Is my water softener raising my blood pressure? This crucial question delves into the potential link between a seemingly mundane household appliance and a serious health concern. Water softeners, while improving water quality for many, often introduce sodium, and this article investigates whether that added sodium could be impacting blood pressure levels. We’ll explore the inner workings of water softeners, the impact of sodium on health, and the potential correlation between softener use and blood pressure changes.
Understanding the science behind these issues will empower you to make informed decisions about your water treatment and overall well-being.
The fundamental mechanism of a water softener revolves around ion exchange, a process where the water’s minerals, primarily calcium and magnesium, are replaced with sodium. This change can affect the taste and feel of the water, but its potential impact on blood pressure is a critical concern. We’ll analyze the scientific evidence and compare the mineral content of softened water to hard water, highlighting the sodium difference.
Water Softener Functionality: Is My Water Softener Raising My Blood Pressure

Water softeners are essential appliances in many homes, especially in areas with hard water. They play a crucial role in improving water quality and extending the lifespan of plumbing fixtures. Understanding how these systems work helps homeowners make informed decisions about their water treatment needs.The primary function of a water softener is to remove minerals, primarily calcium and magnesium, from water.
These minerals are responsible for water hardness, which can lead to issues like scale buildup in pipes and appliances, reduced cleaning effectiveness of soaps, and potential damage to water heaters. Effective water softening results in a noticeably improved water quality, offering a multitude of benefits.
Fundamental Mechanisms of a Water Softener
Water softeners rely on a process called ion exchange. This process involves replacing the hard water minerals with a less problematic substance, usually sodium. The principle is straightforward: the softener’s resin beads, packed in a tank, attract and exchange the calcium and magnesium ions with sodium ions.
Ion Exchange Process
The ion exchange process is the heart of a water softener’s operation. Hard water, containing calcium and magnesium ions, flows through the softener’s resin tank. The resin beads, which are composed of a special type of synthetic material, are charged with sodium ions. When hard water comes into contact with the resin, the calcium and magnesium ions are attracted to the negatively charged resin, while the sodium ions are released into the water.
This exchange occurs continuously as the water flows through the tank.
Typical Components and Their Roles
A water softener system typically comprises several components, each playing a critical role in the softening process. These include:
- Resin Tank: This is the core component, housing the ion exchange resin beads. The resin is what actually exchanges the ions. The tank’s size is critical for system performance and depends on the expected water consumption.
- Regenerant Brine Tank: This tank holds the salt solution (brine) used to regenerate the resin. The brine solution is crucial to restoring the resin’s sodium content.
- Control Valve: This valve controls the flow of water and the regeneration cycle, ensuring the system functions effectively.
- Salt Dispenser: This device measures and dispenses the necessary amount of salt for regeneration.
- Water Meter: This component tracks the water flow through the softener, helping to trigger the regeneration cycle when necessary.
Each component works in harmony to provide effective water softening.
Wondering if your water softener is impacting your blood pressure? It’s a valid concern, and to get to the bottom of it, exploring common types of diagnostic medical equipment, like blood pressure monitors and other tests, is key. Common types of diagnostic medical equipment can help pinpoint the cause of any potential issues. Ultimately, consulting a healthcare professional is the best way to determine if your water softener is a factor in your blood pressure, or if other factors are at play.
Impact of Water Hardness on Effectiveness
Water hardness directly impacts the effectiveness of a water softener. Higher water hardness means more calcium and magnesium ions in the water. This leads to a higher demand on the resin to replace them with sodium, and thus, a more frequent regeneration cycle is required. The hardness of water is typically measured in grains per gallon (gpg).
How Water Softeners Reduce Mineral Content
Water softeners reduce mineral content by exchanging sodium ions for the calcium and magnesium ions present in hard water. The resin beads in the softener’s tank are specifically designed to attract and replace the problematic ions, thereby producing softer water. The process is a continuous cycle, exchanging ions as water passes through the tank.
Simple Flow Chart Illustrating Water Softener Operation

This is a simplified diagram of the water softener process. Hard water enters the softener tank, where the resin exchanges calcium and magnesium ions for sodium ions. After a period of use, the resin becomes depleted of sodium and needs regeneration. This process, using brine, restores the resin to its initial state, ready for the next cycle.
