What is a bone scan for cancer? This scan is a powerful tool for detecting cancer spread, offering crucial insights into the presence and extent of the disease. It’s a non-invasive procedure using radioactive tracers to pinpoint areas of bone activity. Understanding how these scans work and how they help diagnose cancer is essential for anyone facing this health challenge.
This detailed look explores the science behind bone scans and their critical role in cancer diagnosis, from preparation to interpretation and beyond.
This comprehensive guide delves into the mechanics of bone scans, explaining how they identify cancer metastasis and the specific physiological changes in bone that cancer cells cause. The process, from initial preparation to interpreting results, is thoroughly examined, with attention to the potential limitations and considerations for accurate diagnosis. We will also look at how a bone scan compares to other imaging techniques.
Introduction to Bone Scans
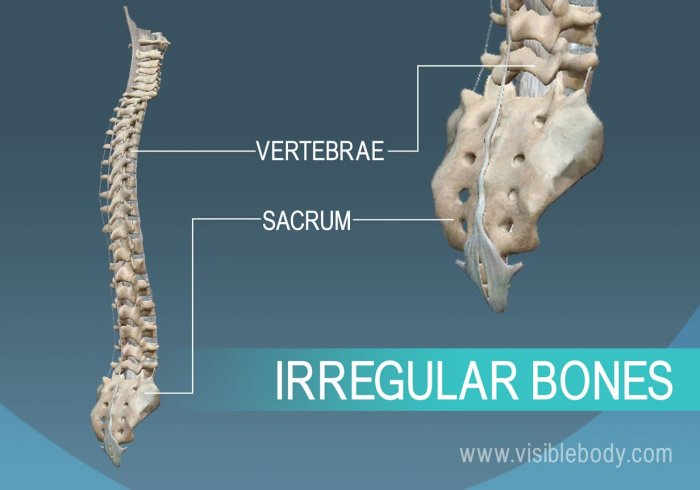
A bone scan, also known as a skeletal scintigraphy, is a specialized imaging technique that helps visualize the bones in the body. It’s a valuable tool for detecting various conditions, but it plays a crucial role in identifying possible cancer spread to the bones. This procedure uses a small amount of radioactive material, called a tracer, which is absorbed by the bones.
The tracer’s uptake is then detected by a special camera, allowing doctors to pinpoint areas of increased or decreased activity.Bone scans are particularly useful in cancer diagnosis and treatment monitoring. They can help determine if cancer has spread from its primary site to the bones (metastasis). By pinpointing areas of increased bone activity, a bone scan can reveal suspicious areas that may need further investigation, potentially leading to early detection and intervention.
This early detection is often crucial in improving treatment outcomes.
Bone Scan Imaging Techniques
The fundamental principle behind bone scans lies in the use of radioactive tracers. These tracers, usually a form of technetium-99m, are injected into the bloodstream. The tracers are preferentially absorbed by bone tissue, especially in areas of high metabolic activity, like damaged or cancerous regions. A specialized gamma camera detects the emitted radiation from the tracer, producing images of the skeletal system.
These images allow medical professionals to identify areas with abnormal uptake of the tracer, which can be indicative of various conditions, including cancer metastasis. Different types of bone scans use various techniques to capture and process the emitted radiation, ultimately providing different levels of detail and resolution.
Types of Bone Scans
Understanding the different types of bone scans is essential to comprehend their specific applications and limitations. Each type provides unique insights into bone health.
| Scan Type | Purpose | Procedure | Advantages/Disadvantages |
|---|---|---|---|
| Planar Bone Scan | Provides a general overview of bone activity. | A single camera image is taken from a fixed angle. | Simple, quick, and relatively inexpensive. However, it might not show small areas of abnormality and may have lower resolution than more advanced techniques. |
| SPECT (Single Photon Emission Computed Tomography) Bone Scan | Provides 3D images of bone activity, revealing subtle abnormalities more effectively than planar scans. | Multiple images are taken from various angles, then processed to create a 3D representation. | Provides detailed 3D images and can detect subtle abnormalities. However, it is more complex, time-consuming, and more expensive than planar scans. |
Cancer Detection with Bone Scans
Bone scans are valuable tools in the detection and monitoring of cancer, particularly when the cancer has spread to the bones. Understanding how these scans work, and the specific characteristics of cancerous bone lesions, is crucial for accurate diagnosis and effective treatment planning. This section delves into the mechanisms by which bone scans identify cancer metastasis and the imaging features that differentiate them from other bone conditions.Bone scans, utilizing radioactive tracers, pinpoint areas of increased bone activity.
