Skin picking and autoimmune disorders are often linked, though the exact nature of their connection is still being explored. This complex interplay involves the interplay of neurobiological factors, psychological stressors, and potential medication effects. Understanding the symptoms, potential mechanisms, and treatment strategies is crucial for those affected by both skin picking disorder (excoriation disorder) and autoimmune conditions. This exploration dives deep into the shared pathways and the unique challenges faced by individuals grappling with these conditions.
This comprehensive look at skin picking and autoimmune disorders examines the shared neurobiological pathways that might be implicated. It delves into the potential connection between various autoimmune conditions and skin picking behavior. The discussion also highlights the crucial role of psychological factors, like stress and anxiety, in exacerbating these behaviors. We’ll explore the diagnostic criteria, treatment options, and the importance of a multidisciplinary approach to effective management.
Introduction to Skin Picking and Autoimmune Disorders

Skin picking, also known as excoriation disorder, is a chronic, distressing condition characterized by the compulsive urge to pick at one’s skin, often leading to significant physical damage and emotional distress. This repetitive behavior can affect various parts of the body, causing open sores, scarring, and infections. The urge to pick can be triggered by a variety of factors, including stress, anxiety, or even boredom.
Understanding the potential links between skin picking and autoimmune disorders is crucial for effective treatment and management.A growing body of research suggests a possible connection between skin picking and certain autoimmune conditions. Both disorders may share underlying neurobiological vulnerabilities, impacting the brain’s reward system and stress response. This overlap in neurological pathways may explain the potential link between the two.
Potential Connection Between Skin Picking and Autoimmune Disorders
The exact mechanisms linking skin picking to autoimmune disorders are still under investigation. However, shared neurobiological pathways and psychological factors could play a significant role. Stress, anxiety, and emotional dysregulation, which are frequently associated with both skin picking and autoimmune conditions, may contribute to the development and maintenance of these behaviors.
| Condition | Symptoms | Potential Link to Skin Picking |
|---|---|---|
| Psoriasis | Red, scaly patches on the skin, often accompanied by itching and inflammation. | The chronic itchiness and inflammation associated with psoriasis can trigger the urge to pick, potentially leading to secondary skin damage and infection. Increased stress related to managing the condition may also contribute to skin picking. |
| Dermatitis (e.g., eczema) | Dry, itchy, inflamed skin, often with rashes and blisters. | The intense itching and discomfort of dermatitis can make it difficult to resist the urge to pick at the affected areas. This can exacerbate the condition, leading to further skin damage and discomfort. |
| Lupus | A chronic autoimmune disease causing inflammation throughout the body, affecting various organs. Symptoms can include skin rashes, joint pain, fatigue, and kidney problems. | The chronic nature and potential for widespread inflammation associated with lupus can lead to increased stress and anxiety, which may increase the likelihood of skin picking. The physical discomfort from the condition may also contribute to picking behavior. |
| Rheumatoid Arthritis | Chronic inflammation of the joints, leading to pain, swelling, and stiffness. | Chronic pain and discomfort can lead to increased stress and anxiety, which may contribute to skin picking. The need to relieve discomfort in affected areas may also lead to picking. |
Shared Neurobiological Pathways
Several neurobiological pathways are thought to be involved in both skin picking and autoimmune disorders. These include pathways related to:
- Reward Processing: Individuals with skin picking disorder often report a sense of temporary relief or reward from picking. This reinforces the behavior, creating a cycle that is difficult to break. Similar reward pathways might be dysregulated in some autoimmune conditions.
- Stress Response: Chronic stress and anxiety are often associated with both skin picking and autoimmune disorders. Dysregulation of the hypothalamic-pituitary-adrenal (HPA) axis, the body’s stress response system, may contribute to the development and maintenance of both conditions.
- Neuroinflammation: Emerging research suggests a potential role for neuroinflammation in both skin picking and some autoimmune disorders. Inflammation in the brain may contribute to the development of compulsive behaviors and heightened stress responses.
