Vitamin a everything you need to know – Vitamin A: Everything You Need to Know delves into the fascinating world of this essential nutrient. From its crucial role in vision and immune function to its impact on skin health and pregnancy, we’ll explore every aspect of this vital vitamin. Understanding the various forms of Vitamin A, its sources, and potential deficiencies is key to maximizing its benefits and avoiding potential risks.
This comprehensive guide will equip you with the knowledge to make informed decisions about your health.
This in-depth look at Vitamin A explores the diverse functions of this important nutrient, covering everything from the chemical structures of retinol, retinal, and retinoic acid, to the foods that provide it and the risks of deficiency or toxicity. We’ll also analyze the specific roles of Vitamin A in pregnancy, vision, immune function, and skin health. By understanding the science behind Vitamin A, you can optimize your health and well-being.
Introduction to Vitamin A

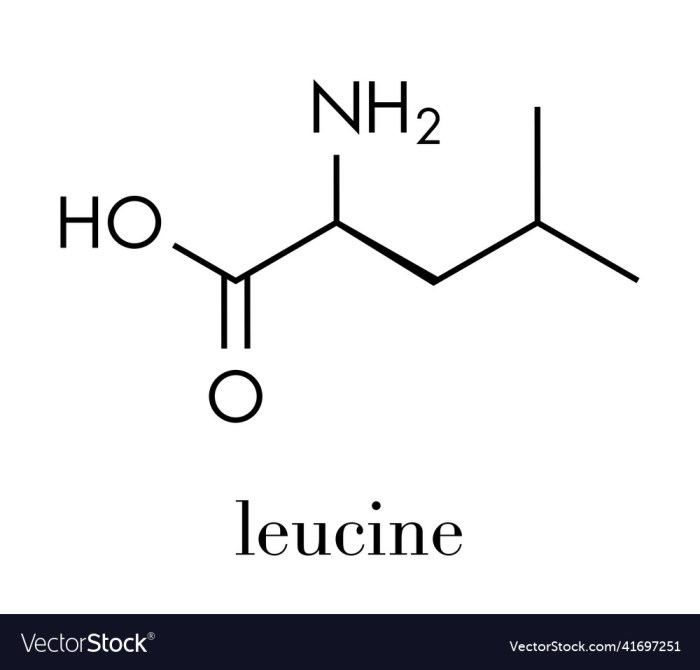
Vitamin A is a crucial fat-soluble vitamin essential for a wide range of bodily functions. It plays a vital role in maintaining healthy vision, supporting a robust immune system, and promoting cell growth and development. Understanding the different forms of Vitamin A and their specific functions is key to appreciating its importance in overall health.The various forms of Vitamin A, including retinol, retinal, and retinoic acid, each have unique roles in the body.
These different forms are crucial for various processes, from vision to immune response, highlighting the complexity and importance of this nutrient.
Different Forms of Vitamin A
Vitamin A exists in several forms, each with a distinct role. These forms are readily convertible into one another, allowing the body to utilize the different forms efficiently. Retinol, retinal, and retinoic acid are the key forms, each with specialized functions.
Roles of Vitamin A in the Body
Vitamin A is a cornerstone of maintaining good vision. It’s essential for the production of rhodopsin, a light-sensitive pigment in the retina, enabling us to see in dim light. Beyond vision, Vitamin A plays a critical role in supporting a healthy immune system. It helps maintain the integrity of mucous membranes, acting as a first line of defense against infection.
Additionally, Vitamin A is vital for cell growth and development, crucial for the maintenance and repair of tissues throughout the body.
Functions of Vitamin A
- Vision: Vitamin A is essential for the production of rhodopsin, the light-sensitive pigment in the retina. This pigment is crucial for low-light vision and overall visual acuity. Deficiencies can lead to night blindness and eventually, more severe vision problems.
- Immune Function: Vitamin A supports a healthy immune system by maintaining the integrity of mucous membranes, which act as a barrier against pathogens. Adequate Vitamin A intake is crucial for preventing infections and supporting the body’s natural defenses.
- Cell Growth and Development: Vitamin A plays a vital role in the growth and development of cells throughout the body. It’s involved in processes such as cell differentiation, reproduction, and repair, ensuring the healthy functioning of various tissues and organs.
