to ensure the medication’s effectiveness and safety.
| Medication | Mechanism of Action | Potential Side Effects |
|---|---|---|
| Thiazide diuretics | Reduce calcium excretion by increasing calcium reabsorption in the kidneys. This lowers the concentration of calcium in the urine, making it less likely for calcium stones to form. | Dehydration, dizziness, and potential electrolyte imbalances (e.g., low potassium). |
| Potassium citrate | Increases urinary citrate levels. Citrate inhibits the formation of calcium stones by binding to calcium ions in the urine. | Diarrhea, nausea, vomiting. |
| Allopurinol | Reduces the production of uric acid, which can contribute to the formation of uric acid stones. | Skin rash, nausea, and liver problems. |
Medical Interventions for Kidney Stone Treatment
Medical interventions for kidney stones range from conservative approaches to more invasive procedures. The choice of intervention depends on various factors, including the stone’s size, location, and the patient’s overall health.
- Extracorporeal Shock Wave Lithotripsy (ESWL): This non-invasive procedure uses shock waves to break down large stones into smaller fragments that can be passed in urine. It’s often the first choice for kidney stones that are not too large or complex.
- Ureteroscopy (URS): This procedure uses a small, flexible scope inserted through the urethra to visualize and remove stones lodged in the ureter. It’s particularly useful for stones in the lower part of the urinary tract.
- Percutaneous Nephrolithotomy (PCNL): For very large or complex kidney stones, PCNL involves making a small incision in the back to access the kidney and remove the stone using instruments.
- Surgical Removal: In rare cases, open surgery may be necessary to remove extremely large or complicated kidney stones.
Importance of Regular Check-ups and Monitoring
Regular check-ups and monitoring are essential for individuals at risk of kidney stones. This allows healthcare professionals to identify potential issues early and intervene promptly. Monitoring urine tests, blood work, and imaging can provide valuable insights into the patient’s stone risk and treatment response. This proactive approach is vital for preventing complications and maintaining overall kidney health.
Early detection and intervention can often prevent the need for more aggressive treatment options.
Hydration and Fluid Intake
Staying well-hydrated is crucial for kidney stone prevention. Adequate fluid intake helps dilute urine, reducing the concentration of minerals that can form stones. Proper hydration also promotes healthy kidney function and helps flush out potential stone-forming substances. This section will explore the importance of hydration, providing recommendations for daily intake, highlighting different types of fluids, and emphasizing the role of urine pH in kidney stone prevention.
Importance of Adequate Fluid Intake
Maintaining a sufficient fluid intake is essential for preventing kidney stones. A well-hydrated body helps dilute the concentration of minerals in the urine, reducing the risk of these minerals crystallizing and forming stones. When urine becomes too concentrated, minerals like calcium, oxalate, and uric acid can precipitate out, leading to stone formation. A healthy fluid intake keeps urine adequately diluted, minimizing the chances of this happening.
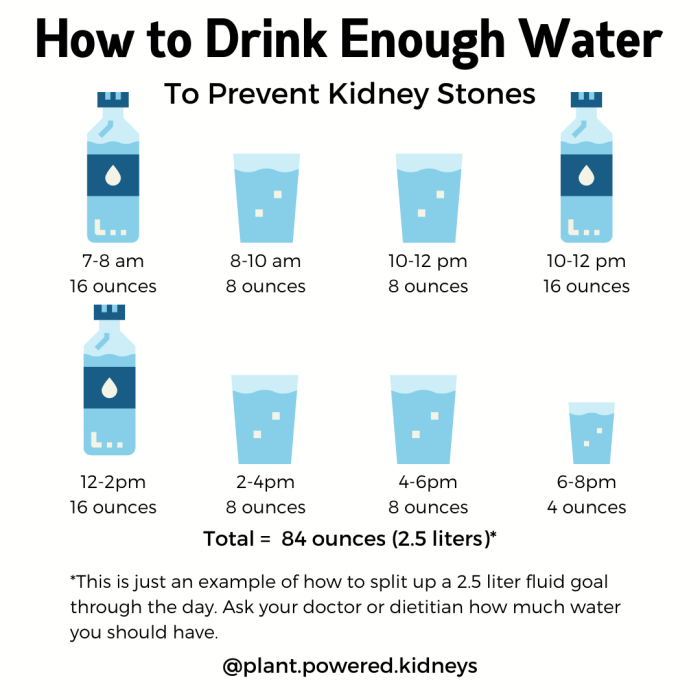
Recommendations for Daily Fluid Intake
Daily fluid needs vary based on factors such as activity level, climate, and overall health. A general guideline is to drink enough fluids to produce at least 2 liters (approximately 8 glasses) of urine per day. However, individual needs may differ. Those who exercise intensely or live in hot climates may need to drink more. It’s crucial to listen to your body’s cues and adjust fluid intake accordingly.