Symptoms and Manifestations
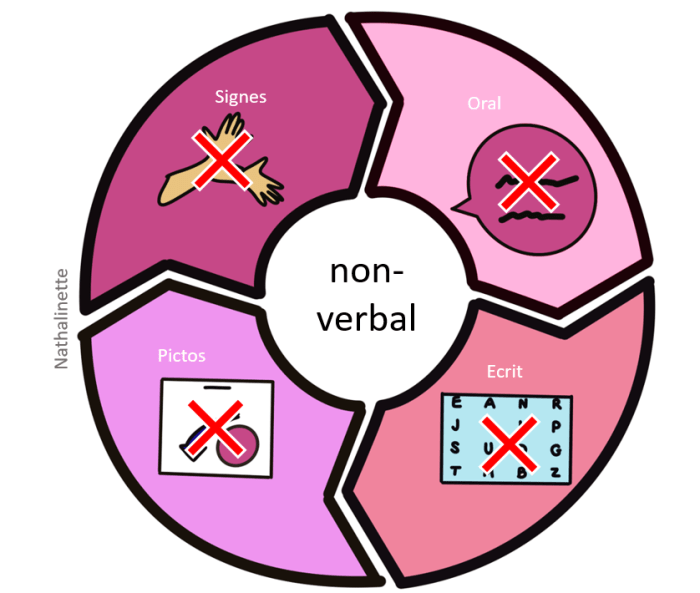
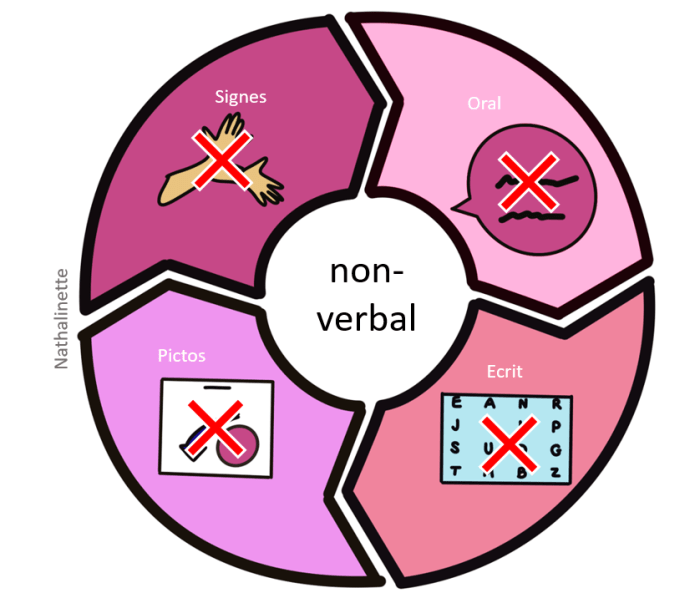
Skin picking, a compulsive behavior, and autoimmune disorders, a complex group of diseases, can share overlapping symptoms and manifestations. Understanding these shared characteristics is crucial for accurate diagnosis and effective treatment. Often, individuals experiencing both conditions face challenges in distinguishing the symptoms, which can lead to delayed or misdirected interventions.The physical expressions of skin picking, coupled with the various manifestations of autoimmune disorders, can create a complex picture for both the affected individual and the healthcare provider.
Recognizing the nuances of these symptoms is essential for tailored management strategies.
Common Symptoms of Skin Picking Disorder
Skin picking disorder, also known as dermatillomania, is characterized by repetitive picking at one’s skin, often leading to noticeable wounds, scars, and infections. This compulsive behavior can manifest in various ways, targeting different areas of the body. Common locations for picking include the face, scalp, and hands. The act itself can be accompanied by a sense of tension or anxiety, which may ease with the act of picking.
The compulsion to pick can be triggered by stress, boredom, or other emotional states. The repetitive nature of the behavior can cause significant physical damage and psychological distress.
Types of Autoimmune Disorders Linked to Skin Picking
Numerous autoimmune disorders may present with skin manifestations and potentially overlap with the behaviors associated with skin picking. Examples include lupus, psoriasis, eczema, and scleroderma. The precise mechanisms linking skin picking to these conditions are not fully understood, but some researchers hypothesize that underlying anxiety and emotional distress associated with the autoimmune conditions may contribute to the compulsive behavior.
Furthermore, the physical discomfort and appearance associated with some autoimmune conditions may increase the urge to pick.
Skin picking and autoimmune disorders can be a tricky combination, especially when your hormones are all over the place. For example, it’s well-documented that fluctuating thyroid levels can significantly impact mood and stress levels, often making existing skin picking tendencies worse. Understanding how these factors intertwine is key to managing both conditions effectively. This can be particularly challenging when your thyroid levels are fluctuating, as explained in more detail here: when your thyroid levels are fluctuating.
It’s all about finding the right balance to help you control skin picking, and addressing the underlying issues like thyroid fluctuations. The connection between these issues can be complex, but recognizing them can help you on your journey to better health.
Physical Manifestations in Different Autoimmune Conditions
The physical manifestations of skin picking can vary considerably depending on the specific autoimmune condition. For instance, in lupus, skin lesions may appear as butterfly-shaped rashes across the face. In psoriasis, skin may exhibit thick, red plaques, particularly on the elbows and knees. Scleroderma can lead to hardening and tightening of the skin, sometimes making it difficult to move certain joints.
