New stroke prevention guidelines offer a crucial update to existing strategies, aiming to reduce the risk of this debilitating condition. This comprehensive guide delves into the historical context, key improvements, and practical application of these new guidelines. From lifestyle modifications to medication strategies, we’ll explore the multifaceted approach to stroke prevention.
The new stroke prevention guidelines build upon previous recommendations, addressing advancements in medical knowledge and patient care. A detailed breakdown of target populations, risk factors, and preventive strategies will be presented, accompanied by comparative effectiveness analyses. This information empowers individuals and healthcare professionals to navigate the new guidelines effectively.
Introduction to Stroke Prevention Guidelines
The new stroke prevention guidelines represent a significant advancement in our understanding and approach to mitigating this debilitating condition. These updated guidelines aim to equip healthcare professionals and individuals with the most current and effective strategies for stroke prevention, ultimately reducing the global burden of stroke. They build upon decades of research and clinical experience, incorporating the latest scientific evidence to provide a more comprehensive and personalized approach to stroke prevention.The historical context of stroke prevention guidelines reveals a progression from a focus on risk factors to a more multifaceted approach.
Early guidelines often emphasized managing hypertension and hyperlipidemia. However, evolving knowledge of stroke mechanisms and risk factors has led to a more comprehensive approach that incorporates lifestyle modifications, pharmacological interventions, and the importance of individual risk profiles. This new iteration reflects this evolution.Key improvements in the new guidelines include a stronger emphasis on individual risk assessment, personalized interventions, and the integration of emerging research.
Compared to previous versions, the guidelines now provide more specific recommendations for diverse populations, incorporating genetic predispositions and lifestyle factors. The integration of novel technologies, such as advanced imaging and genetic testing, further enhances the precision of stroke risk prediction and tailored interventions.
Target Population for the New Guidelines
These guidelines recognize that stroke risk varies significantly across different demographic groups and individuals. To address this diversity, the guidelines have been designed to provide tailored recommendations based on specific risk factors.
| Risk Factor Category | Specific Risk Factor | Age Group | Population Demographics |
|---|---|---|---|
| Hypertension | Systolic blood pressure consistently above 140 mmHg | Adults aged 40-75 | Individuals with a family history of hypertension, African Americans, and those with a sedentary lifestyle. |
| Diabetes | Elevated blood glucose levels | Adults aged 35-70 | Individuals with a family history of diabetes, overweight or obese individuals, and those with a history of gestational diabetes. |
| Atrial Fibrillation | Irregular heart rhythm | Adults aged 65 and above | Individuals with a history of heart conditions, especially those with a family history of atrial fibrillation or other cardiac conditions. |
| Smoking | Active cigarette smoking | Adults aged 18-65 | Individuals with a family history of cardiovascular diseases, particularly smokers with a history of other risk factors. |
| Carotid Artery Disease | Stenosis (narrowing) of the carotid arteries | Adults aged 50 and above | Individuals with a history of high blood pressure, high cholesterol, and those with a family history of stroke or other cardiovascular diseases. |
Key Recommendations and Strategies
These updated stroke prevention guidelines emphasize a multifaceted approach, recognizing that a combination of lifestyle modifications, targeted medications, and proactive screening is crucial for reducing the risk of stroke. This holistic strategy aims to empower individuals to take control of their health and significantly decrease their likelihood of experiencing this debilitating condition.
I’ve been really digging the new stroke prevention guidelines lately. They’re focusing on lifestyle changes, and it’s fascinating how much impact those can have. However, it got me thinking about other potential health risks, like the side effects and risks of oophorectomy, a procedure I’ve read about. Side effects and risks of oophorectomy can vary significantly, and it’s important to be well-informed.
Ultimately, understanding all the potential health factors involved in stroke prevention is crucial for making the best decisions about your health.
Lifestyle Modifications
Adopting healthy lifestyle choices plays a pivotal role in stroke prevention. These modifications not only reduce the risk of stroke but also improve overall health and well-being. Maintaining a balanced diet rich in fruits, vegetables, and whole grains, while limiting processed foods, saturated fats, and excessive sodium intake, is essential. Regular physical activity, such as brisk walking, swimming, or cycling for at least 150 minutes per week, is strongly recommended.