This heightened activity is often a telltale sign of cancer spreading to the bone. Cancer cells, when they metastasize to the bone, stimulate a complex cascade of physiological responses in the surrounding bone tissue. These responses lead to increased bone turnover, characterized by an imbalance between bone formation and resorption.
Mechanisms of Cancer Spread to Bone
Cancer cells, during metastasis, can directly invade bone tissue or travel through the bloodstream to reach the bone. Once there, they stimulate osteoclasts, cells responsible for breaking down bone, to become more active. This accelerated bone resorption creates an environment where new bone is laid down more rapidly, often in an abnormal and disorganized pattern. The abnormal remodeling process is evident as focal areas of increased bone activity, which bone scans detect.
Imaging Characteristics of Bone Lesions
The imaging characteristics of bone lesions associated with cancer vary depending on the specific type of cancer and the stage of bone involvement. Bone scans typically reveal focal areas of increased uptake of the radioactive tracer. These areas, called “hot spots,” are often irregular in shape and size. The intensity of the “hot spot” reflects the degree of bone turnover stimulated by the cancer cells.
In some cases, the lesions might appear as “cold spots,” areas of decreased tracer uptake, due to the absence of cellular activity or an accumulation of fibrous tissue.
Comparison with Other Imaging Techniques
Bone scans complement other imaging techniques like X-rays and CT scans in assessing bone health. X-rays are useful for detecting gross bone abnormalities, fractures, and bone deformities. CT scans provide detailed cross-sectional images, offering a wider view of the affected area, and can highlight soft tissue abnormalities. However, bone scans excel at identifying subtle changes in bone metabolism associated with cancer spread, which X-rays and CT scans might miss.
This sensitivity to subtle metabolic changes makes bone scans particularly valuable for detecting early signs of metastasis, even before visible structural changes are evident.
Table: Bone Cancer Detection with Bone Scans
| Cancer Type | Symptoms | Imaging Findings | Bone Scan Role |
|---|---|---|---|
| Multiple Myeloma | Bone pain, fractures, anemia, recurrent infections | Lytic lesions (areas of bone destruction), increased bone density in some areas | Identifies widespread bone involvement, assesses extent of disease |
| Breast Cancer | Pain, swelling, palpable lump in breast, often accompanied by fatigue and weight loss | Focal areas of increased uptake in bone | Detects distant spread to bone, aids in staging and monitoring |
| Prostate Cancer | Frequent urination, pain in lower back, hips, or pelvis, and difficulty urinating | Focal areas of increased uptake in bone, possible osteolytic or sclerotic lesions | Assesses spread to bone, assesses disease extent and response to treatment |
| Lung Cancer | Persistent cough, shortness of breath, chest pain, fatigue, and weight loss | Focal areas of increased uptake in bone | Detects distant spread to bone, aids in staging and monitoring |
Preparing for a Bone Scan
Getting ready for a bone scan involves careful preparation to ensure accurate results. Understanding the necessary steps can ease anxiety and help you feel more prepared for the procedure. Proper preparation minimizes potential interference with the scan’s interpretation and ensures a smooth experience.
Dietary Restrictions
Dietary restrictions play a crucial role in obtaining clear and accurate bone scan results. Certain foods and beverages can affect the uptake of the radioactive tracer used in the scan. These restrictions typically begin a few days before the procedure. Specific instructions will vary depending on the facility and the reason for the scan, but commonly, patients are advised to avoid foods high in calcium and iron.
- Foods high in calcium, like dairy products, may interfere with the tracer’s absorption, potentially leading to inaccurate results.
- Iron-rich foods, such as red meat and spinach, can also affect the scan’s accuracy.
- The specific dietary guidelines will be provided by the medical facility performing the scan.
Medications
Certain medications can influence the outcome of a bone scan. Patients should inform their doctor about all medications they are taking, including over-the-counter drugs, supplements, and herbal remedies. This is vital to assess if any adjustments are needed or if there are medications that should be temporarily stopped.
- Inform your doctor about all medications, including prescription, over-the-counter, and herbal remedies.
- Some medications may affect the tracer’s uptake or interfere with the scan’s interpretation. Adjustments may be necessary, or temporary cessation might be required.
- Follow the specific instructions provided by the medical facility regarding medication intake before the scan.