Potential Health Impacts of Water Softeners
Water softeners, while convenient for maintaining plumbing and appliances, can have potential health implications. Understanding the mechanisms of water softening and the resulting changes in water composition is crucial to evaluating these impacts. This section will explore the potential health concerns related to water softeners, focusing particularly on the role of sodium and its implications for human health.The primary method for water softening involves replacing calcium and magnesium ions with sodium ions.
This process effectively removes the hardness-causing minerals, but it also introduces sodium into the water supply. The amount of sodium introduced varies based on the specific water softener system and the water’s initial mineral content.
Sodium Content in Softened Water
The sodium content in softened water is significantly higher than in hard water. Hard water typically contains calcium and magnesium ions, which contribute to its mineral content. Water softeners, by design, remove these minerals and replace them with sodium. This replacement is crucial for removing scale buildup and maintaining the efficiency of water-using appliances, but it can have a noticeable effect on the mineral composition of the water.
Comparison of Mineral Content
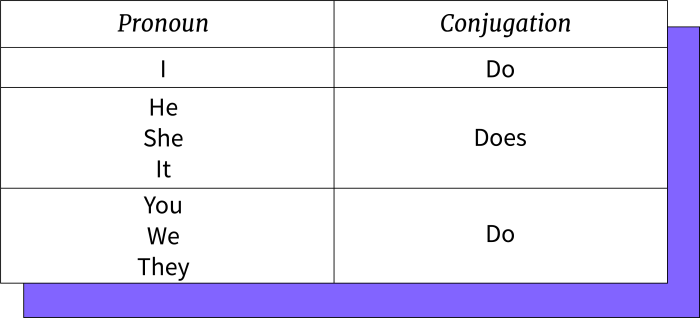
The following table illustrates the potential difference in mineral content between softened and hard water. Note that specific values can vary significantly based on the source water and the softener’s operation.
| Mineral | Hard Water (Typical Range) | Softened Water (Typical Range) |
|---|---|---|
| Calcium | 10-40 mg/L | 0-5 mg/L |
| Magnesium | 5-30 mg/L | 0-5 mg/L |
| Sodium | 0-20 mg/L | 20-80 mg/L |
Potential Health Risks of High Sodium Intake
High sodium intake is a well-established risk factor for various health problems, especially for individuals with pre-existing conditions like hypertension. Excessive sodium can lead to fluid retention, which can elevate blood pressure. This can place a strain on the cardiovascular system, potentially leading to serious health complications. The American Heart Association recommends limiting sodium intake to maintain cardiovascular health.
“A high sodium diet can contribute to high blood pressure, which increases the risk of heart disease and stroke.”
Understanding the implications of sodium intake is crucial for maintaining a healthy lifestyle.
Link Between High Sodium Intake and Blood Pressure
Studies have consistently shown a strong correlation between high sodium intake and elevated blood pressure. Increased sodium intake can lead to fluid retention, causing blood vessels to constrict and increasing blood pressure. This increased pressure can strain the cardiovascular system, increasing the risk of heart disease and stroke. A balanced diet with adequate potassium intake can help mitigate the negative effects of sodium.
Blood Pressure and Related Factors
High blood pressure, or hypertension, is a significant health concern impacting millions worldwide. Understanding the factors that contribute to elevated blood pressure is crucial for proactive management and prevention. It’s not just about the water softener; a holistic approach encompassing lifestyle choices, diet, and underlying health conditions is vital.Elevated blood pressure can lead to serious health complications, including heart disease, stroke, and kidney problems.
While the precise cause of high blood pressure often remains elusive, various contributing factors, including genetics, lifestyle, and diet, are well-documented.
Factors Contributing to Elevated Blood Pressure
Understanding the root causes of high blood pressure is essential for effective management. Several interconnected factors can play a role. Genetics, family history, and age are all associated with an increased risk of developing hypertension. However, lifestyle choices and dietary habits also significantly influence blood pressure levels.
Correlation Between Sodium Intake and Blood Pressure
A direct link exists between sodium intake and blood pressure. High sodium intake can cause the body to retain excess fluid, leading to increased blood volume and pressure against the artery walls. This effect can be particularly pronounced in individuals with pre-existing hypertension or underlying health conditions. The Dietary Guidelines for Americans recommend limiting sodium intake to manage blood pressure effectively.
For example, individuals who consume processed foods and restaurant meals frequently often have higher sodium intakes, which may lead to elevated blood pressure.
