Carrot and turmeric juice is a vibrant beverage packed with potential health benefits. This drink, made from the potent combination of carrots and turmeric, promises a powerful punch of vitamins, minerals, and antioxidants. Common preparation methods include blending the ingredients together, offering a customizable and easily digestible way to consume these nutritional powerhouses. From historical uses to modern health trends, this juice holds a fascinating place in the world of wellness.
This post delves into the nutritional value and potential health benefits of carrot and turmeric juice, exploring the key vitamins, minerals, and antioxidants. We’ll also discuss potential drawbacks, recipes, and how to incorporate this drink into a balanced diet. Get ready to uncover the secrets behind this trendy beverage!
Introduction to Carrot and Turmeric Juice
Carrot and turmeric juice is a vibrant beverage gaining popularity for its potential health benefits. This refreshing drink combines the earthy sweetness of carrots with the warm spice of turmeric, offering a unique flavor profile and a possible boost to overall well-being. Often touted for its antioxidant properties and anti-inflammatory effects, it’s a delicious way to potentially enhance your diet.
The combination of these two ingredients provides a blend of vitamins, minerals, and phytonutrients that could contribute to a healthier lifestyle.This juice is a simple and flavorful way to incorporate these beneficial ingredients into your daily routine. Understanding its key ingredients, potential benefits, and preparation methods can empower you to make informed choices about its role in your health journey.
The nutritional profile, while estimated, can offer a glimpse into the potential contribution of this beverage to your daily intake.
Key Ingredients
Carrot and turmeric juice is primarily composed of carrots and turmeric. Carrots are a well-known source of beta-carotene, which the body converts to vitamin A. Turmeric, a spice commonly used in Indian cuisine, boasts curcumin, a potent antioxidant. These ingredients, along with any other additions like ginger or lemon, contribute to the drink’s unique taste and potential health advantages.
Potential Health Benefits
Carrot and turmeric juice is often associated with a variety of potential health benefits. The beta-carotene in carrots is crucial for eye health, promoting good vision. Turmeric’s curcumin is known for its potential anti-inflammatory properties, which may support joint health and overall well-being. The combination of these nutrients could also contribute to improved immunity and potentially aid in digestion.
Preparation Methods
Preparing carrot and turmeric juice is straightforward. A simple blender is sufficient to create a smooth, vibrant beverage. Simply chop the carrots and turmeric root, add any optional ingredients like ginger or lemon, and blend until smooth. The juice can be strained for a smoother texture if desired.
Historical Context and Cultural Significance
Carrots have a long history, with evidence of cultivation dating back centuries. Turmeric, a staple in Indian cuisine, has been used for centuries for both culinary and medicinal purposes. In various cultures, these ingredients have played significant roles in both nutrition and traditional medicine, emphasizing their importance in different societies.
Nutritional Content
| Nutrient | Carrot | Turmeric | Carrot & Turmeric Juice (estimated) |
|---|---|---|---|
| Vitamin A | High | Low | Medium |
| Vitamin C | Medium | Low | Medium |
| Potassium | Medium | Low | Medium |
| Fiber | High | Medium | Medium |
| Antioxidants | Medium | High | High |
The table above provides an estimated nutritional breakdown. The actual amounts may vary based on the specific ingredients and preparation methods used. It’s important to consult a healthcare professional for personalized dietary advice.
Nutritional Value and Benefits
Carrot and turmeric juice, a vibrant blend of these powerful ingredients, offers a potent punch of nutrients and potential health benefits. This combination taps into the rich nutritional profiles of both carrots and turmeric, delivering a delicious and potentially restorative beverage. The synergy of their properties could contribute to overall well-being, but as with any dietary change, consulting a healthcare professional is recommended, especially for those with pre-existing conditions.The remarkable nutritional value of this juice stems from the unique properties of carrots and turmeric.
Carrots are a fantastic source of vitamins and minerals, while turmeric boasts potent anti-inflammatory and antioxidant compounds. Understanding the precise contributions of each ingredient is key to appreciating the holistic impact on health.
