Fiber alternatives to chia seeds offer a wealth of options for boosting your daily fiber intake. Chia seeds are fantastic, but knowing other sources of fiber can help you tailor your diet to your specific needs and preferences. This exploration delves into various alternatives, from flax seeds and psyllium husk to apples, barley, and oats. We’ll compare their nutritional profiles, explore practical applications, and address potential considerations.
This comprehensive guide examines the diverse world of fiber-rich foods, exploring how they can be used in place of or alongside chia seeds. We’ll delve into their nutritional content, usage in various recipes, and how to incorporate them into a healthy diet. Discover the surprising variety of foods packed with fiber and learn how to leverage them for optimal well-being.
Introduction to Fiber Alternatives

Dietary fiber is an essential component of a healthy diet, playing a crucial role in maintaining digestive health and overall well-being. It’s the indigestible part of plant-based foods, promoting regularity, aiding in weight management, and contributing to a balanced gut microbiome. Fiber’s benefits extend to reducing the risk of chronic diseases like heart disease and type 2 diabetes.Consuming adequate fiber is vital for optimal health.
It fosters a healthy digestive system, helping prevent constipation and promoting regular bowel movements. Furthermore, fiber helps regulate blood sugar levels, reducing the risk of spikes and crashes, which is particularly important for individuals with diabetes or those looking to maintain stable energy levels. Fiber also aids in weight management by promoting satiety, making you feel fuller for longer, thus potentially reducing overall calorie intake.
This, in turn, can support weight loss or maintenance efforts.
Looking for fiber-rich alternatives to chia seeds? Well, a healthy diet is crucial for overall well-being, and sometimes, finding alternatives to familiar foods can be a game-changer. For example, if you’re looking to manage hormone levels for specific health goals, like those related to transgender women, understanding options like testosterone blockers for transgender women is key.
Thankfully, flax seeds, psyllium husk, and even certain fruits like berries offer excellent fiber content and can be great substitutes for chia seeds in your daily routine.
Nutritional Profile of Chia Seeds
Chia seeds are renowned for their high fiber content, contributing significantly to their nutritional value. These tiny seeds are packed with omega-3 fatty acids, antioxidants, and various essential minerals, making them a valuable addition to any healthy diet. The fiber in chia seeds is primarily soluble, which helps regulate blood sugar levels and cholesterol. Their unique ability to absorb liquid and form a gel-like consistency makes them a popular ingredient in various recipes, from smoothies to baked goods.
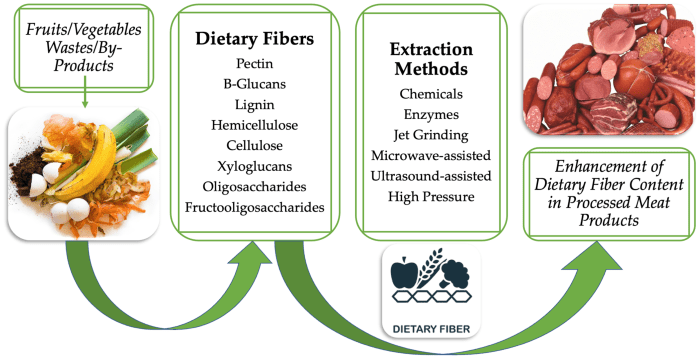
Examples of Different Types of Fiber
Dietary fiber is categorized into two main types: soluble and insoluble. Soluble fiber dissolves in water, forming a gel-like substance that can help lower cholesterol and regulate blood sugar. Insoluble fiber does not dissolve in water and adds bulk to the stool, promoting regularity and preventing constipation. Both types of fiber are vital for digestive health and overall well-being.
Examples of foods rich in soluble fiber include oats, beans, and apples, while whole grains, nuts, and vegetables are good sources of insoluble fiber.