Maintaining a healthy weight, avoiding smoking, and limiting alcohol consumption are also crucial elements of a comprehensive stroke prevention strategy.
Medication Strategies for Stroke Prevention
Medication plays a critical role in stroke prevention, especially for individuals with pre-existing conditions like high blood pressure, high cholesterol, or diabetes. These medications work to manage these risk factors, reducing the likelihood of blood clots and other events that can lead to stroke. The new guidelines emphasize the importance of appropriate medication regimens tailored to individual needs and risk profiles.
Specific medications, such as blood thinners (anticoagulants) or antiplatelet agents, may be prescribed to prevent blood clots from forming. Aspirin is often a key component of prevention strategies. The precise medication, dosage, and duration of treatment are determined through a thorough assessment by a healthcare professional.
The new stroke prevention guidelines are really interesting, focusing on lifestyle changes. But, sometimes, even with the best preventative measures, health challenges like Crohn’s flare-ups can significantly impact overall well-being. Knowing how to handle a Crohn’s flare-up can be crucial for managing the symptoms and getting back on track, as detailed in this helpful guide: how to handle a crohn s flare up.
Ultimately, incorporating these new stroke prevention strategies into a holistic health plan is key.
Early Detection and Screening for Stroke Risk Factors
Proactive screening for stroke risk factors is vital in early detection and intervention. Regular check-ups allow for the early identification of conditions like high blood pressure, high cholesterol, and diabetes. Early detection enables prompt intervention with lifestyle changes and medications, potentially preventing a stroke. This proactive approach empowers individuals to address these risk factors before they lead to serious health complications.
Screening programs can identify individuals at high risk, allowing for personalized strategies to minimize their chances of suffering a stroke.
Comparative Effectiveness of Preventive Strategies
| Strategy | Effectiveness Metrics | Advantages | Disadvantages |
|---|---|---|---|
| Lifestyle Modifications | Studies consistently show that lifestyle changes can significantly reduce stroke risk. Improved diet, exercise, and weight management can lower blood pressure, cholesterol, and blood sugar levels, ultimately diminishing the likelihood of a stroke. | Lifestyle modifications are generally well-tolerated, have long-term benefits for overall health, and are relatively inexpensive compared to medication. | Lifestyle changes require consistent effort and commitment. Sustaining these modifications can be challenging for some individuals. |
| Medication | Pharmacological interventions, when appropriately prescribed, demonstrate proven effectiveness in reducing stroke risk, particularly for those with established cardiovascular risk factors. | Medications can effectively target specific risk factors, offering a targeted approach to stroke prevention. They can help control blood pressure, cholesterol, and blood sugar levels. | Medication may have side effects, and adherence to a medication regimen can be difficult for some individuals. Long-term medication use may also have costs associated with it. |
| Screening | Regular screenings for stroke risk factors, such as blood pressure and cholesterol checks, enable early detection and management of potential problems. Early detection empowers individuals to take proactive steps to reduce their stroke risk. | Early detection allows for prompt intervention and treatment, potentially preventing or delaying the progression of stroke risk factors. Screening is a relatively low-cost way to identify high-risk individuals. | Screening may not always identify every individual at risk. The results may not always be immediately actionable, as follow-up and intervention may be needed. |
Impact and Implications of the New Stroke Prevention Guidelines
The newly released stroke prevention guidelines represent a significant shift in how we approach this critical health issue. These updated recommendations, built upon years of research and clinical experience, aim to reduce stroke incidence and improve patient outcomes. This shift demands a careful examination of the potential impact on healthcare providers, patients, and the overall healthcare system.These updated guidelines, with their emphasis on preventative measures and early intervention, will undoubtedly reshape the landscape of stroke care.
The transition to these new protocols requires a proactive and comprehensive understanding of the changes and their potential consequences.