Vitamin A Forms, Sources, and Functions
| Form | Sources | Primary Functions |
|---|---|---|
| Retinol | Liver, egg yolks, dairy products, fatty fish | Essential for cell growth and development; crucial for maintaining healthy skin and mucous membranes. |
| Retinal | Carotenoids in fruits and vegetables (e.g., carrots, sweet potatoes, spinach) | Crucial for vision, particularly night vision; also involved in cell differentiation and immune function. |
| Retinoic Acid | Converted from retinol and retinal in the body; also available in some supplements | Plays a key role in cell growth and differentiation; important for regulating gene expression. |
Vitamin A deficiency can lead to various health issues, including impaired vision, weakened immune function, and problems with growth and development.
Sources of Vitamin A: Vitamin A Everything You Need To Know
Vitamin A, a crucial nutrient for vision, immune function, and cell growth, is available in a wide array of foods. Understanding the different sources and their bioavailability is key to ensuring adequate intake. This section explores the diverse food sources of Vitamin A, highlighting the importance of a balanced diet.
Animal Sources of Vitamin A
Animal products are excellent sources of preformed vitamin A, also known as retinol. This form is readily absorbed by the body. Liver, particularly beef and chicken liver, is exceptionally rich in retinol. Other excellent sources include fatty fish like salmon and tuna, and dairy products like milk and cheese. The fat content in these foods plays a significant role in the absorption of vitamin A.
- Liver: Beef and chicken liver are particularly rich in vitamin A. Liver contains a high concentration of retinol, making it a potent source of this essential nutrient. The vitamin A content varies depending on the specific animal and preparation method. Consumption of liver should be moderate due to potential for other nutrients like iron.
- Fatty Fish: Salmon, tuna, and mackerel are excellent sources of vitamin A, particularly in the form of retinyl esters. The fat content in these fish helps with absorption. The specific vitamin A content varies depending on the fish species and its diet.
- Dairy Products: Milk, cheese, and butter contain vitamin A, although the amounts may vary. The vitamin A content in dairy products is often fortified to enhance its nutritional value.
Plant Sources of Vitamin A
Plant foods contain provitamin A carotenoids, which the body converts into retinol. This conversion process isn’t always efficient, so the bioavailability of vitamin A from plant sources is generally lower than from animal sources. However, a varied diet rich in colorful fruits and vegetables provides a significant contribution to overall vitamin A intake.
- Dark Leafy Greens: Spinach, kale, and collard greens are excellent sources of carotenoids, particularly beta-carotene. These greens also provide other essential nutrients, making them a valuable addition to a balanced diet.
- Orange and Yellow Fruits and Vegetables: Carrots, sweet potatoes, pumpkins, and mangoes are rich in beta-carotene. The vibrant colors of these foods indicate a high concentration of carotenoids. The conversion rate of beta-carotene to retinol varies by individual and factors such as overall diet and health.
- Other Fruits and Vegetables: Broccoli, cantaloupe, and apricots also contribute to vitamin A intake. The specific carotenoid composition and the conversion rate to retinol vary across these and other plant-based foods.
Bioavailability of Vitamin A
The bioavailability of vitamin A, meaning how effectively the body absorbs and utilizes it, varies significantly between sources. Preformed vitamin A from animal products is generally more readily absorbed than provitamin A carotenoids from plant foods. Factors such as the presence of fat in the diet, the presence of other nutrients in the food, and overall health can influence bioavailability.
Importance of Dietary Diversity
Consuming a wide variety of vitamin A-rich foods is essential for optimal health. A diverse diet ensures a greater intake of both preformed vitamin A and carotenoids, leading to a more reliable supply of this vital nutrient. This diversity also provides the body with a broader range of beneficial nutrients and antioxidants. Furthermore, varying sources offer diverse nutritional benefits.
For instance, the carotenoids in plant foods also act as antioxidants, contributing to overall health.