Fiber Alternative Categories
| Name | Source | Fiber Type | Health Benefits |
|---|---|---|---|
| Psyllium Husk | Seeds of the Plantago ovata plant | Mostly soluble | Promotes regularity, lowers cholesterol, and aids in weight management. |
| Flaxseeds | Seed of the flax plant | Both soluble and insoluble | Excellent source of omega-3 fatty acids, promotes satiety, and aids in lowering cholesterol. |
| Oat Bran | Outer layer of oat grain | Mostly insoluble | Promotes regularity, helps lower cholesterol, and adds bulk to the diet. |
| Sweet Potatoes | Root vegetable | Mostly insoluble | Rich in vitamins and minerals, promotes regularity, and provides a good source of antioxidants. |
Comparison of Fiber Content
| Fiber Alternative | Fiber Content (grams per 100g) (Approximate) | Soluble Fiber (grams per 100g) (Approximate) | Insoluble Fiber (grams per 100g) (Approximate) |
|---|---|---|---|
| Chia Seeds | 30-40 | 15-20 | 10-20 |
| Flaxseeds | 25-30 | 10-15 | 10-15 |
| Psyllium Husk | 60-70 | 40-50 | 10-20 |
| Oat Bran | 20-30 | 5-10 | 15-20 |
Note: Fiber content can vary based on the specific preparation and growing conditions.
Exploring Potential Fiber Alternatives
Fiber-rich foods are essential for digestive health and overall well-being. Beyond chia seeds, a wealth of other plant-based options provide significant fiber, each with unique nutritional profiles. This exploration delves into the nutritional content and benefits of various fiber alternatives.Fiber alternatives offer diverse nutritional benefits, and understanding their composition helps us make informed choices for a balanced diet.
This section provides detailed information on the fiber content and other nutritional aspects of flax seeds, psyllium husk, apples, barley, and oats, highlighting their potential as substitutes for chia seeds.
Flax Seeds: A Nutritional Powerhouse
Flax seeds are a popular source of fiber, offering a unique blend of nutrients. They are a good source of lignans, which have antioxidant properties and are associated with potential health benefits. Flax seeds are also rich in omega-3 fatty acids, contributing to heart health. Their fiber content is primarily composed of soluble and insoluble fiber, promoting regularity and satiety.
The fiber in flax seeds contributes to digestive health and may also support blood sugar control.
Looking for fiber-rich alternatives to chia seeds? Many people find chia seeds a bit too “intense” in texture or flavor. Fortunately, there are plenty of other options out there, from flaxseeds and psyllium husk to various vegetables. Choosing the right fiber alternative can be especially important for those managing certain health conditions, like those related to birth control and hypothyroidism, which can impact nutrient absorption and overall health.
Understanding how different fiber sources affect your body is crucial, and researching topics like birth control and hypothyroidism can help you make informed choices about your health. Ultimately, the best fiber alternative will depend on individual needs and preferences.
Psyllium Husk: A Soluble Fiber Champion
Psyllium husk is a highly soluble fiber source known for its ability to absorb water and form a gel-like substance in the digestive tract. This unique property aids in promoting regularity and managing digestive issues. Psyllium husk is often used as a dietary supplement to enhance fiber intake. It’s a good choice for those looking to increase their fiber consumption quickly.
The gel-like consistency of psyllium husk in the digestive tract can help to slow down the absorption of sugars, potentially helping manage blood sugar levels.
Apples: A Delicious Fiber Source, Fiber alternatives to chia seeds
Apples are a common fruit that provides a significant amount of fiber. The fiber in apples is primarily insoluble, contributing to healthy digestion and preventing constipation. Apples also contain vitamins and antioxidants, adding to their nutritional value. Eating apples as part of a balanced diet can be a convenient way to increase fiber intake. They are a readily available and delicious way to incorporate fiber into your daily routine.
Barley: A Whole Grain with Digestive Benefits
Barley, a whole grain, offers a good amount of fiber. The fiber in barley is primarily insoluble, contributing to regularity and preventing constipation. Barley also contains essential vitamins and minerals. It’s a good addition to a balanced diet and can be used in various dishes. The soluble fiber in barley can help to lower cholesterol levels, and the insoluble fiber helps with bowel movements.