Other Considerations
Other factors beyond diet and medications can affect the outcome of a bone scan. Patient activity levels, hydration, and the time of day the scan is performed can all contribute to the accuracy of the results.
- Patient activity levels may influence the results, so discuss any recent strenuous exercise with your doctor.
- Hydration levels can impact the scan’s accuracy. Follow instructions on hydration before the scan.
- The time of day for the scan can sometimes be a factor. Discuss this with the facility performing the scan.
- Jewelry and metal objects should be removed prior to the scan, as they may interfere with the images.
Common Questions
Patients often have questions about preparing for a bone scan. These concerns are addressed to provide clarity and alleviate any anxiety.
- Patients may inquire about the specific dietary restrictions required before the scan.
- Concerns regarding medications and their impact on the scan’s outcome are also common.
- Questions about the timing of the scan and any additional instructions are frequently asked.
- Understanding the potential factors that could affect the results helps patients feel more informed and prepared.
Factors Affecting Interpretation
Several factors can influence the interpretation of a bone scan. These include underlying medical conditions, the presence of previous fractures or surgeries, and the individual’s bone density. These factors are essential for a proper evaluation of the results.
A bone scan for cancer helps doctors see if cancer has spread to the bones. It’s a useful diagnostic tool, but it’s important to remember that understanding how medications like Cialis work, this is how cialis works , is a completely different medical area. Ultimately, a bone scan is just one piece of the puzzle in figuring out a cancer diagnosis and treatment plan.
- Underlying medical conditions, such as arthritis or osteoporosis, can affect bone scan results.
- Previous fractures or surgeries may show up as areas of increased uptake on the scan, potentially leading to misinterpretations.
- Bone density variations across different individuals can affect the scan’s interpretation.
- The radiologist interpreting the scan will consider these factors and provide an accurate assessment.
Comparison of Preparations by Age Group
| Age Group | Diet | Medications | Special Instructions | Additional Considerations |
|---|---|---|---|---|
| Adults | Avoid high calcium and iron foods | Inform doctor about all medications | Remove jewelry and metal objects | Discuss recent activity levels |
| Children | Follow specific pediatric guidelines | Inform doctor about all medications | Possible need for sedation or parental assistance | Consider developmental stages and behaviors |
| Elderly | Follow specific guidelines for elderly patients | Inform doctor about all medications, including over-the-counter and supplements | May need assistance with preparation | Consider potential cognitive impairment and mobility issues |
Interpreting Bone Scan Results
Understanding a bone scan’s results involves more than just looking at images. It requires a meticulous analysis by a radiologist, considering various factors to determine if the findings are related to cancer or other conditions. The radiologist carefully examines the images and creates a comprehensive report, detailing the location, size, and characteristics of any suspicious areas. This report is crucial for the patient’s overall diagnosis and treatment plan.
Bone Scan Image Presentation, What is a bone scan for cancer
Bone scan results are presented primarily through images and reports. The images, often acquired using specialized cameras, display areas of increased uptake of the radioactive tracer. These areas appear as “hot spots” on the scan. The intensity and location of these hot spots are crucial in determining the significance of the findings. A detailed report accompanying the images further clarifies the interpretation.
Radiologist Interpretation of Bone Scan Images
Radiologists employ a multifaceted approach in interpreting bone scan images. They examine the distribution, intensity, and size of the “hot spots” to identify potential abnormalities. This involves comparing the findings to normal bone patterns and considering the patient’s medical history, symptoms, and other imaging results. The radiologist’s experience and knowledge are essential for accurate interpretation, especially when distinguishing between benign and malignant conditions.
A bone scan for cancer helps doctors pinpoint suspicious areas in your bones that might indicate the presence of cancer cells. Understanding the specifics of different types of cancer, like insulinoma, is also important. For a deeper dive into insulinoma, check out this comprehensive overview insulinoma overview and more. Ultimately, a bone scan is a crucial diagnostic tool in the fight against cancer, helping to identify and manage potential skeletal involvement.
Common Cancer-Associated Findings on Bone Scans
Common findings on bone scans associated with cancer include localized “hot spots” indicating increased bone activity. These hot spots might be present in areas known to be affected by cancer or in regions not commonly associated with cancer, necessitating further investigation. Examples of common locations include the spine, pelvis, and ribs. The presence of multiple “hot spots” or widespread areas of increased activity could also suggest metastatic disease.