Eczema often presents with dry, itchy skin, which may be a trigger for picking in some individuals. Importantly, the appearance of the skin can change and evolve over time with both skin picking and autoimmune disorders, making accurate diagnosis crucial.
Overlap of Symptoms Between Skin Picking and Autoimmune Disorders
The following table illustrates potential overlapping symptoms between skin picking and autoimmune disorders, categorized by body system. It’s crucial to remember that this table is not exhaustive and should not be used for self-diagnosis. Consultation with a healthcare professional is essential for accurate diagnosis and treatment.
| Body System | Skin Picking Symptoms | Autoimmune Disorder Symptoms (Examples) |
|---|---|---|
| Skin | Repeated picking, sores, scars, infections, visible wounds, inflammation, irritation | Rashes, lesions, plaques, dryness, itching, redness, swelling, discoloration |
| Musculoskeletal | (Rarely) pain, stiffness, or discomfort in joints | Joint pain, stiffness, inflammation (e.g., in rheumatoid arthritis), limited range of motion (e.g., in scleroderma) |
| Neurological | Anxiety, tension, emotional distress, altered sensory perception | Headaches, fatigue, cognitive dysfunction (e.g., in lupus) |
| Psychological | Compulsive behavior, anxiety, depression, obsessive thoughts | Depression, anxiety, mood swings (e.g., in lupus) |
Potential Mechanisms and Underlying Factors
Skin picking, a common yet often distressing behavior, can be significantly influenced by a range of factors, particularly when intertwined with autoimmune conditions. Understanding these underlying mechanisms is crucial for developing effective coping strategies and interventions. The psychological toll of autoimmune diseases, combined with the potential for medication side effects, can create a complex interplay that fuels skin picking behaviors.
Ever wondered about the connection between skin picking and autoimmune disorders? It’s a complex relationship, and sometimes, the symptoms overlap with other conditions like rheumatoid arthritis flares. Understanding the symptoms of rheumatoid arthritis flares can be helpful in recognizing patterns and potential triggers. Ultimately, recognizing the connection between skin picking and autoimmune disorders is crucial for managing both conditions effectively.
This exploration delves into the psychological underpinnings, the role of stress and mental health, and the impact of medications on skin picking tendencies in individuals with autoimmune disorders.The complex relationship between autoimmune disorders and skin picking often stems from a confluence of psychological and physiological factors. Individuals navigating the challenges of chronic illness, such as pain, fatigue, and emotional distress, may turn to skin picking as a coping mechanism.
Ever noticed how skin picking can be linked to autoimmune disorders? It’s a complex connection, and often overlooked. Finding the best way to boost fiber without bloating can be a game-changer in managing some of the underlying issues, like digestive discomfort. A good approach to increasing fiber intake is crucial for those with these conditions, which can often lead to inflammation and skin sensitivities.
Check out this guide on best way to boost fiber without bloating for some helpful tips. Ultimately, managing both skin picking and autoimmune disorders requires a holistic approach that considers dietary factors.
This behavior can become a cyclical pattern, where the discomfort of the picking reinforces the urge to pick, and the resulting skin damage perpetuates the emotional distress.
Psychological Factors Contributing to Skin Picking
Autoimmune conditions frequently lead to heightened anxiety, depression, and stress. These psychological factors can directly influence skin picking behaviors. Chronic pain, unpredictable symptoms, and the uncertainty surrounding disease management can all contribute to a heightened state of stress, which, in turn, may increase the urge to pick at the skin. The emotional dysregulation often associated with these conditions can make it difficult for individuals to regulate their impulses, further fueling the cycle of skin picking.
Role of Stress, Anxiety, and Mental Health Conditions
Stress, anxiety, and other mental health conditions, such as obsessive-compulsive disorder (OCD), can exacerbate skin picking behaviors in individuals with autoimmune disorders. The heightened emotional reactivity associated with these conditions can create a strong urge to engage in repetitive behaviors, including skin picking. The stress of managing a chronic illness, coupled with the anxiety about unpredictable symptoms, can make it more challenging for individuals to cope with urges and impulses.
Furthermore, the emotional distress can create a negative feedback loop, where the act of skin picking itself contributes to feelings of shame, guilt, and self-loathing.
Influence of Medication Side Effects
Some medications used to treat autoimmune disorders can have side effects that influence skin picking tendencies. These side effects can include dry skin, changes in skin sensitivity, and even specific skin conditions. These physiological changes can create an environment more conducive to skin picking. The discomfort or irritation associated with these side effects can trigger the urge to pick, perpetuating the cycle.