Oats: A Source of Soluble Fiber
Oats are known for their high soluble fiber content, specifically beta-glucan. This type of fiber has been linked to improved blood cholesterol levels and potential benefits for heart health. Oats are a versatile grain that can be enjoyed in various ways. The soluble fiber in oats can also help to regulate blood sugar levels.
Comparison Table: Fiber Content and Nutritional Aspects
| Nutrient | Chia Seeds | Flax Seeds | Psyllium Husk | Apples | Barley | Oats |
|---|---|---|---|---|---|---|
| Fiber (grams per 100g) | 35-40 | 25-30 | >60 | 4-6 | 10-15 | 10-12 |
| Protein (grams per 100g) | 15-20 | 18-25 | ~5 | 0.3-0.5 | 10-12 | 10-12 |
| Fat (grams per 100g) | 10-15 | 40-50 | <1 | 0.2-0.4 | 1-2 | 5-7 |
| Other Notable Nutrients | Omega-3 fatty acids, antioxidants | Omega-3 fatty acids, lignans, antioxidants | High soluble fiber, potential blood sugar regulation | Vitamins, antioxidants | Vitamins, minerals, soluble fiber | Soluble fiber (beta-glucan), vitamins, minerals |
Practical Applications and Usage
Chia seeds and their fiber alternatives offer a versatile way to boost your daily fiber intake. They are incredibly adaptable to various recipes, making them a valuable addition to a healthy diet. From creamy smoothies to hearty breakfast bowls, these ingredients can be seamlessly integrated into your existing meal plans. This section delves into practical applications, exploring different preparation methods and recipe ideas to showcase the versatility of these fiber-rich options.Understanding how to incorporate chia seeds and their alternatives effectively allows for a seamless transition to a healthier lifestyle.
The key is to understand the nuances of preparation and find recipes that appeal to your taste preferences. This section will provide practical guidance on using these ingredients for diverse meals.
Incorporating Chia Seeds and Alternatives into Daily Meals
Chia seeds and their alternatives are exceptionally versatile, allowing for their incorporation into a wide range of dishes. Their ability to absorb liquid and form a gel-like consistency makes them ideal for smoothies, breakfast bowls, and even baked goods. They can also be used as a thickening agent in sauces and puddings. This adaptability makes them a valuable addition to any healthy eating plan.
Preparing Chia Seed Alternatives for Different Recipes
Different fiber alternatives require slightly different preparation methods. For example, flaxseed meal, a common alternative, can be added directly to recipes or ground into a powder. Psyllium husk powder, another alternative, needs to be mixed with water or liquid to form a gel-like consistency, similar to chia seeds. Careful attention to the specific preparation guidelines for each alternative is essential for achieving the desired results and texture in various dishes.
Recipes Incorporating Chia Seed Alternatives
Here are some recipe ideas incorporating chia seed alternatives, along with preparation methods and health benefits:
| Recipe Idea | Ingredients | Preparation Method | Health Benefits |
|---|---|---|---|
| Chia Seed Pudding | 1/4 cup chia seeds, 1 cup milk (dairy or non-dairy), 1 tbsp honey, vanilla extract | Combine all ingredients in a jar or container. Refrigerate overnight. | Excellent source of fiber, protein, and omega-3 fatty acids. |
| Breakfast Bowl with Flaxseed Meal | 1/4 cup flaxseed meal, 1 cup yogurt, berries, nuts, granola | Mix flaxseed meal into yogurt. Top with your favorite fruits and toppings. | High in fiber, omega-3 fatty acids, and antioxidants. |
| Baked Oatmeal with Psyllium Husk | 1/2 cup psyllium husk powder, 1 cup rolled oats, 1/2 cup milk, 1/4 cup fruit | Mix psyllium husk powder into the oatmeal mixture. Cook as usual. | Provides a good source of fiber, helping to regulate digestion. |
| Smoothie with Hemp Seeds | 1/4 cup hemp seeds, 1 cup frozen fruit, 1/2 cup spinach, 1/2 cup liquid | Blend all ingredients until smooth. | Excellent source of protein, fiber, and healthy fats. |
Utilizing Fiber Alternatives for a Balanced Diet
Fiber alternatives can be incorporated into a balanced diet to promote digestive health and overall well-being. By including a variety of fiber-rich foods in your meals, you can support healthy digestion, regulate blood sugar levels, and promote satiety. A balanced diet incorporating these alternatives provides a holistic approach to well-being.