Different Types of Fluids for Kidney Stone Prevention
Various fluids contribute to hydration and may affect urine pH differently. Water is the most effective choice for maintaining proper hydration and diluting urine. Other beverages like unsweetened tea and diluted fruit juices can also be part of a healthy hydration plan. Keep in mind that some beverages can influence urine pH and should be considered within the context of overall dietary intake.
Maintaining Proper Hydration Throughout the Day
Consistent hydration throughout the day is more effective than sporadic bursts of drinking. Carry a water bottle and sip on it regularly, especially during and after physical activity. Schedule reminders on your phone to ensure you’re drinking fluids at regular intervals. Don’t wait until you feel thirsty to drink; thirst is often a sign of mild dehydration.
Role of Urine pH in Kidney Stone Prevention
Urine pH plays a significant role in kidney stone formation. Certain stones, such as calcium oxalate stones, are more likely to form in acidic urine. Maintaining a balanced urine pH within a specific range can help prevent the formation of these stones. A diet rich in fruits and vegetables tends to alkalinize the urine, while a diet high in protein and processed foods can make urine more acidic.
Monitoring urine pH through testing strips or dietary adjustments can help prevent stone formation.
Specific Beverages to Include and Exclude
- Include: Water is the cornerstone of hydration. Unsweetened herbal teas and diluted fruit juices (like diluted apple or cranberry juice) are also beneficial. These fluids contribute to overall hydration without the added sugar or acidity that can be detrimental.
- Exclude: Sugary sodas and highly caffeinated beverages should be limited. High caffeine intake can lead to dehydration, and sugary drinks add unnecessary calories and can contribute to other health issues. Excessive consumption of these beverages may increase the risk of kidney stones. Consider these as occasional treats rather than regular parts of your daily routine.
Supplements and Dietary Aids
Kidney stones, unfortunately, can be a recurring problem for many. While dietary changes and lifestyle modifications are crucial, supplements and certain dietary aids can play a supporting role in preventing stone formation. This section delves into the potential benefits and risks of various supplements, highlighting the importance of professional guidance before starting any new regimen.Dietary supplements are not a substitute for a balanced diet and healthy lifestyle.
They should be used as part of a comprehensive strategy for preventing kidney stones, and only under the guidance of a healthcare professional. It is essential to remember that supplements can interact with medications, and certain individuals may have specific sensitivities.
Potential Supplements for Kidney Stone Prevention
Understanding the role of various vitamins and minerals in kidney stone formation is crucial. Some supplements may help manage the levels of certain substances in the body that contribute to stone development. Careful consideration of individual needs and potential interactions is vital.
- Potassium Citrate: This supplement can help increase urine citrate levels, which can help prevent calcium stones from forming. Increased citrate in urine makes the environment less conducive to stone formation. However, some individuals may experience digestive discomfort, such as diarrhea or gas, as a side effect.
- Magnesium Supplements: Magnesium is a mineral that can help prevent calcium oxalate stones by binding to oxalate in the digestive tract, reducing its absorption into the bloodstream. The recommended intake of magnesium varies based on individual needs and should be determined by a healthcare professional. Potential side effects include diarrhea and nausea.
- Vitamin B6: Vitamin B6 can help reduce oxalate levels in the body, which is beneficial for those prone to calcium oxalate stones. High doses of Vitamin B6 may lead to nerve damage, so consulting a doctor is crucial before taking any supplements.
- Vitamin D: While vitamin D is important for calcium absorption, excessive intake can increase calcium levels in the blood, potentially increasing the risk of kidney stones. The optimal levels of Vitamin D are dependent on individual factors and should be discussed with a doctor. Too much vitamin D can lead to hypercalcemia.
Role of Specific Vitamins and Minerals
The balance of vitamins and minerals plays a critical role in overall health and kidney function. Certain vitamins and minerals can either support or hinder the prevention of kidney stones. This balance is highly personalized and should be discussed with a qualified healthcare professional.
- Calcium: Calcium, although important for bone health, can contribute to kidney stone formation if not balanced with other nutrients. The source of calcium (e.g., dairy, supplements) and overall dietary pattern significantly impact its effect on kidney stone formation.
- Oxalate: Oxalate is a substance found in many foods that can contribute to calcium oxalate kidney stones. Dietary changes to reduce oxalate-rich foods may be helpful. However, it’s important to maintain a balanced diet.