Impact on Healthcare Providers
Implementing the new guidelines will require healthcare providers to adapt their practices. This includes updating knowledge on the latest risk factors and preventive strategies, which might necessitate additional training or continuing education programs. Physicians will need to incorporate these recommendations into routine patient assessments and develop individualized preventive strategies. Clinicians must also be equipped to manage the potential complications of preventative therapies and accurately assess individual patient needs.
The need for enhanced communication and collaboration among healthcare professionals is crucial for optimal patient care. Increased access to preventative therapies, including medication management and lifestyle modification programs, will be vital.
Impact on Patient Care and Outcomes
The new guidelines promise to enhance patient care and improve outcomes by focusing on proactive prevention. Early identification and management of modifiable risk factors will reduce the incidence of stroke. Personalized preventive strategies will result in more tailored approaches to reduce individual patient risk. Improved access to preventive care and lifestyle interventions will lead to better overall patient health and well-being.
Patients can expect more proactive monitoring and engagement in their health, fostering a collaborative approach to managing their risk. This improved patient care translates to fewer debilitating strokes and better long-term health.
Cost-Effectiveness of the New Guidelines
The cost-effectiveness of the new guidelines is a crucial consideration. While initial investment in training and resources might be substantial, the long-term benefits of preventing strokes are likely to outweigh the costs. Reducing hospitalizations, readmissions, and long-term care needs will result in significant savings to the healthcare system. The reduced incidence of stroke-related complications, such as disability and long-term care requirements, will contribute to a more cost-effective approach to healthcare.
The new stroke prevention guidelines emphasize lifestyle changes, and it’s fascinating how seemingly minor health indicators can offer clues. For instance, a black line on your nail, a seemingly innocuous detail, could sometimes be a sign of a broader underlying health concern, like a blood clot or other cardiovascular issue. Knowing more about this, like what causes a black line on nail , can help you proactively address potential risks.
These new guidelines are crucial for understanding and mitigating those risks, promoting overall well-being.
The focus on lifestyle interventions, which can be implemented with relative ease, offers the potential for a high return on investment.
Expected Changes in Healthcare Resource Utilization
Implementing the new guidelines is expected to lead to measurable changes in healthcare resource utilization. These changes are anticipated to be positive, with a reduced strain on hospital resources. The focus on preventative care should lead to a reduction in hospitalizations and readmissions.
| Resource Type | Expected Change | Rationale | Justification |
|---|---|---|---|
| Hospitalizations | Decrease | Proactive prevention reduces the need for emergency admissions and subsequent hospital stays. | Evidence suggests that lifestyle modifications and early interventions can significantly decrease the risk of stroke, leading to fewer hospitalizations. |
| Readmissions | Decrease | Improved patient management and preventative care reduce the risk of recurrent stroke and associated readmissions. | Studies on post-stroke care have shown that implementing proactive preventative measures and improving patient adherence to treatment plans lead to fewer readmissions. |
| Emergency Department Visits | Potential Decrease | Early identification and intervention may reduce the need for emergency department visits due to stroke-like symptoms. | Implementing the guidelines can potentially prevent the onset of a stroke, reducing the need for emergency interventions. |
| Long-Term Care | Decrease | Reduced stroke incidence and improved outcomes minimize the need for long-term care services. | Fewer stroke-related disabilities translate to a lower demand for long-term care facilities and services. |
Practical Application and Implementation
Implementing new stroke prevention guidelines effectively requires a multifaceted approach that seamlessly integrates them into existing clinical workflows. This involves clear communication, readily accessible resources, and a commitment to continuous learning and improvement. Success depends on tailoring strategies to specific patient populations and ensuring patient education is comprehensive and easily understood.
Step-by-Step Guide for Integration
Integrating the new guidelines into clinical practice requires a phased approach. First, healthcare providers must thoroughly familiarize themselves with the updated recommendations. Second, existing protocols and documentation systems should be reviewed and modified to incorporate the new guidelines. Third, a system for tracking patient adherence to the guidelines should be established. Finally, ongoing monitoring and evaluation of the implementation process are essential to identify areas for improvement and ensure optimal outcomes.