Factors Affecting Bone Scan Results
False-positive or false-negative results can occur due to various factors. For example, inflammation, infection, or benign bone conditions can mimic the appearance of cancerous lesions, leading to a false-positive result. Conversely, a lack of uptake in areas affected by cancer can sometimes lead to a false-negative result, particularly if the disease is in an early stage or involves minimal bone involvement.
It is crucial to consider these possibilities when evaluating the findings.
Information in a Bone Scan Report
A bone scan report typically contains specific information about the location, size, and characteristics of any detected lesions. The report will describe the exact location of the abnormal areas, their size, and the degree of uptake. It may also note the presence of any other associated findings, such as the presence of pain or other symptoms.
Table: Bone Lesion Characteristics and Potential Associations
| Lesion Characteristic | Description | Potential Cancer Association | Other Possible Causes |
|---|---|---|---|
| Focal Increased Uptake | A concentrated area of increased radioactivity | Possible metastasis, primary bone cancer | Inflammation, infection, trauma, benign tumors |
| Diffuse Increased Uptake | Increased uptake spread over a large area | Possible widespread metastasis, certain types of bone cancer | Metabolic bone disease, Paget’s disease |
| Moth-eaten Appearance | Lesion with irregular borders | Suggests aggressive cancer | Certain types of bone tumors |
| Permeative Lesion | Lesion that penetrates the bone structure | Aggressive cancer or severe infection | Bone infections, certain types of bone tumors |
Limitations and Considerations

Bone scans, while valuable tools, are not without limitations. Their accuracy and effectiveness depend on various factors, and understanding these limitations is crucial for accurate interpretation and appropriate patient management. A thorough evaluation often requires combining bone scan results with other diagnostic methods for a comprehensive picture of the patient’s condition.Interpreting a bone scan in isolation can lead to misdiagnosis or missed diagnoses.
Clinicians need to consider other factors like the patient’s medical history, symptoms, and the results of other tests, alongside the bone scan. A comprehensive approach is essential to ensure the most accurate assessment.
Limitations of Bone Scans in Cancer Diagnosis
Bone scans are excellent for detecting bone involvement by cancer, but they are not perfect. They can be less sensitive in identifying early-stage cancers or cancers that haven’t spread to the bones. Sometimes, a bone scan might show abnormal activity that isn’t necessarily cancerous. This can be due to other conditions like arthritis or inflammation. Moreover, bone scans don’t always pinpoint the exact location of the primary tumor.
A bone scan for cancer helps doctors pinpoint suspicious areas in your bones, potentially revealing signs of cancer spread. While discussing medical imaging, it’s important to remember that preventative health measures like getting the moderna covid 19 vaccine are crucial. Ultimately, a bone scan can be a valuable tool for diagnosing and monitoring various bone-related conditions, ensuring you get the best possible care.
They primarily indicate the presence and extent of bone metastases, not the origin of the cancer.
Situations Where Bone Scans Might Not Be the Best Diagnostic Tool
Bone scans are not always the optimal diagnostic tool. Their effectiveness is limited when the cancer hasn’t spread to the bones or when the bone involvement is minimal. For example, early-stage cancers may not yet have reached the stage where bone metastases are detectable. In such cases, other imaging techniques might be more suitable. Similarly, if the primary concern is the location and characteristics of the primary tumor, a bone scan might not provide the necessary information.
Alternative and Supplementary Diagnostic Methods
Various alternative and supplementary imaging methods are available to provide a more complete picture of the disease. These include X-rays, CT scans, MRI scans, and PET scans. Each method has its strengths and weaknesses. For instance, CT scans can reveal details about bone structure, while MRI scans provide superior soft tissue imaging. PET scans are particularly useful in detecting metabolic activity, which can be helpful in distinguishing between benign and malignant processes.
Importance of Considering Other Factors
A comprehensive diagnostic approach requires considering factors beyond the bone scan results. A patient’s medical history, symptoms, and the results of other tests, such as blood tests, are crucial. For example, a patient with a history of back pain and a positive bone scan result might need further investigation to rule out other potential causes, like a herniated disc.
A thorough evaluation, combining different data points, leads to a more accurate and informed diagnosis.