Importance of Professional Consultation
“It is strongly recommended that individuals consult with a healthcare professional before starting any supplement regimen, especially if they have underlying health conditions or are taking other medications.”
Consultations with a doctor are necessary to determine the right dosage and whether the supplement is appropriate for an individual’s specific health situation. This helps avoid potential adverse interactions or exacerbating existing conditions. Dosage and individual needs should be determined by a healthcare professional.
Comparing Dietary Aids, How to prevent kidney stones
Various dietary aids can support kidney stone prevention, but their effectiveness varies depending on individual factors. Some popular options include certain fruits, vegetables, and herbal remedies. The effectiveness of any specific aid should be discussed with a healthcare professional.
Supplement Comparison Table
| Supplement | Potential Benefits | Potential Risks |
|---|---|---|
| Potassium citrate | May help prevent calcium stones by increasing urine citrate levels. | May cause digestive upset, such as diarrhea or gas. |
| Magnesium | May help prevent calcium oxalate stones by binding to oxalate. | May cause diarrhea or nausea in high doses. |
| Vitamin B6 | May help reduce oxalate levels. | High doses may cause nerve damage. |
| Vitamin D | Important for calcium absorption. | High doses can increase calcium levels in the blood, potentially increasing kidney stone risk. |
Risk Factors and Prevention Strategies
Kidney stones, those painful crystalline deposits that form in the kidneys, can be a significant health concern. Understanding the risk factors and adopting preventative measures are crucial in reducing the likelihood of developing them. A proactive approach to lifestyle and dietary choices, combined with appropriate medical management, can dramatically lower the chances of experiencing this agonizing condition.Understanding the interplay of genetic predisposition, underlying medical conditions, and dietary habits is key to developing a personalized strategy for preventing kidney stones.
This involves recognizing your individual risk factors and implementing tailored prevention methods. This section will delve into the factors that contribute to kidney stone formation, offering insights into preventive strategies and highlighting the importance of proactive health management.
Risk Factors for Kidney Stone Development
Several factors contribute to the formation of kidney stones. These include a family history of kidney stones, certain medical conditions, and dietary habits. Understanding these factors is the first step towards implementing effective prevention strategies.
Family History and Kidney Stone Formation
A strong family history of kidney stones significantly increases an individual’s risk. If a parent or sibling has had kidney stones, the individual is more likely to develop them. This genetic predisposition suggests that certain genetic factors may influence the body’s ability to regulate the minerals that contribute to stone formation. This heightened risk underscores the importance of early intervention and proactive lifestyle modifications in those with a family history.
Medical Conditions and Kidney Stone Risk
Certain medical conditions increase the likelihood of kidney stone formation. These include conditions like gout, hyperparathyroidism, and inflammatory bowel disease. These conditions often lead to imbalances in mineral levels or changes in urine composition, making the individual more susceptible to stone formation. For example, individuals with hyperparathyroidism have elevated calcium levels, which can promote the formation of calcium-based stones.
Proactive management of these underlying conditions is essential to reduce the risk.
Preventive Measures for Individuals with Family History
Individuals with a family history of kidney stones should take proactive measures to minimize their risk. These measures include maintaining a healthy weight, consuming sufficient fluids, and adhering to a diet low in oxalate and purine-rich foods. This proactive approach may significantly reduce the chances of developing kidney stones.
Individuals at High Risk for Kidney Stones
Several groups of individuals are at a higher risk of developing kidney stones. These include individuals with a family history, those with certain medical conditions, and those with a diet high in calcium-rich foods. Additionally, individuals who are inactive, obese, or have a history of urinary tract infections (UTIs) are also at increased risk.
Flowchart for Assessing and Managing Kidney Stone Risk
| Step | Action |
|---|---|
| 1 | Assess Family History: Determine if there is a family history of kidney stones. |
| 2 | Evaluate Medical Conditions: Identify any underlying medical conditions that may increase the risk of kidney stones (e.g., hyperparathyroidism, gout). |
| 3 | Dietary Analysis: Analyze current dietary habits, particularly regarding fluid intake, oxalate, and purine content. |
| 4 | Hydration Assessment: Evaluate daily fluid intake. |
| 5 | Lifestyle Evaluation: Assess physical activity levels and weight. |
| 6 | Consultation with Healthcare Professional: Discuss findings with a healthcare professional for personalized recommendations and management. |
Final Review
In conclusion, preventing kidney stones is a multifaceted approach that involves dietary adjustments, lifestyle changes, and potentially medical interventions. By understanding the role of diet, hydration, and exercise, you can significantly lower your risk. Remember to consult with your healthcare provider for personalized advice and monitoring. Armed with this knowledge, you can proactively safeguard your kidney health and enjoy a better quality of life.