Comparison of Vitamin A Content in Fruits and Vegetables
| Food | Vitamin A (mcg) | Vitamin C (mg) | Fiber (g) |
|---|---|---|---|
| Carrots (cooked, 1 medium) | 420 | 5 | 2.6 |
| Spinach (cooked, 1 cup) | 585 | 18 | 2.4 |
| Sweet Potatoes (baked, 1 medium) | 450 | 8 | 4.1 |
| Mango (1 medium) | 20 | 62 | 1.1 |
| Cantaloupe (1 cup) | 80 | 28 | 1.3 |
Note: Values may vary depending on the specific food and preparation method.
Vitamin A Deficiency
Vitamin A, a crucial nutrient for vision and immune function, is essential for overall health. Unfortunately, a significant portion of the global population faces a deficiency, leading to a range of adverse health consequences. Understanding the symptoms, prevalence, and long-term effects of vitamin A deficiency is vital for preventive measures and effective interventions.
Symptoms and Consequences of Deficiency
Vitamin A deficiency manifests in various ways, impacting primarily vision and immune function. Early signs can be subtle, but if left unaddressed, they can progress to severe complications. A deficiency weakens the body’s ability to fight off infections, increasing susceptibility to diseases. This compromised immune response is particularly detrimental in children, as it can hinder their growth and development.
Impact on Vision
A deficiency in vitamin A significantly affects the health of the eyes. The most well-known consequence is night blindness, where individuals struggle to see in low-light conditions. Prolonged deficiency can lead to more severe eye problems, including xerophthalmia, a condition characterized by dryness of the eyes. This dryness can progress to corneal damage and, ultimately, blindness if left untreated.
This highlights the critical role vitamin A plays in maintaining healthy vision.
Impact on Immune Function
Vitamin A plays a crucial role in the development and function of the immune system. A deficiency diminishes the body’s ability to mount an effective immune response against pathogens. This impaired immunity makes individuals more susceptible to infections, increasing the risk of developing severe illnesses, particularly in children. The reduced immune response can manifest as increased susceptibility to respiratory infections, diarrhea, and other common ailments.
Prevalence of Vitamin A Deficiency
Globally, vitamin A deficiency remains a significant public health concern, particularly in developing countries. Malnourished children and pregnant women are at higher risk of experiencing this deficiency. Regions with limited access to a balanced diet rich in vitamin A-containing foods are disproportionately affected. For example, populations in certain parts of sub-Saharan Africa and Southeast Asia frequently face vitamin A deficiency due to dietary limitations.
Long-Term Health Effects of Chronic Deficiency
Chronic vitamin A deficiency can have severe long-term health consequences. The impaired immune system makes individuals more vulnerable to infections, leading to increased morbidity and mortality. Moreover, the ongoing damage to the eyes can result in permanent vision impairment or blindness. In children, chronic deficiency can hinder growth and development, leading to long-term physical and cognitive deficits.
Summary of Signs and Symptoms
| Sign/Symptom | Severity | Description |
|---|---|---|
| Night blindness | Mild | Difficulty seeing in low-light conditions. |
| Xerophthalmia (dry eyes) | Moderate | Dryness and inflammation of the eyes, potentially leading to corneal damage. |
| Increased susceptibility to infections | Moderate to Severe | Weakened immune response, making individuals more vulnerable to various diseases. |
| Corneal ulceration | Severe | Open sores on the cornea, often accompanied by pain and inflammation. |
| Blindness | Severe | Permanent vision loss due to severe corneal damage. |
Vitamin A Toxicity
Vitamin A, while crucial for vision and overall health, can become harmful if consumed in excessive amounts. Understanding the risks associated with vitamin A toxicity is essential for maintaining a balanced diet and preventing potential health issues. This section will delve into the potential dangers of exceeding recommended daily allowances, outlining the symptoms and conditions that can arise.
Potential Risks of Excessive Vitamin A Intake
Excessive vitamin A intake can lead to a range of adverse health effects. High levels of preformed vitamin A (retinol) are particularly concerning, as the body doesn’t readily excrete it. This accumulation can result in a condition known as hypervitaminosis A. The toxicity can manifest in various ways, impacting different bodily systems.
So, diving into vitamin A – everything you need to know is a fascinating journey. It’s crucial for healthy vision, skin, and immune function. Learning how to properly remove a tick, however, is equally important for your well-being. If you’re bitten by a tick, following these steps for proper tick removal is key to preventing potential health issues.