Versatility of Fiber Alternatives
The following table demonstrates the versatility of various fiber alternatives in different meal types:
| Fiber Alternative | Breakfast | Lunch | Dinner |
|---|---|---|---|
| Chia Seeds | Chia seed pudding, smoothie | Salad topping, added to wraps | Thickening agent in sauces, added to oatmeal |
| Flaxseed Meal | Breakfast bowl, added to yogurt | Salad dressings, added to sandwiches | Added to soups, stews |
| Psyllium Husk Powder | Smoothies, breakfast bars | Added to salads, soups | Added to baked goods, thickening agent |
| Hemp Seeds | Breakfast bowls, smoothies | Salads, wraps, sandwiches | Added to stir-fries, salads |
Considerations and Cautions
Fiber alternatives, like many dietary changes, require careful consideration. While generally beneficial, consuming high amounts of fiber can lead to certain side effects if not approached gradually. Understanding these potential issues and the importance of a balanced approach is crucial for reaping the benefits of these alternatives without jeopardizing your health.The journey towards incorporating more fiber into your diet should be a gradual one, allowing your body to adjust and minimizing the risk of digestive discomfort.
This is especially true when introducing new fiber sources, whether they are traditional fibers or alternatives.
Potential Side Effects of Increased Fiber Intake
High fiber intake, even from healthy sources, can sometimes lead to digestive issues. Bloating and gas are common, often occurring as your body adjusts to the increased fiber content. This is a temporary response and usually subsides as your digestive system becomes accustomed to the higher fiber levels. It’s important to note that the intensity and duration of these effects can vary significantly depending on the individual and the type of fiber consumed.
Importance of Gradual Intake
Rapidly increasing fiber intake can be detrimental. It’s essential to increase fiber intake gradually, giving your digestive system time to adapt. A gradual increase, typically measured in grams per day, is recommended to avoid significant digestive discomfort. This allows the digestive system to adjust to the new fiber content, producing enzymes and gut flora to handle the increase in fiber efficiently.
This also ensures that the body can efficiently utilize the added fiber.
Fiber Supplements and Medication Interactions
Fiber supplements, like those derived from alternative sources, can interact with certain medications. These interactions can affect the absorption of the medication, potentially reducing its effectiveness or causing adverse effects. It’s crucial to consult with a healthcare professional to determine if any potential interactions exist between the fiber supplement and your current medications. This is particularly important for individuals on blood-thinning medications or those with specific health conditions.
Choosing Fiber Alternatives Based on Individual Needs
Individual needs and dietary restrictions should guide the selection of fiber alternatives. For example, someone with a known sensitivity to certain plant-based foods should be cautious when selecting fiber alternatives. If you have any underlying health conditions, it’s best to consult with a healthcare professional before adding significant amounts of fiber alternatives to your diet. This tailored approach is crucial for optimizing the health benefits while minimizing potential risks.