For example, certain medications can cause increased dryness, leading to an increased desire to pick at dry, flaky skin. Individuals should discuss any potential links between medication side effects and their skin picking behavior with their healthcare providers.
Possible Connections Between Autoimmune Disorders, Psychological Factors, and Skin Picking
| Autoimmune Disorder | Potential Psychological Factors | Potential Skin Picking Behaviors |
|---|---|---|
| Rheumatoid Arthritis | Chronic pain, fatigue, anxiety, depression, fear of disability | Picking at inflamed or painful joints, picking at areas of dryness or skin irritation from medications |
| Psoriasis | Social stigma, anxiety about appearance, body image issues, depression | Picking at inflamed plaques, picking at areas of skin irritation from topical medications |
| Lupus | Chronic pain, fatigue, anxiety, depression, fluctuating symptoms | Picking at skin lesions, picking at areas of dryness or skin irritation from medications, picking at itchy skin |
| Multiple Sclerosis | Physical limitations, anxiety, depression, frustration | Picking at skin lesions, picking at areas of dryness or skin irritation from medications, picking at itchy skin |
This table provides a general overview and individual experiences may vary. It is crucial to remember that these are potential connections and not definitive causal relationships. Professional evaluation and tailored support are essential for understanding the unique interplay of factors contributing to skin picking in each individual.
Diagnosis and Assessment
Unraveling the connection between skin picking and autoimmune disorders requires a meticulous diagnostic process. Simply observing the repetitive behavior isn’t enough; a deeper understanding of the individual’s overall health is crucial. This involves identifying potential underlying autoimmune conditions and assessing the severity and impact of the skin picking itself. A comprehensive approach, considering both the psychological and physiological aspects, is vital for effective treatment planning.A thorough assessment considers not only the physical manifestations of skin picking but also the psychological factors contributing to the behavior.
This multifaceted evaluation aids in distinguishing between the symptoms of skin picking and the symptoms of potential autoimmune disorders. The process often involves a multidisciplinary team, bringing together experts in dermatology, psychiatry, and rheumatology, among others.
Diagnostic Criteria for Skin Picking Disorder
Skin picking disorder, often classified as a body-focused repetitive behavior, is characterized by repetitive picking at the skin, leading to noticeable skin lesions and distress. The diagnostic criteria typically include the presence of recurrent skin picking, causing significant distress or impairment in social, occupational, or other important areas of functioning. This repetitive behavior is not attributable to another medical condition or substance use.
The intensity and frequency of skin picking are key factors in determining the severity of the disorder.
Assessment Methods for Potential Autoimmune Disorders
Identifying potential autoimmune disorders in individuals with skin picking requires a comprehensive approach encompassing various assessment methods. These methods include detailed medical history taking, physical examination, and laboratory testing. A careful review of past medical records and family history can reveal potential genetic predispositions to autoimmune conditions. Physical examination may reveal signs suggestive of specific autoimmune disorders, such as inflammation or joint pain.
Laboratory tests, including blood tests, may be employed to identify specific markers associated with autoimmune conditions.
Importance of a Multidisciplinary Approach
A multidisciplinary approach is paramount in accurately diagnosing and assessing individuals with both skin picking and suspected autoimmune disorders. This approach leverages the expertise of various specialists, such as dermatologists, psychiatrists, rheumatologists, and psychologists. The combined knowledge of these specialists allows for a holistic understanding of the individual’s needs and the complexities of their condition. For example, a dermatologist can assess skin lesions, a psychiatrist can address the psychological aspects of skin picking, and a rheumatologist can investigate potential autoimmune markers.
Diagnostic Tools and Their Relevance
| Diagnostic Tool | Relevance to Connection |
|---|---|
| Medical History | Provides context on past illnesses, family history of autoimmune disorders, and triggers for skin picking. |
| Physical Examination | Identifies physical signs of inflammation, skin lesions, and joint pain that may suggest autoimmune disorders. |
| Laboratory Tests (e.g., blood tests) | Helps identify specific markers associated with autoimmune conditions, such as elevated inflammatory markers or autoantibodies. |
| Psychological Evaluation | Assesses the severity of skin picking, identifies underlying psychological factors, and explores potential comorbid conditions, such as anxiety or depression, which may influence the behavior. |
| Dermatological Examination | Provides insights into the nature and severity of skin lesions, ruling out other dermatological conditions, and monitoring the effectiveness of treatments. |
Treatment and Management Strategies: Skin Picking And Autoimmune Disorders
Unraveling the complexities of skin picking disorder and its potential interplay with autoimmune conditions necessitates a multifaceted approach. Effective treatment strategies aim to address both the behavioral patterns driving the picking and the underlying psychological factors contributing to the issue. Understanding the interplay between these factors is crucial for developing personalized treatment plans.