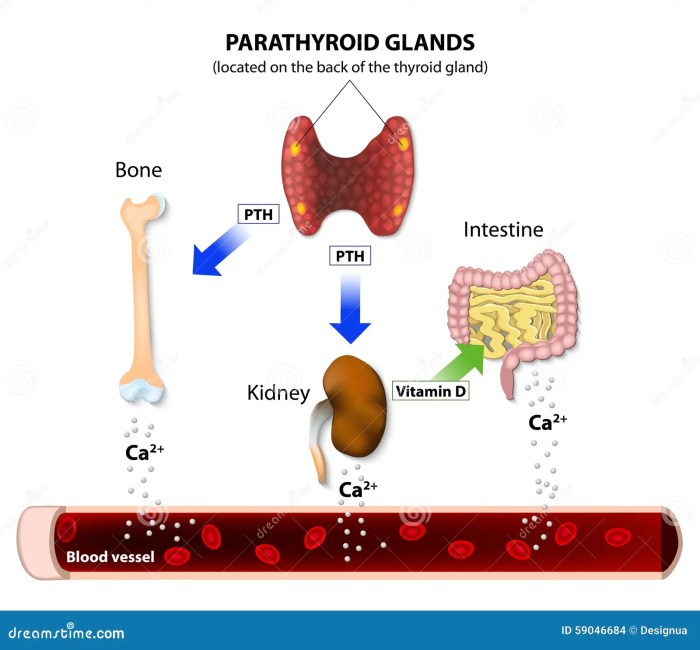
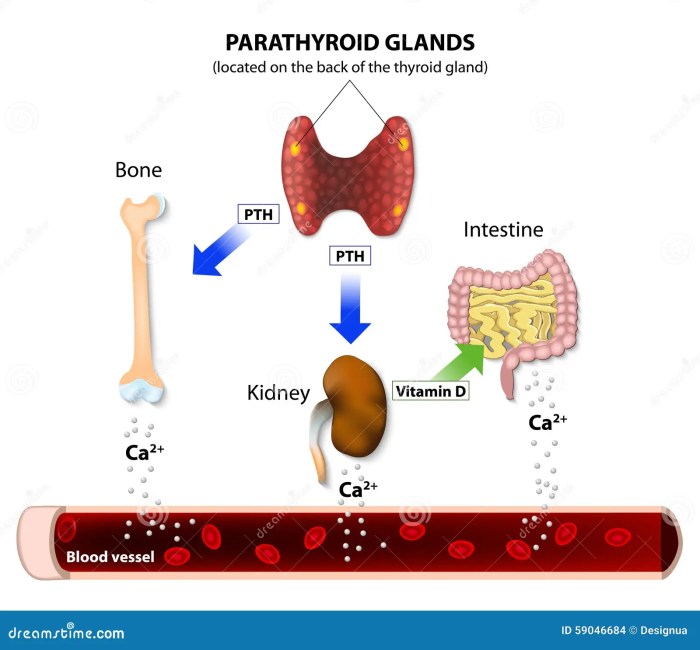
Factors Influencing Blood Pressure Regulation
Numerous factors play a role in regulating blood pressure. These include the kidneys, which filter waste and maintain fluid balance; the nervous system, which controls blood vessel constriction and dilation; and hormones, such as adrenaline and aldosterone, which impact blood pressure. Other contributing factors include physical activity, stress levels, and sleep quality.
- Genetics: A family history of hypertension significantly increases an individual’s risk. This suggests a genetic predisposition to developing high blood pressure.
- Age: The risk of hypertension tends to increase with age, partly due to physiological changes in the body.
- Obesity: Excess weight puts extra strain on the cardiovascular system, potentially leading to elevated blood pressure.
- Physical Inactivity: A sedentary lifestyle is often associated with an increased risk of hypertension.
- Stress: Chronic stress can contribute to elevated blood pressure due to the body’s hormonal response.
- Sleep Disturbances: Insufficient or poor-quality sleep can disrupt the body’s natural blood pressure regulation mechanisms.