Recommendations for Choosing Fiber Alternatives
| Potential Side Effects | Recommendations for Usage | Interactions with Medications | Alternative Options for Specific Health Concerns |
|---|---|---|---|
| Bloating, gas, diarrhea | Start with small amounts and gradually increase intake. Drink plenty of water to aid digestion. | Check with a doctor if taking medications that affect digestion or absorption. | Consider low-FODMAP fiber options if experiencing significant digestive issues. |
| Allergic reactions | If you have known allergies, avoid fiber sources from that specific plant family. Always read labels carefully. | Always consult a doctor for any potential allergies to fiber alternatives. | Look for hypoallergenic fiber alternatives that are derived from different sources. |
| Nutrient deficiencies | Ensure the chosen fiber alternative is part of a balanced diet to avoid nutrient deficiencies. | Be cautious of supplements that may interfere with the absorption of essential nutrients. | Choose fiber alternatives that provide additional nutrients alongside fiber. |
Importance of Consulting a Healthcare Professional
Before significantly altering your diet, including the addition of fiber alternatives, it’s crucial to consult a healthcare professional. They can assess your individual needs, health conditions, and potential interactions with medications. A healthcare professional can provide personalized guidance to ensure you safely and effectively incorporate fiber alternatives into your diet. This is vital for both safety and optimal health outcomes.
Looking for fiber-rich alternatives to chia seeds? Many options exist, and understanding their potential benefits can be key. For example, flaxseeds and psyllium husk are excellent substitutes, offering similar nutritional advantages. While we’re on the topic of health, factors like a person’s overall health and the specific type of cerebral palsy can significantly impact cerebral palsy life expectancy , so it’s important to consult with a doctor.
Ultimately, finding the right fiber-rich foods to complement your diet is crucial for overall well-being.
Comparing Fiber Sources in Depth
Choosing a fiber alternative to chia seeds involves understanding the nuances of different fiber types and their effects on your body. This comparison delves into the specifics of various fiber sources, highlighting their impact on digestion, bioavailability, blood sugar management, and overall gut health. Different fibers have unique characteristics, and recognizing these distinctions is key to making informed choices.Understanding the diverse effects of different fibers is crucial for optimizing your health and dietary needs.
This analysis will explore the nuances of various fiber types, providing a comprehensive overview to help you navigate the world of fiber alternatives.
Fiber Types and Digestive Effects
Different types of dietary fiber exhibit varying effects on digestion. Soluble fiber dissolves in water, forming a gel-like substance that can slow down digestion and improve blood sugar control. Insoluble fiber, on the other hand, adds bulk to stool, promoting regularity and preventing constipation. The combination of both soluble and insoluble fiber is often ideal for optimal digestive health.
Bioavailability and Digestibility of Fiber Sources
The bioavailability and digestibility of fiber sources vary considerably. Some fibers are more easily broken down and absorbed by the body, while others may be less digestible, leading to a different impact on digestion. This difference in bioavailability can influence the overall effect of a fiber source on your body.
Impact on Blood Sugar Levels
The impact of different fiber sources on blood sugar levels is a critical consideration. Soluble fiber, in particular, is known for its ability to slow down the absorption of sugar into the bloodstream, which can help to regulate blood sugar levels and prevent spikes. This is particularly important for individuals with diabetes or those looking to manage their blood sugar.
Fiber Types and Gut Health
The different types of fiber play a significant role in supporting gut health. A balanced intake of both soluble and insoluble fiber fosters a healthy gut microbiome, which is essential for overall well-being. This includes supporting the growth of beneficial bacteria and promoting regularity.
Factors to Consider When Selecting a Fiber Alternative
Several factors should be considered when selecting a fiber alternative to chia seeds. Cost, availability, and personal preferences all play a role in your decision. Finding a source that fits within your budget and dietary needs is important. Also, consider whether the fiber is easily incorporated into your current diet and whether it complements your preferences.
Comparison Table of Fiber Sources
| Fiber Source | Fiber Type | Digestive Effects | Impact on Digestion |
|---|---|---|---|
| Chia Seeds | Soluble and Insoluble | Promotes regularity, slows digestion, improves blood sugar control | High bioavailability, good source of both types of fiber |
| Psyllium Husk | Soluble | Excellent for improving regularity, promotes satiety | High digestibility, effective for digestive health |
| Flaxseed | Soluble and Insoluble | Improves blood sugar control, promotes satiety, adds bulk to stool | Good source of omega-3 fatty acids, supports heart health |
| Oat Bran | Soluble | Lowers cholesterol, promotes satiety, improves blood sugar control | High in fiber, supports overall digestive health |
Fiber Alternatives in Specific Diets: Fiber Alternatives To Chia Seeds
Fiber alternatives offer exciting possibilities for tailoring diets to individual needs and preferences. They can be valuable additions to vegetarian, vegan, or gluten-free diets, and can also be integrated into meal plans for specific health conditions like diabetes or high cholesterol. By understanding the properties and suitability of different fiber sources, individuals can make informed choices to enhance their dietary health and well-being.