Knowing how to remove a tick how to remove a tick is a valuable skill, but understanding vitamin A’s vital role in the body remains paramount. Ultimately, both topics contribute to a healthier you.
Symptoms of Vitamin A Toxicity
Vitamin A toxicity presents with a variety of symptoms, ranging from mild discomfort to severe complications. Early signs might include headaches, dizziness, and nausea. Prolonged or excessive intake can lead to more severe symptoms, such as bone pain, blurred vision, and liver damage. In severe cases, hypervitaminosis A can even prove fatal.
Conditions Leading to Vitamin A Toxicity
Vitamin A toxicity is primarily caused by consuming excessive amounts of preformed vitamin A from supplements or fortified foods. A diet heavily reliant on liver or certain fish oil supplements can also contribute. Individuals with underlying liver conditions may be particularly susceptible to the negative effects of high vitamin A intake. In some instances, genetic factors may play a role in how the body processes vitamin A, making certain individuals more prone to toxicity.
Recommended Daily Allowance (RDA) of Vitamin A
The recommended daily allowance of vitamin A varies depending on age and gender. A balanced diet, including fruits, vegetables, and fortified foods, should provide the necessary amount. Dietary sources of vitamin A are typically well-tolerated, while excessive amounts from supplements can pose significant risks. Calculating the appropriate RDA is crucial for avoiding both deficiency and toxicity.
| Age Group | Gender | RDA (mcg RAE) |
|---|---|---|
| 0-6 months | Male/Female | 400 |
| 7-12 months | Male/Female | 500 |
| 1-3 years | Male/Female | 300 |
| 4-8 years | Male/Female | 400 |
| 9-13 years | Male | 600 |
| 9-13 years | Female | 500 |
| 14-18 years | Male | 900 |
| 14-18 years | Female | 700 |
| 19+ years | Male | 900 |
| 19+ years | Female | 700 |
Note: RDA values are approximations and may vary slightly based on individual needs. Consult a healthcare professional for personalized recommendations.
Maintaining a Balanced Diet
A balanced diet is essential for ensuring adequate vitamin A intake without exceeding the recommended daily allowance. Focus on consuming a variety of fruits, vegetables, and whole grains. These natural sources of vitamin A provide the body with essential nutrients alongside the vitamin, supporting overall health and preventing toxicity. It’s important to avoid relying solely on supplements or fortified foods for vitamin A, as these can easily lead to exceeding the recommended daily intake.
Moderation is key when incorporating vitamin A-rich foods into your diet.
Vitamin A and Health Conditions
Vitamin A plays a crucial role in maintaining overall health, impacting numerous bodily functions. Beyond its well-known importance for vision, it’s a vital component for healthy skin, immune function, and reproduction. Understanding its influence on various health conditions is essential for optimal well-being. This section delves into the multifaceted relationship between vitamin A and specific health concerns, examining both benefits and potential risks.Vitamin A’s diverse impact extends far beyond its role in vision.
It acts as a powerful antioxidant, protecting cells from damage and contributing to healthy skin. Furthermore, its influence on the immune system and reproductive functions highlights its significance in maintaining overall health. This section explores the complexities of vitamin A’s involvement in these areas, including the specific mechanisms through which it contributes to positive outcomes and the potential risks of supplementation.
Vitamin A and Acne
Vitamin A derivatives, such as retinoids, are commonly used topically to treat acne. These compounds help regulate sebum production, reduce inflammation, and promote cell turnover, leading to a reduction in acne lesions. However, topical retinoids can sometimes cause skin irritation, dryness, and sensitivity, especially in the beginning. The efficacy and optimal dosage vary significantly depending on individual responses and the severity of acne.
Diving into vitamin A’s benefits is fascinating, but it’s crucial to remember that while a healthy diet is essential, especially when facing a condition like living with metastatic breast cancer , it’s vital to consult with healthcare professionals. Understanding the specific needs of your body and how vitamin A interacts with other treatments is key to a well-rounded approach to your health.
Further research into vitamin A’s role in overall health and well-being is definitely worthwhile.