Key Vitamins, Minerals, and Antioxidants
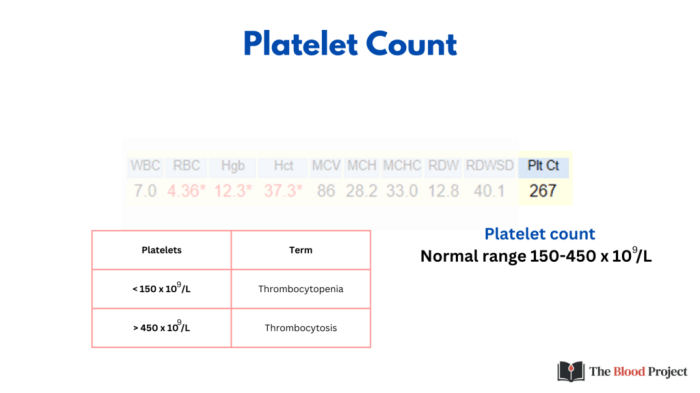
Carrots are rich in beta-carotene, a precursor to vitamin A, essential for healthy vision, immune function, and cell growth. They also contain vitamin K, important for blood clotting and bone health, and various B vitamins, crucial for energy production and metabolism. Turmeric, on the other hand, is renowned for its curcumin content, a potent antioxidant and anti-inflammatory compound. Other vitamins and minerals present in varying amounts include potassium, calcium, and iron.
This combination provides a broad spectrum of nutrients that can positively influence various bodily functions.
Potential Health Benefits
The unique combination of nutrients in carrot and turmeric juice may offer a range of health benefits. These include potential anti-inflammatory effects, antioxidant protection, support for digestive health, and potential immune system support. However, further research is needed to fully understand the extent of these benefits. These potential advantages stem from the specific vitamins, minerals, and bioactive compounds within each ingredient.
I’ve been experimenting with carrot and turmeric juice lately, and while it’s definitely a delicious drink, I’ve also been researching its potential benefits. Learning about stage 3 lung cancer overview stage 3 lung cancer overview has made me think about how important preventative measures are. While I’m not a doctor, I’m still exploring the idea that a healthy diet like one including carrot and turmeric juice might play a role in overall well-being.
Comparison to Other Beverages
Compared to other juices, carrot and turmeric juice stands out due to its potent combination of antioxidants and anti-inflammatory properties. While other fruit juices offer vitamins and minerals, the unique blend of curcumin and beta-carotene distinguishes this beverage. A direct comparison could include vegetable juices, but the emphasis on turmeric’s anti-inflammatory properties gives this blend a unique characteristic.
Table of Potential Health Benefits
| Benefit | Description | Evidence | Caveats |
|---|---|---|---|
| Anti-inflammatory | Carrot and turmeric juice may help reduce inflammation in the body. | Some studies suggest a positive correlation, but more research is needed. | Individual responses may vary, and further research is required to establish conclusive evidence. |
| Antioxidant | The presence of antioxidants like curcumin and beta-carotene can protect cells from damage. | Strong evidence exists supporting the antioxidant properties of curcumin and beta-carotene. | A balanced diet rich in various antioxidants is crucial; this juice should not replace a healthy lifestyle. |
| Digestive health | The fiber content of carrots and potential benefits of turmeric may support healthy digestion. | Some evidence suggests a positive impact on digestive function. | Individual responses may vary, and further research is needed to establish conclusive evidence. |
| Immune system support | The vitamins and minerals in the juice may contribute to a healthy immune response. | Some evidence supports this, but more research is needed to fully understand the extent of this impact. | This juice should not be considered a cure-all; a healthy lifestyle is essential for a strong immune system. |
Potential Drawbacks and Considerations

While carrot and turmeric juice offers numerous health benefits, it’s crucial to be aware of potential drawbacks and considerations. Understanding these aspects allows for responsible consumption and ensures the juice complements, rather than compromises, overall health. Careful consideration of potential side effects, interactions, and moderation is key to maximizing the positive impact of this beverage.
Potential Side Effects
Consuming large quantities of carrot and turmeric juice, like any concentrated food, can lead to digestive issues in some individuals. This can manifest as an upset stomach, nausea, or diarrhea. Furthermore, certain individuals may experience allergic reactions, such as skin rashes or itching, due to sensitivities to carrots or turmeric. These reactions can vary in severity and are crucial to monitor closely.
Interactions with Medications, Carrot and turmeric juice
Some medications, particularly blood thinners, may interact with components of carrot and turmeric juice. This interaction could potentially affect the efficacy of the medication or increase the risk of side effects. It’s essential to consult with a doctor or pharmacist before consuming carrot and turmeric juice if you’re taking any medications. This is especially vital if you have existing health conditions, as the juice may interact with treatment regimens.