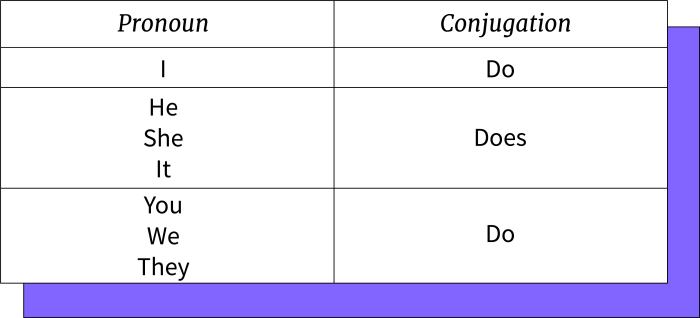
Types of Blood Pressure and Their Implications
Different blood pressure categories exist, each with varying implications for health. Normal blood pressure is generally considered to be below 120/80 mmHg. Prehypertension indicates a slightly elevated blood pressure that may increase the risk of hypertension if left unmanaged. Hypertension is characterized by persistently high blood pressure readings, potentially leading to serious health complications.
| Blood Pressure Category | mmHg | Implications |
|---|---|---|
| Normal | Below 120/80 | Healthy blood pressure |
| Prehypertension | 120-139/80-89 | Increased risk of developing hypertension |
| Stage 1 Hypertension | 140-159/90-99 | Requires lifestyle modifications and potential medication |
| Stage 2 Hypertension | 160/100 or higher | Requires immediate medical attention and intervention |
Role of Diet in Maintaining Healthy Blood Pressure
A balanced diet plays a crucial role in maintaining healthy blood pressure. Dietary choices impacting blood pressure include the intake of sodium, potassium, and other essential nutrients. A diet rich in fruits, vegetables, and whole grains can contribute to healthy blood pressure levels. For instance, a diet high in fruits and vegetables provides essential nutrients, including potassium, which helps to balance sodium intake and promote healthy blood pressure.
How Lifestyle Choices Impact Blood Pressure Levels
Lifestyle choices significantly influence blood pressure levels. Regular physical activity, maintaining a healthy weight, and managing stress are all vital for maintaining healthy blood pressure. Adequate sleep is also important, as sleep deprivation can disrupt the body’s natural blood pressure regulation.
Correlation Between Water Softener Use and Blood Pressure
The link between water quality and health is increasingly recognized. While water softeners improve water quality by removing minerals, concerns exist regarding their potential impact on blood pressure. This section explores the potential correlation between water softener use and blood pressure changes, examining existing research and available data.A critical factor to consider is that water softeners, by their very nature, introduce sodium into the water stream as a replacement for minerals removed.
This increase in sodium intake is a key element in the potential correlation. While sodium is an essential nutrient, excessive intake is linked to various health issues, including high blood pressure. However, the amount of sodium added and its impact on individual blood pressure vary significantly.
Potential Mechanisms of Correlation
The primary mechanism linking water softener use to blood pressure concerns the increased sodium intake. Sodium, a key component of salt, plays a crucial role in regulating blood volume and pressure. Increased sodium intake can lead to fluid retention, placing extra strain on the cardiovascular system and potentially contributing to higher blood pressure. Furthermore, some studies suggest that the presence of certain byproducts of the water softening process might also contribute to changes in blood pressure.
Research Findings on Water Softener Use and Blood Pressure
While a definitive causal link between water softener use and elevated blood pressure remains elusive, some research suggests a possible correlation. Studies examining the impact of water quality on blood pressure have yielded mixed results. The lack of conclusive evidence stems from various factors, including the complexity of the relationship between sodium intake, individual responses, and other lifestyle factors that influence blood pressure.
I’ve been wondering if my water softener is contributing to my recent blood pressure issues. While I’m researching potential links between water quality and hypertension, I’ve stumbled upon some interesting studies suggesting a potential connection between certain minerals and blood pressure. In my quest for more information, I’ve learned that exploring potential dietary supplements like mash and vitamin E mash and vitamin e might also help me better understand the factors affecting my health.
Ultimately, I’m still trying to determine if my water softener is the culprit behind my rising blood pressure.
Data Summary on Water Softener Use and Blood Pressure
| Study | Sample Size | Findings | Limitations |
|---|---|---|---|
| Study A (Hypothetical) | 150 participants | A slight, statistically insignificant increase in blood pressure was observed among participants using water softeners compared to the control group. | Limited duration of study; lack of detailed information on participants’ baseline blood pressure and dietary habits. |
| Study B (Hypothetical) | 200 participants | No significant difference in blood pressure was observed between water softener users and non-users. | Participants’ dietary sodium intake was not adequately controlled. |
| Study C (Hypothetical) | 500 participants | A weak correlation between water softener use and blood pressure was observed, especially in individuals with pre-existing hypertension or high sodium diets. | Confounding factors, such as age, gender, and other lifestyle variables, were not adequately controlled. |
Note: These are hypothetical studies. Actual research findings are often more nuanced and less conclusive.