Vitamin A and Skin Health
Vitamin A is essential for maintaining healthy skin. It promotes collagen production, crucial for skin elasticity and firmness. Furthermore, it supports cell turnover, contributing to a youthful complexion. Vitamin A derivatives, in both oral and topical forms, can stimulate collagen synthesis and enhance skin barrier function. Proper skin hydration and gentle exfoliation are often recommended in conjunction with vitamin A treatments to maximize benefits and minimize potential side effects.
Vitamin A and Reproductive Health
Vitamin A is essential for normal reproductive function in both males and females. It plays a role in sperm production and maturation in males, and in maintaining healthy reproductive tissues in females. Adequate vitamin A intake is critical during pregnancy to support fetal development. However, excessive intake can pose risks during pregnancy. Consult with a healthcare professional for guidance on appropriate vitamin A intake during pregnancy and other stages of reproductive health.
Potential Interactions with Other Nutrients and Medications
Vitamin A can interact with other nutrients and medications. For instance, high doses of vitamin A can interfere with the absorption of vitamin K, potentially leading to bleeding disorders. Some medications, such as certain antibiotics and corticosteroids, may also influence vitamin A metabolism. Careful monitoring and consultation with a healthcare professional are essential when taking vitamin A supplements or medications.
Dietary sources of vitamin A pose less risk of these interactions, but still should be considered in relation to the broader dietary context.
Table of Vitamin A Health Benefits
| Health Benefit | Mechanism | Examples |
|---|---|---|
| Acne Treatment | Regulates sebum production, reduces inflammation, promotes cell turnover | Topical retinoids |
| Skin Health Maintenance | Promotes collagen production, supports cell turnover, enhances skin barrier function | Topical retinoids, oral vitamin A |
| Reproductive Health Support | Essential for sperm production, supports healthy reproductive tissues | Critical during pregnancy and other reproductive stages |
Vitamin A and Pregnancy

Vitamin A plays a crucial role in both maternal and fetal health, particularly during pregnancy and breastfeeding. Adequate intake is essential for the development of various organs and tissues in the growing fetus, while also supporting the mother’s overall well-being. Understanding the importance of vitamin A during these critical periods is paramount for ensuring healthy outcomes.
Importance of Vitamin A During Pregnancy
Vitamin A is vital for cell growth and differentiation, impacting multiple systems during pregnancy. It’s essential for the formation of the embryo’s tissues and organs, including the eyes, lungs, and heart. Adequate intake during early pregnancy is especially critical for the proper development of the neural tube, a structure that forms the brain and spinal cord.
Potential Risks of Insufficient Vitamin A Intake
Insufficient vitamin A intake during pregnancy can lead to various complications. It can increase the risk of spontaneous abortions, low birth weight, and birth defects. Women with insufficient vitamin A reserves may also experience a compromised immune system, making them more susceptible to infections during pregnancy.
Potential Risks of Excessive Vitamin A Intake
While crucial for development, excessive vitamin A intake during pregnancy can be harmful. High doses of preformed vitamin A (retinol) can lead to fetal abnormalities, including birth defects. It’s important to adhere to recommended dietary allowances and avoid supplements containing high amounts of preformed vitamin A without consulting a healthcare professional.
Vitamin A and Maternal Health
Vitamin A supports various aspects of maternal health during pregnancy. It contributes to maintaining healthy mucous membranes, which are vital for preventing infections. Adequate vitamin A levels can also help in the production of breast milk and support the immune system during this crucial period.
Recommended Daily Allowances for Pregnant and Breastfeeding Women
| Category | Recommended Daily Allowance (RAE) |
|---|---|
| Pregnant Women (19-50 years) | 770 mcg RAE |
| Lactating Women (19-50 years) | 1300 mcg RAE |
| Note: | RAE stands for Retinol Activity Equivalent. This unit accounts for the different forms of vitamin A and their relative biological activity. |
These values are approximate and may vary based on individual needs and specific circumstances. It is always advisable to consult a healthcare professional for personalized recommendations.
Vitamin A Supplements
Taking vitamin A supplements can be a helpful strategy for individuals who have difficulty meeting their daily needs through diet alone. However, like any supplement, it’s crucial to understand the potential benefits, drawbacks, and the importance of professional guidance. Unregulated intake can lead to adverse effects, making informed decisions vital.Vitamin A supplements come in various forms, each with unique characteristics.