Training Resources for Healthcare Providers
A comprehensive approach to training healthcare providers is crucial for effective implementation of the new guidelines. This includes diverse learning materials tailored to various roles and skill levels.
| Training Resource Type | Description | Target Audience | Access |
|---|---|---|---|
| Online Modules | Interactive, self-paced modules covering key aspects of the guidelines, including risk assessment, lifestyle modifications, and pharmacotherapy. | Physicians, nurses, pharmacists, and other healthcare professionals. | Accessible via a dedicated online portal. |
| Webinars and Conferences | Live sessions featuring presentations, Q&A sessions, and panel discussions with leading experts in stroke prevention. | All healthcare professionals. | Scheduled events with registration required. |
| Clinical Practice Guidelines | Detailed, evidence-based guidelines providing step-by-step instructions for implementing the new recommendations in clinical practice. | All healthcare professionals. | Available on the organization’s website and internal networks. |
| Workshops and Seminars | Hands-on workshops and seminars focused on specific aspects of the guidelines, like patient education or risk stratification. | Physicians, nurses, and other healthcare professionals. | Scheduled events with registration required. |
Patient Education Strategies
Educating patients about the new guidelines is critical for successful implementation. Clear, concise, and easily understandable language is essential. Visual aids, such as infographics and videos, can enhance comprehension. Encouraging patient participation and active involvement in their care planning is also vital. Examples include providing patients with personalized action plans and empowering them to track their progress.
Tailoring Strategies to Specific Patient Populations
The new guidelines must be tailored to meet the unique needs of diverse patient populations. Consideration should be given to cultural differences, socioeconomic factors, and access to resources. For example, patients with limited literacy may require simplified materials and support. Additionally, individuals from marginalized communities may face barriers to accessing healthcare services, necessitating tailored interventions to address these disparities.
A patient’s prior medical history, lifestyle, and support system should also be considered when tailoring interventions. This personalized approach leads to more effective and equitable stroke prevention strategies.
Future Directions and Research Needs: New Stroke Prevention Guidelines
The newly released stroke prevention guidelines represent a significant advancement in our understanding and management of this debilitating condition. However, the journey towards optimal stroke prevention is an ongoing one, requiring continuous refinement and adaptation based on emerging evidence and evolving patient needs. Future research will be crucial to further optimize these strategies and ensure their broadest possible impact.
Areas for Future Research
Further research is needed to refine the current stroke prevention strategies. This includes exploring the long-term effectiveness of the guidelines across diverse populations, considering factors like socioeconomic status, ethnicity, and access to healthcare. Additionally, investigating the impact of specific lifestyle interventions, such as tailored dietary modifications or exercise programs, on reducing stroke risk in particular subgroups, is essential.
Importance of Ongoing Surveillance and Evaluation
Continuous monitoring and evaluation of the new guidelines are critical to ensure their effectiveness and identify any potential shortcomings or unintended consequences. This involves collecting data on stroke incidence rates before and after implementation, analyzing trends in risk factor management, and identifying potential disparities in outcomes across different demographics. Regular reviews and updates of the guidelines based on emerging data are necessary to maintain their relevance and optimize patient care.
Potential Future Directions in Stroke Prevention
Future research could explore the use of novel biomarkers for early stroke risk prediction, allowing for proactive interventions and personalized preventive strategies. The development of innovative technologies, such as wearable devices for continuous monitoring of risk factors, could facilitate early detection of at-risk individuals and empower them to adopt preventative measures. Integrating existing healthcare systems with telemedicine platforms for remote monitoring and support could further improve access to preventative care and enhance compliance with recommended lifestyle modifications.