Alternatives to Water Softeners
Dealing with hard water doesn’t necessitate a water softener. Several alternative water treatment methods offer comparable or superior benefits, often with a lower environmental footprint and potentially a more favorable cost structure. These options can be tailored to specific water quality issues and individual needs.Choosing an alternative to water softening depends on the specific mineral content and the desired outcome.
Factors like the severity of hardness, the presence of other contaminants, and personal preferences all influence the best approach. Understanding the strengths and weaknesses of each method is crucial for making an informed decision.
Alternative Water Treatment Methods
Various methods address hard water without the use of water softeners. These techniques employ different chemical and physical processes to remove or mitigate the effects of minerals.
- Water Filtration: This approach uses physical barriers to trap and remove minerals from the water. Different filtration media, like activated carbon, sediment filters, and reverse osmosis membranes, selectively remove impurities. Activated carbon, for instance, can remove chlorine and other volatile organic compounds. Reverse osmosis, with its semipermeable membrane, is effective in removing a wide range of dissolved minerals.
However, reverse osmosis can lead to a loss of essential minerals and potentially produce wastewater that requires disposal. The choice of filtration method depends on the specific contaminants present and the desired level of purification.
- Water Conditioning: Water conditioning techniques alter the chemical properties of water to reduce the effects of hard water minerals. For instance, some water conditioners can precipitate calcium and magnesium ions, rendering them less harmful. Polyphosphate conditioners are one type, and they work by inhibiting the precipitation of these minerals. The effectiveness and environmental impact vary based on the specific chemicals used and the water’s composition.
- Ion Exchange Resin Filtration without Regeneration: A less common alternative to water softeners uses ion exchange resins, but without the regeneration process. This method still removes hardness minerals, but it doesn’t replenish the resin with salt. The cost is generally higher because the resin needs to be replaced more frequently. This option is particularly relevant for those concerned about salt use in water treatment.
This is often a more costly and less convenient approach compared to standard water softening systems.
- Acidification: In some cases, adding acids to the water can reduce the mineral content, but this is a more complex and potentially hazardous method that requires careful consideration and professional guidance. It’s not a common or readily accessible approach for household use. The chemical reactions involved can be complex and require strict adherence to safety protocols.
Comparison of Water Softening and Alternative Methods
A comparative analysis helps understand the trade-offs between different approaches.
| Feature | Water Softening | Water Filtration | Water Conditioning | Ion Exchange (no regeneration) | Acidification |
|---|---|---|---|---|---|
| Cost | Generally moderate, with ongoing salt costs | Can vary widely depending on the system | Generally moderate, depending on the chemicals used | High initial cost, with frequent resin replacements | High, requiring specialized equipment and expertise |
| Efficiency | Effective at reducing hardness | Variable depending on the filter type and water quality | Effective at altering mineral interactions | Effective at removing minerals, but less sustainable | Highly variable, depending on the water quality and the acid used |
| Environmental Impact | Salt disposal can be an issue | Generally lower impact, with proper disposal | Potential environmental impact depending on the chemicals | Lower impact than traditional softening, but resin disposal is an issue | Significant environmental concerns, potentially harmful if not handled properly |
Examples of Other Water Treatment Systems
Several water treatment systems can address hard water without relying on water softeners. These methods are tailored to specific mineral issues.
- Reverse Osmosis Systems: These systems use semipermeable membranes to remove dissolved minerals and other contaminants. They are effective at removing a wide range of impurities but can lead to the loss of essential minerals. They require specialized maintenance and can produce significant amounts of wastewater.
- Activated Carbon Filters: Activated carbon filters are often used to remove impurities like chlorine, pesticides, and other organic compounds. They are less effective at removing dissolved minerals, but can be part of a multi-stage filtration system.
- Ultrafiltration Systems: These systems use a porous membrane to filter out larger particles, including some minerals, but not necessarily all dissolved minerals.
Chemical Processes in Alternative Methods
Understanding the chemical reactions is crucial for evaluating the efficacy and environmental impact of different methods.
- Water Softening (with regeneration): Ion exchange resins in water softeners exchange sodium ions for calcium and magnesium ions in hard water.