Understanding these differences is essential for selecting the appropriate supplement and ensuring safe and effective use. It’s not a one-size-fits-all solution, and individual needs vary greatly. Consulting a healthcare professional is paramount to determine the best course of action.
Vitamin A Supplement Types and Formulations, Vitamin a everything you need to know
Different forms of vitamin A supplements cater to diverse needs and preferences. Understanding these formulations is crucial for selecting the right one. Vitamin A exists in two primary forms: retinol (preformed vitamin A) and carotenoids (provitamin A).
- Retinol supplements are readily absorbed by the body. They are often found in concentrated forms, providing a high dose of vitamin A. However, excessive intake of retinol can lead to toxicity, highlighting the importance of appropriate dosage and professional guidance.
- Carotenoid supplements, such as beta-carotene, are converted into retinol in the body. This conversion process is not always efficient, and the body may not utilize all the ingested carotenoids. The advantage lies in a potential lower risk of toxicity compared to preformed vitamin A.
Importance of Professional Consultation
Before starting any vitamin A supplementation regimen, consulting a healthcare professional is paramount. This consultation allows for a personalized assessment of individual needs, existing health conditions, and potential interactions with other medications.A healthcare provider can accurately assess if a vitamin A supplement is necessary and recommend the appropriate dosage and type. They can also monitor for potential side effects and adjust the regimen as needed.
Self-treating with vitamin A supplements without professional guidance can lead to unwanted consequences.
Potential Benefits and Drawbacks
Vitamin A supplements can offer various benefits, such as supporting vision health, immune function, and cell growth. However, excessive intake can lead to significant drawbacks, including liver damage, birth defects (especially during pregnancy), and other health issues.
- Potential Benefits: Vitamin A supplements can be beneficial for individuals with a diagnosed deficiency or those with specific dietary restrictions that hinder vitamin A intake. Proper intake can enhance immune function and support eye health.
- Potential Drawbacks: Excessive intake can lead to a range of adverse effects, including nausea, vomiting, headaches, and even more serious conditions like liver damage and birth defects. These risks highlight the critical need for professional guidance.
Comparison of Vitamin A Supplement Brands
| Brand | Supplement Type | Ingredients | Dosage (mg) | Potential Side Effects |
|---|---|---|---|---|
| Brand A | Retinol | Retinyl Palmitate | 5000 | Headache, nausea, dry skin |
| Brand B | Beta-carotene | Beta-carotene | 10,000 | Orange-tinged skin, diarrhea |
| Brand C | Retinol + Vitamin E | Retinyl Palmitate, Vitamin E | 2500 | Dry skin, hair loss |
Note: This table is for illustrative purposes only and does not represent an exhaustive list. Always consult a healthcare professional before starting any supplement regimen. Dosage and potential side effects can vary significantly based on individual factors and specific product formulations.
Vitamin A and Vision
Vitamin A plays a crucial role in maintaining healthy vision, supporting a wide range of functions from basic light perception to detailed image processing. Its importance in eye health extends beyond just visual acuity; it’s fundamental for the structure and function of the entire eye. Understanding the specific mechanisms of Vitamin A in vision is key to appreciating its impact on overall eye health.Vitamin A, in its active form retinol, is a vital component of rhodopsin, a light-sensitive pigment in the retina.
Rhodopsin’s role is to convert light signals into electrical signals that the brain interprets as images. Adequate Vitamin A levels are essential for the production and maintenance of rhodopsin, enabling the eye to function optimally in low-light conditions. Furthermore, Vitamin A is also crucial for maintaining the integrity of the cornea, the transparent outer layer of the eye, protecting it from damage and ensuring clear vision.
The Role of Vitamin A in Rhodopsin Production
Vitamin A is directly involved in the synthesis of rhodopsin, the light-sensitive pigment within the retina’s rod cells. These cells are responsible for vision in dim light. Rhodopsin’s structure relies on the presence of retinal, a derivative of Vitamin A. When light strikes the retina, retinal changes shape, triggering a cascade of events that ultimately lead to a nerve signal being sent to the brain, allowing us to see.