Importance of Moderation and Balanced Nutrition
Carrot and turmeric juice should be viewed as a complementary part of a balanced diet, not a replacement. While the juice offers valuable nutrients, consuming it in isolation won’t provide all the essential vitamins, minerals, and fiber necessary for optimal health. Focusing on a varied diet rich in fruits, vegetables, and whole grains alongside the juice will offer a more comprehensive nutritional intake.
Excessive consumption of the juice might lead to an imbalance in the body’s nutritional intake. For instance, overconsumption could lead to a deficiency in certain vitamins or minerals not found in the juice, while a diet lacking in other important nutrients might not benefit from the juice.
I’ve been loving this carrot and turmeric juice lately – it’s got a vibrant orange hue and a surprisingly smooth texture. Speaking of health, have you ever wondered about the safety of getting a flu shot if you have diabetes? Learning more about this could be really helpful for making informed decisions. Checking out this article on diabetes and the flu shot is it safe will give you more insights.
Regardless, I’m sticking with my daily dose of carrot and turmeric juice for its potential health benefits.
Potential Allergic Reactions or Sensitivities
Allergic reactions to carrots or turmeric, although rare, can occur. Symptoms might range from mild skin irritation to more severe reactions. Individuals with known allergies to these ingredients should avoid consuming carrot and turmeric juice. Similarly, individuals with pre-existing conditions, such as those with a history of digestive issues, should exercise caution when introducing the juice into their diet.
Careful monitoring and consideration are essential for these individuals.
I’ve been experimenting with carrot and turmeric juice lately, and I’m finding it surprisingly refreshing. While researching its potential health benefits, I stumbled upon information about neurofibromatosis type 2 NF2, a genetic disorder that can impact nerve function. Neurofibromatosis type 2 nf2 is fascinating, but I’m more focused on how this juice might support overall wellness, potentially boosting antioxidants and aiding digestion.
I’ll keep experimenting with different recipes and report back on my findings. Carrot and turmeric juice is definitely worth a try!
Table of Potential Side Effects and Precautions
| Side Effect | Description | Severity | Mitigation |
|---|---|---|---|
| Digestive issues | Upset stomach, diarrhea | Mild | Drink in moderation and slowly introduce into your diet. |
| Allergic reactions | Skin rash, itching, swelling | Varies | Avoid if allergic. Consult a doctor if symptoms worsen. |
| Drug interactions | May interact with certain medications | Varies | Consult a doctor or pharmacist before consumption if on any medication. |
| Liver issues | Potential for liver stress | Low (unlikely in moderate amounts) | Consult a doctor if experiencing liver-related symptoms. |
Recipes and Preparation Methods
Carrot and turmeric juice offers a delicious and nutritious way to incorporate these potent ingredients into your daily routine. This section provides various recipes and methods for preparing this vibrant elixir, highlighting different flavor profiles and extraction techniques.
Carrot and Turmeric Juice Recipes
Different flavor combinations can be explored to suit your taste preferences. These recipes provide a starting point for experimentation and adaptation.
| Recipe Name | Ingredients | Preparation Steps | Storage |
|---|---|---|---|
| Classic Carrot Turmeric | 2 medium carrots, 1/2 inch piece of fresh turmeric root, 1 inch piece of fresh ginger, 1/2 lemon | 1. Wash and peel carrots, turmeric, and ginger. 2. Roughly chop the carrots, turmeric, and ginger. 3. Add the ingredients to a juicer or blender. 4. Blend until smooth, adding a little water if needed to achieve desired consistency. 5. Squeeze the juice from half a lemon into the mixture. |
Refrigerate for up to 2 days. |
| Spicy Carrot Turmeric | 2 medium carrots, 1/2 inch piece of fresh turmeric root, 1 inch piece of fresh ginger, 1/4 teaspoon chili flakes (or more to taste) | 1. Wash and peel carrots, turmeric, and ginger. 2. Roughly chop the carrots, turmeric, and ginger. 3. Add the ingredients to a juicer or blender. 4. Blend until smooth, adding a little water if needed to achieve desired consistency. 5. Taste and adjust chili flakes to your desired spice level. |
Refrigerate for up to 2 days. |
| Tropical Carrot Turmeric | 2 medium carrots, 1/2 inch piece of fresh turmeric root, 1/2 cup mango chunks, 1/4 cup pineapple chunks | 1. Wash and peel carrots and turmeric. 2. Roughly chop the carrots and turmeric. 3. Add the ingredients to a juicer or blender. 4. Blend until smooth, adding a little water if needed to achieve desired consistency. |
Refrigerate for up to 2 days. |
Juice Extraction Techniques
Using a juicer is often the most efficient way to extract juice from carrots and turmeric. A good quality centrifugal juicer is recommended for optimal results. For those without a juicer, a high-powered blender can be used, but this might result in a slightly thicker consistency. Adding a little water to the blender can help achieve the desired juice-like consistency.