Fiber Alternatives in Vegetarian Diets
Vegetarian diets often emphasize plant-based foods, and fiber alternatives can play a significant role in supplementing dietary fiber intake. Many plant-based sources of fiber, such as psyllium husk, flaxseed meal, and guar gum, are readily available and easily incorporated into vegetarian meal plans. These alternatives can contribute to satiety, improve digestion, and support overall health. For example, adding psyllium husk to smoothies or using flaxseed meal as a topping for salads can be convenient ways to increase fiber intake without significantly altering existing recipes.
Fiber Alternatives in Vegan Diets
Vegan diets, which exclude all animal products, also benefit from fiber alternatives. These alternatives can help maintain digestive health and support a healthy gut microbiome. Many vegan recipes already incorporate legumes, fruits, and vegetables that are naturally high in fiber. However, fiber alternatives like glucomannan or konjac flour can further enhance the fiber content of vegan meals.
For instance, using glucomannan as a thickener in soups or stews can create a satisfying and nutritious dish while increasing fiber intake.
Fiber Alternatives in Gluten-Free Diets
Gluten-free diets require careful consideration of ingredients to avoid gluten-containing products. Many fiber alternatives are naturally gluten-free, making them suitable for this dietary approach. Options such as chia seeds, flaxseed meal, and psyllium husk are commonly used in gluten-free baking and cooking. For example, flaxseed meal can replace some of the flour in gluten-free bread recipes, enhancing the texture and nutritional value.
Carefully checking labels is crucial to ensure that any processed fiber alternative is indeed gluten-free.
Fiber Alternatives for Diabetes Management
Individuals with diabetes often need to closely monitor their carbohydrate intake. Certain fiber alternatives, particularly those with a low glycemic index, can be beneficial. Psyllium husk and glucomannan are often recommended for their ability to slow down the absorption of sugar, which can help manage blood sugar levels. Incorporating these fiber alternatives into meals, such as using them as a thickener in soups or adding them to smoothies, can be a practical way to manage blood sugar control.
Fiber Alternatives for High Cholesterol
Fiber alternatives can play a significant role in managing high cholesterol levels. Soluble fibers, like those found in psyllium husk and flaxseed, can help lower LDL (“bad”) cholesterol. This can be achieved by incorporating these alternatives into various dishes. For instance, using psyllium husk as a replacement for traditional thickeners can enhance the nutritional value of meals.
Comparing Fiber Alternatives for Different Diets
| Fiber Alternative | Vegetarian | Vegan | Gluten-Free | Pros/Cons |
|---|---|---|---|---|
| Psyllium Husk | Yes | Yes | Yes | High in soluble fiber, aids digestion, helps manage blood sugar; can have a slightly gritty texture. |
| Flaxseed Meal | Yes | Yes | Yes | Excellent source of omega-3 fatty acids and fiber; adds a nutty flavor to dishes. |
| Glucomannan | Yes | Yes | Yes | Forms a gel-like consistency, increasing satiety; can have a subtle flavor. |
| Chia Seeds | Yes | Yes | Yes | Versatile addition to various dishes; high in omega-3 fatty acids and fiber. |
Epilogue
In conclusion, fiber alternatives to chia seeds provide a spectrum of options for enriching your diet. From the familiar to the less common, each alternative offers unique nutritional benefits and culinary applications. Understanding their individual properties, and how to integrate them into your meals, is key to unlocking a healthier, more balanced lifestyle. Remember to consult a healthcare professional before making significant dietary changes.