Vitamin A is crucial for a ton of bodily functions, from vision to immune support. But did you know that proper thyroid function plays a vital role in absorbing and utilizing vitamin A? If your thyroid isn’t functioning optimally, it can impact how well your body processes vitamin A. This is why understanding what happens when you don’t take your thyroid medication is so important.
What happens when you don’t take your thyroid meds can significantly affect your overall health, potentially impacting vitamin A levels. Ultimately, ensuring your thyroid is healthy is key for optimal vitamin A absorption and overall wellness.
Without sufficient Vitamin A, rhodopsin production is compromised, leading to problems with night vision.
Vitamin A Deficiency and Eye Health Issues
Vitamin A deficiency can lead to a spectrum of eye health problems, with night blindness being a prominent early symptom. This occurs because insufficient Vitamin A prevents the proper regeneration of rhodopsin, making it harder to see in low light conditions. Prolonged deficiency can further progress to xerophthalmia, a condition characterized by dryness of the conjunctiva and cornea.
This dryness can lead to corneal damage, ulcers, and even blindness if left untreated.
Impact of Vitamin A on Various Eye Conditions
| Eye Condition | Potential Impact of Vitamin A Deficiency | Potential Impact of Adequate Vitamin A Intake |
|---|---|---|
| Night Blindness | A significant symptom of Vitamin A deficiency, resulting from impaired rhodopsin production. | Adequate Vitamin A intake supports the production of rhodopsin, improving night vision. |
| Xerophthalmia | Prolonged Vitamin A deficiency can lead to dryness of the conjunctiva and cornea, potentially causing corneal damage and ulcers. | Adequate Vitamin A intake helps maintain the moisture and health of the eye’s surface tissues, preventing xerophthalmia. |
| Corneal Ulcers | Dryness and damage to the cornea, often a consequence of Vitamin A deficiency, can increase the risk of corneal ulcers. | Sufficient Vitamin A helps maintain the integrity of the cornea, reducing the risk of ulcers. |
| Cataracts | While the direct link to Vitamin A deficiency isn’t always clear, maintaining optimal nutritional status, including Vitamin A, is important for overall eye health. | Adequate Vitamin A intake is a part of a comprehensive approach to eye health and may contribute to reduced risk of certain eye conditions. |
Vitamin A and Immune Function
Vitamin A plays a crucial role in maintaining a robust immune system, impacting various aspects of its function. Its influence extends from the production of immune cells to the regulation of their activity. This vital nutrient is essential for a healthy response to infections and overall well-being.Vitamin A’s impact on immune function stems from its involvement in the development and maturation of immune cells, primarily lymphocytes.
These cells are the body’s frontline defense against pathogens. Vitamin A also supports the proper functioning of the mucous membranes, forming a crucial barrier against infection.
Mechanisms of Vitamin A’s Immunomodulatory Effects
Vitamin A influences immune responses through several mechanisms. It affects the development and differentiation of T cells, a crucial type of lymphocyte. Vitamin A also enhances the production of antibodies, which neutralize pathogens and help the body clear infections. Further, Vitamin A helps regulate the inflammatory response, preventing excessive inflammation that can damage healthy tissues. Its presence is essential for the proper function of phagocytes, cells that engulf and destroy pathogens.
Impact of Vitamin A Deficiency on Immunity
Vitamin A deficiency significantly weakens the immune system’s ability to fight infections. Individuals with low vitamin A levels are more susceptible to respiratory infections, diarrhea, and other illnesses. This is because a lack of vitamin A impairs the development and function of immune cells, reducing the body’s capacity to effectively combat pathogens. The impaired mucosal barrier function also contributes to increased infection risk.