Potential Research Questions, New stroke prevention guidelines
| Research Question | Methodology | Expected Outcomes | Significance |
|---|---|---|---|
| Does the implementation of the new stroke prevention guidelines lead to a statistically significant reduction in stroke incidence rates in diverse populations? | Retrospective cohort study comparing stroke incidence rates before and after implementation of the guidelines in different demographic groups. This would include data from national registries or large healthcare databases. | Reduction in stroke incidence rates across different demographic groups. Identification of specific subgroups where the guidelines show greatest effectiveness or where further intervention is needed. | Demonstrates the effectiveness of the guidelines in a real-world setting, and identifies areas for targeted interventions. |
| What is the impact of tailored dietary modifications on stroke risk reduction in individuals with specific comorbidities (e.g., diabetes, hypertension)? | Randomized controlled trial comparing the efficacy of a tailored dietary intervention to a standard care group in patients with identified comorbidities. Dietary compliance would be rigorously monitored. | Reduction in stroke risk factors (blood pressure, blood glucose, lipid levels) in the intervention group, compared to the control group. Identification of specific dietary components that have the greatest impact. | Provides evidence-based recommendations for personalized dietary interventions, which can be incorporated into the guidelines. |
| How effective are wearable devices in facilitating adherence to lifestyle modifications and reducing stroke risk? | Prospective cohort study comparing stroke risk factors and adherence to lifestyle modifications in a group of patients using wearable devices to a control group without the devices. | Improved adherence to lifestyle recommendations, such as diet and exercise, in the device-using group. Reduction in stroke risk factors among users of the devices. | Evaluates the practical application of technology in stroke prevention, and identifies the potential for broader implementation of such devices. |
| Can novel biomarkers identify individuals at high risk of stroke years before the onset of symptoms? | Longitudinal study involving a large cohort of individuals. Blood samples would be collected over time to analyze biomarker levels. Medical records would be analyzed to determine stroke incidence. | Identification of specific biomarkers that predict stroke risk with high sensitivity and specificity. Development of a predictive model based on these biomarkers. | Allows for early intervention and personalized preventative strategies, potentially significantly reducing stroke burden. |
Last Recap
In conclusion, the new stroke prevention guidelines represent a significant advancement in mitigating stroke risk. By incorporating lifestyle changes, targeted medication strategies, and early detection, we can proactively reduce the incidence of this serious condition. The guidelines’ potential impact on healthcare providers, patient outcomes, and resource utilization is substantial, offering a pathway toward a healthier future. Further research and ongoing surveillance are vital for continuous improvement and adaptation of these guidelines.
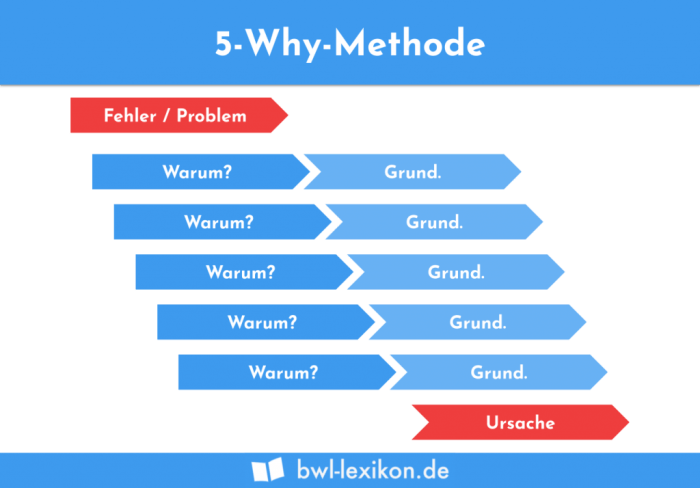


 The flowchart would visually depict the dynamic nature of chronic pain management, showcasing how patient needs may necessitate adjustments to treatment plans. It would clearly indicate points for reassessment and modification of the treatment plan based on the patient’s response. For instance, if a patient doesn’t respond well to initial therapy, the flowchart would guide clinicians toward alternative strategies or adjusting the dosage of buprenorphine. Furthermore, the flowchart would highlight the importance of ongoing monitoring and communication between the patient and the healthcare team.
The flowchart would visually depict the dynamic nature of chronic pain management, showcasing how patient needs may necessitate adjustments to treatment plans. It would clearly indicate points for reassessment and modification of the treatment plan based on the patient’s response. For instance, if a patient doesn’t respond well to initial therapy, the flowchart would guide clinicians toward alternative strategies or adjusting the dosage of buprenorphine. Furthermore, the flowchart would highlight the importance of ongoing monitoring and communication between the patient and the healthcare team.