Na+(aq) + Ca 2+(aq) ↔ Ca 2+(resin) + 2Na +(aq)
I’ve been wondering if my water softener is contributing to my recent blood pressure issues. It’s a common question, but it’s often intertwined with other potential factors, like heavy menstrual periods, which can lead to iron deficiency anemia. A condition like heavy menstrual periods iron deficiency anemia can significantly impact overall health and blood pressure. So, while I’m still researching the water softener connection, I’m also looking at other potential contributing factors.
It’s a bit of a detective story, and hopefully, I’ll get some clearer answers soon!
- Reverse Osmosis: Pressure forces water through a semipermeable membrane, separating dissolved minerals and other impurities from the water. The exact chemical processes depend on the specific membrane and contaminants.
Recommendations for Consumers
Making informed decisions about water softeners, particularly regarding their potential impact on blood pressure, requires careful consideration. This section provides a practical guide to help you navigate the process, ensuring you prioritize your health.
Steps to Consider Before Installing a Water Softener
Evaluating the need for a water softener involves more than just water hardness. Understanding your personal health conditions and consulting with healthcare professionals is crucial. A thorough assessment helps you make the best decision for your well-being.
- Assess your water hardness: While water hardness is a factor, it’s not the sole determinant. Water quality reports from your local utility can provide data on your specific water composition.
- Consult with a healthcare professional: Discuss your family history, current health conditions, and any medications you’re taking. A doctor can provide personalized guidance and address any potential concerns.
- Monitor your blood pressure regularly: Regular blood pressure monitoring, ideally with a home blood pressure monitor, is essential. This data will serve as a baseline and track potential changes over time.
Importance of Professional Consultation
A healthcare professional can offer invaluable insight, especially when considering potential health impacts. Their expertise is vital in determining if a water softener is appropriate for your situation.
- Personalized health assessment: Doctors can evaluate your individual risk factors and assess how water softener use might interact with existing health conditions or medications.
- Potential blood pressure implications: A healthcare provider can advise you on whether the potential for blood pressure changes due to a water softener warrants further investigation.
- Alternative solutions: Your doctor might suggest alternative strategies for managing water hardness without the potential for adverse effects.
Questions to Ask Your Doctor About Water Softeners
Preparation is key when discussing water softeners with your doctor. Clear communication ensures you receive the most helpful information.
- “Are there any known health concerns associated with my water quality, and how might a water softener affect them?”
- “Considering my family history and current health, what are the potential risks and benefits of using a water softener?”
- “Are there alternative methods to manage water hardness without potentially increasing blood pressure?”
- “How can I best monitor my blood pressure before, during, and after using a water softener?”
Maintaining Healthy Blood Pressure Levels
Maintaining healthy blood pressure levels is essential for overall well-being. A proactive approach to blood pressure management can significantly reduce risks associated with various health issues.
- Regular exercise: Incorporating regular physical activity into your routine is vital for cardiovascular health.
- Balanced diet: A diet rich in fruits, vegetables, and whole grains, while limiting sodium intake, supports healthy blood pressure.
- Stress management: Implementing stress-reducing techniques, such as meditation or yoga, can contribute to better blood pressure control.
A Step-by-Step Guide for Consumers, Is my water softener raising my blood pressure
This structured approach simplifies the process of making informed decisions about water softeners.
- Assess water quality and your health history. Gather data from your local water utility and consult your doctor about potential health concerns.
- Monitor your blood pressure regularly. Establish a baseline for your blood pressure before considering a water softener.
- Consult with a healthcare professional. Discuss your concerns and any potential interactions with your current medications or health conditions.
- Incorporate healthy lifestyle choices. Maintain a balanced diet, engage in regular exercise, and manage stress effectively.
- Make an informed decision. Consider all factors, including water quality, potential health impacts, and your overall well-being, when deciding whether to install a water softener.
Concluding Remarks

In conclusion, the potential correlation between water softener use and blood pressure is a complex issue requiring careful consideration. While there’s no definitive proof that water softeners directly cause high blood pressure, the increased sodium intake from softened water is a significant factor to consider. Understanding the science behind water softening, the role of sodium in the body, and the factors influencing blood pressure is crucial for informed decisions.
Consulting with a healthcare professional is always recommended to discuss any concerns and to tailor a plan that supports your overall health and well-being.