Comparison of Imaging Methods for Cancer Detection
| Cancer Type | Bone Scan | Alternative Imaging | Advantages/Disadvantages |
|---|---|---|---|
| Breast Cancer | Can detect bone metastases | Mammogram, Ultrasound, MRI | Bone scan: Useful for advanced stages, less sensitive for early detection. Alternatives: Detect primary tumor and early stages more effectively, better for soft tissue imaging. |
| Lung Cancer | Can detect bone metastases | CT scan, PET scan, X-ray | Bone scan: Less detailed than CT or PET, not as effective for primary tumor location. Alternatives: CT and PET are superior for lung cancer diagnosis and staging, detecting early signs and spreading. |
| Prostate Cancer | Can detect bone metastases, often used to assess extent of disease | PSA blood test, MRI | Bone scan: Identifies bone involvement, helps stage the disease. Alternatives: PSA is a useful marker for prostate cancer, MRI provides detailed imaging of the prostate gland. |
Illustrative Cases
Bone scans play a crucial role in diagnosing and managing cancer, particularly when it has spread to the bones. Understanding how these scans are used in real-world scenarios is essential for comprehending their diagnostic value. The following cases illustrate both positive and negative outcomes of bone scan utilization.
A Case of Metastatic Cancer
A 65-year-old female patient presented with persistent back pain, fatigue, and unexplained weight loss. The pain had worsened over several weeks, radiating to her hips and legs. Physical examination revealed tenderness in the lumbar spine and hips. Initial blood tests and X-rays showed no apparent abnormalities. Given the patient’s symptoms and the possibility of metastatic cancer, a bone scan was ordered.The bone scan revealed multiple areas of increased uptake in the spine, pelvis, and ribs.
These areas corresponded with the patient’s reported pain locations. The increased uptake suggested the presence of bone lesions, potentially indicative of metastatic disease. Further investigation, including a biopsy of a suspicious lesion in the spine, confirmed the diagnosis of breast cancer that had metastasized to the bone. The patient was then referred for chemotherapy and radiation therapy, aiming to manage the cancer and alleviate her pain.
A Case Ruling Out Cancer
A 42-year-old male presented with mild hip pain after a recent fall. The pain was localized to the hip joint and wasn’t accompanied by other symptoms. He denied any previous medical history of cancer or significant trauma. Given the possibility of a fracture or other condition, a bone scan was performed.The bone scan showed no evidence of abnormal bone uptake in the hip or any other area.
There were no signs of bone lesions or fractures. The results were consistent with a normal bone structure and metabolism. The patient was diagnosed with a simple hip contusion related to the fall, and the bone scan effectively ruled out the possibility of cancer metastasis.
Diagnostic Workflow Table
| Step | Description | Imaging Findings | Potential Diagnosis |
|---|---|---|---|
| 1. Patient Presentation | Patient presents with symptoms like bone pain, fatigue, unexplained weight loss, or history of cancer. | None yet, symptoms noted | Suspected metastatic cancer, other bone conditions |
| 2. Initial Assessment | Initial physical examination and blood tests are performed. X-rays might be conducted to rule out other conditions | Normal X-rays, or abnormal X-rays suggestive of fracture or bone disease | Fracture, other bone condition, non-cancerous lesions |
| 3. Bone Scan Ordering | Based on the initial assessment and patient’s history, a bone scan is ordered. | Increased uptake in specific bones, or normal bone uptake. | Metastatic cancer, infection, or other bone pathology, normal bone condition |
| 4. Bone Scan Interpretation | Radiologist analyzes the bone scan images to determine areas of abnormal uptake or lack thereof. | Specific areas of increased or decreased uptake visualized on bone scan. | Metastatic cancer, infection, or other bone pathology, normal bone condition, stress fracture, or other bone issues. |
| 5. Further Investigation | If the bone scan suggests a possible malignancy, further tests like biopsy are performed. | Biopsy results confirm or rule out the presence of cancer cells. | Cancer, or other pathology |
| 6. Final Diagnosis | The combination of the bone scan results, clinical presentation, and results of further investigations lead to a final diagnosis. | Images and results of other tests | Final diagnosis, either cancer or no cancer. |
Final Review: What Is A Bone Scan For Cancer
In conclusion, a bone scan is a valuable diagnostic tool for cancer detection and staging, offering crucial information about the extent of the disease. While it’s not a perfect method, its insights, when combined with other diagnostic tools, provide a more complete picture of a patient’s condition. Understanding the preparation, interpretation, and limitations of this procedure is vital for both patients and healthcare professionals.
We’ve explored the mechanics, potential pitfalls, and complementary methods for a holistic understanding of bone scans in the context of cancer detection.