Improving Vitamin A Intake for Enhanced Immune Response
A balanced diet rich in vitamin A-rich foods is key to supporting a strong immune system. The following table Artikels various sources and their respective vitamin A content. Remember, vitamin A can be obtained in both preformed (retinol) and provitamin (carotenoid) forms. Carotenoids, like beta-carotene, are converted into retinol in the body.
| Food Source | Vitamin A Content (approximate) | Notes |
|---|---|---|
| Liver (beef, pork, chicken) | High | Excellent source of preformed vitamin A, but consume in moderation due to potential for other nutrients. |
| Fish (salmon, tuna) | Moderate | Good source of vitamin A and other essential nutrients. |
| Eggs | Moderate | A good source of vitamin A and other essential nutrients. |
| Dairy products (milk, yogurt, cheese) | Moderate | Good source of vitamin A, especially in fortified versions. |
| Dark leafy greens (spinach, kale) | Moderate (as carotenoids) | Excellent source of carotenoids, which the body converts to vitamin A. |
| Orange and yellow fruits and vegetables (carrots, sweet potatoes, mangoes) | Moderate (as carotenoids) | Rich in carotenoids, essential for vitamin A production. |
| Fortified foods (cereals, milk) | Variable | Check labels for vitamin A content. |
Vitamin A plays a vital role in supporting a strong immune system, contributing to the body’s defense against infections. Consuming a variety of vitamin A-rich foods is crucial for optimal immune function.
Vitamin A and Skin Health
Vitamin A plays a crucial role in maintaining healthy skin. It’s essential for various functions, from promoting cell turnover to bolstering the skin’s protective barrier. This intricate relationship between vitamin A and skin health extends to the treatment of various skin conditions, making it a valuable component in dermatological care.Vitamin A, in its active forms, influences skin cell proliferation and differentiation, crucial processes in skin regeneration.
This impact on cell turnover ensures the skin maintains its youthful appearance and protective functions. The modulation of inflammation is another key mechanism by which vitamin A impacts skin health, contributing to the overall well-being and appearance of the skin.
Mechanisms of Vitamin A’s Impact on Skin
Vitamin A’s influence on skin health stems from its impact on cell proliferation and differentiation. Retinoids, a form of vitamin A, promote the production of new skin cells, replacing damaged or old ones. This process, known as cell turnover, helps maintain the skin’s texture, resilience, and ability to repair itself. The active forms of vitamin A, particularly retinoids, stimulate the production of collagen, a crucial protein that supports skin elasticity and structure.
This contributes to a smoother, firmer, and more youthful complexion.
Vitamin A in Acne Treatment
Vitamin A derivatives, like retinoids, are frequently used to treat acne. They work by reducing inflammation, unclogging pores, and regulating sebum production. By exfoliating the skin, retinoids help remove dead skin cells that can contribute to clogged pores. This exfoliation also helps prevent the formation of comedones, which are the small bumps that characterize acne. Retinoids have proven effective in treating various acne types, from mild to severe cases.
Vitamin A and Other Skin Conditions
Vitamin A, in various forms, shows promise in treating several skin conditions. Its ability to modulate inflammation and stimulate skin regeneration makes it a valuable tool in dermatological treatments.
| Skin Condition | Potential Vitamin A Use |
|---|---|
| Acne | Retinoids are commonly prescribed to reduce inflammation, regulate sebum production, and exfoliate the skin. |
| Wrinkles and Fine Lines | Retinoids can stimulate collagen production, leading to firmer, smoother skin and a reduction in the appearance of wrinkles and fine lines. |
| Psoriasis | Some studies suggest vitamin A derivatives can help manage psoriasis symptoms by reducing inflammation and promoting skin cell turnover. |
| Eczema | Vitamin A may help alleviate some eczema symptoms by reducing inflammation and improving skin barrier function. |
| Sun Damage | Topical retinoids can help reduce the appearance of sun spots, wrinkles, and other signs of sun damage. |
Safety Considerations
While vitamin A is generally safe, it’s important to use it cautiously, particularly when used topically. Sensitivity to retinoids can manifest as dryness, redness, or peeling. It’s crucial to start with a low concentration and gradually increase the dosage as tolerated. Consulting a dermatologist is always recommended, especially when treating specific skin conditions.
Final Wrap-Up
In conclusion, Vitamin A plays a multifaceted role in overall health. From bolstering your immune system to supporting healthy vision and skin, its importance cannot be overstated. Understanding the different forms, sources, and potential risks associated with this vitamin is crucial for making informed dietary choices. By incorporating Vitamin A-rich foods into your diet and understanding its crucial functions, you can support your body’s optimal functioning.
This guide provides a solid foundation for understanding this vital nutrient and how it impacts your well-being.