The choice of appliance depends on personal preference and availability.
Proper Storage of Carrot and Turmeric Juice
Proper storage is crucial to maintain the freshness and nutritional value of the juice. Store the juice in an airtight container in the refrigerator. Avoid leaving the juice at room temperature for extended periods as this can lead to bacterial growth and reduce the juice’s quality. Consume the juice within 2 days of preparation for optimal results.
Carrot and Turmeric Juice in the Context of Overall Health

Carrot and turmeric juice, with its vibrant blend of nutrients, can be a valuable addition to a healthy lifestyle. The potent antioxidants and vitamins found in these ingredients contribute to overall well-being, but it’s crucial to remember that it’s part of a broader approach to health. It shouldn’t replace a balanced diet or regular exercise.Integrating this juice into your daily routine can offer numerous benefits, but it’s essential to understand how it fits within the bigger picture of a healthy lifestyle.
This includes considering its role in a balanced diet and how to incorporate it effectively without neglecting other essential components of a healthy lifestyle.
Role in a Balanced Diet
Carrot and turmeric juice provides a concentrated dose of vitamins, minerals, and antioxidants. However, it’s not a replacement for whole foods. A balanced diet encompassing a variety of fruits, vegetables, lean proteins, and whole grains is crucial for optimal health. This juice can act as a supplement, adding nutrients to an already healthy eating pattern. A balanced diet promotes optimal digestion, energy levels, and immune function.
Focusing on whole, unprocessed foods ensures a comprehensive intake of essential nutrients, while this juice provides a convenient way to enhance the nutritional profile of your diet.
Incorporating into a Healthy Lifestyle
This vibrant beverage can be easily integrated into a healthy lifestyle by incorporating it into existing routines. Drinking it as a part of breakfast, a midday snack, or a post-workout recovery drink can provide a convenient way to boost your daily nutrient intake. It can also be used as a base for smoothies or added to other recipes for a healthy boost.
Combining this juice with other healthy choices like regular exercise and stress management further enhances its potential impact on overall health.
Meal Pairings
This juice complements a variety of meals and snacks, enhancing their nutritional value and overall health benefits. Careful selection of pairings can maximize the positive impact of this beverage on your well-being.
| Meal | Description | Juice Pairing | Rationale |
|---|---|---|---|
| Breakfast Smoothie | Berries, yogurt, oats | Carrot and Turmeric | Provides a healthy start to the day with a blend of antioxidants, probiotics, and complex carbohydrates. |
| Lunch Salad | Mixed greens, chicken, avocado | Carrot and Turmeric | Adds a healthy boost of vitamins and antioxidants to a light and filling lunch. |
| Dinner Side Dish | Roasted vegetables | Carrot and Turmeric | Compliments the meal with added vitamins and a subtly sweet flavor profile. |
| Snack | Apple slices with almond butter | Carrot and Turmeric | A balanced snack with healthy fats, fiber, and antioxidants. |
Ultimate Conclusion: Carrot And Turmeric Juice
In conclusion, carrot and turmeric juice offers a promising blend of nutrients, with potential benefits ranging from anti-inflammatory properties to immune system support. However, it’s essential to understand the potential side effects and the importance of moderation. This juice can be a delicious and convenient addition to a healthy lifestyle, but it’s not a magic bullet. A balanced diet and lifestyle are crucial for optimal health, and this juice can be a valuable part of that plan.
Ultimately, responsible consumption and careful consideration of individual needs are key to maximizing the potential of this potent beverage.








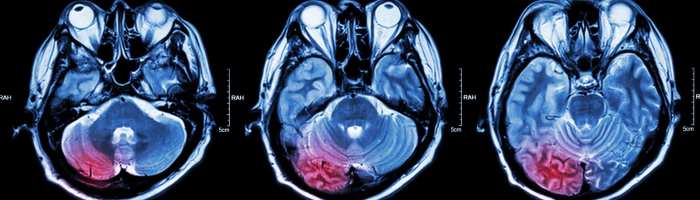
![[100+] Gray Gradient Backgrounds | Wallpapers.com What is gray matter in the brain](https://lyricapills.com/wp-content/uploads/2025/06/wp2249260-1.jpg)