Behavioral Therapies for Skin Picking
Behavioral therapies play a pivotal role in managing skin picking. These therapies focus on changing the maladaptive behaviors associated with the disorder. Cognitive Behavioral Therapy (CBT) is a particularly effective approach. CBT helps individuals identify and challenge negative thought patterns that may trigger skin picking urges. It also equips individuals with coping mechanisms to manage stress and anxiety, which often exacerbate the urge to pick.
Exposure and response prevention (ERP) is another highly effective behavioral therapy technique. ERP involves gradually exposing individuals to situations that trigger picking urges while preventing the act of picking. This process helps break the cycle of compulsive picking and reduce the urge over time.
Psychotherapy and Counseling
Addressing the underlying psychological factors is critical in the treatment of skin picking. Psychotherapy and counseling can help individuals explore and understand the emotional and mental factors that contribute to their skin picking. Therapy can help individuals identify and process negative emotions, such as stress, anxiety, or boredom, which may trigger the urge to pick. Furthermore, it can provide a safe space for individuals to express their concerns and develop healthy coping mechanisms.
Group therapy can also be beneficial, offering support and shared experiences with others facing similar challenges.
Pharmacological Interventions
Pharmacological interventions may be considered in conjunction with behavioral therapies, particularly when the skin picking is severe or accompanied by co-occurring conditions. For instance, selective serotonin reuptake inhibitors (SSRIs) might be prescribed to help regulate mood and reduce anxiety, which can contribute to picking behaviors. However, the efficacy of pharmacological interventions for skin picking disorder is not consistently established, and the decision to use medication should be made in consultation with a qualified medical professional.
A comprehensive assessment of the individual’s needs and potential side effects is essential.
Treatment Options for Co-occurring Skin Picking and Autoimmune Disorders
| Treatment Option | Description | Effectiveness | Considerations |
|---|---|---|---|
| Cognitive Behavioral Therapy (CBT) | Identifies and challenges negative thought patterns and develops coping mechanisms. | Generally effective, particularly for managing anxiety and stress | Requires active participation and commitment. |
| Exposure and Response Prevention (ERP) | Gradually exposes individuals to triggers while preventing the picking behavior. | Highly effective for breaking the picking cycle. | May be challenging and require gradual exposure. |
| Psychotherapy and Counseling | Addresses underlying psychological factors contributing to the disorder. | Can be very helpful in managing emotional distress. | Requires finding a therapist with experience in treating skin picking. |
| Selective Serotonin Reuptake Inhibitors (SSRIs) | May help regulate mood and reduce anxiety. | Limited evidence for skin picking specifically, effectiveness varies. | Potential side effects and need for close monitoring by a physician. |
A tailored treatment plan, combining behavioral therapies, psychotherapy, and potentially pharmacological interventions, is often the most effective approach for managing skin picking disorder, particularly when co-occurring with autoimmune conditions. The specific combination of treatments will depend on the individual’s unique circumstances and the severity of their condition.
Case Studies and Examples
Unraveling the complex interplay between skin picking and autoimmune disorders requires understanding how these conditions manifest in real-world scenarios. Case studies offer valuable insights into the challenges faced by individuals grappling with both issues, providing a framework for developing effective treatment strategies. The unique experiences and needs of each individual must be considered to tailor interventions that address both the skin picking and the autoimmune condition’s impact.Understanding the specific challenges individuals face with these co-occurring disorders allows healthcare professionals to design personalized care plans.
This approach emphasizes a holistic understanding of the patient’s experiences, enabling them to navigate the complexities of their conditions and achieve a better quality of life.
Illustrative Cases of Co-occurring Conditions
Several case studies highlight the intricate relationship between skin picking and autoimmune disorders. These cases demonstrate the wide range of presentations, from mild to severe, and underscore the need for individualized treatment plans.
- Case 1: A Young Adult with Systemic Lupus Erythematosus (SLE) and Severe Skin Picking: This patient presented with SLE, characterized by joint pain, fatigue, and skin rashes. Simultaneously, she exhibited compulsive skin picking, particularly around the affected skin areas. The skin picking exacerbated existing lesions and created new ones, leading to significant emotional distress and a cycle of self-harm. The patient reported a strong association between stress and increased skin picking urges.
Effective treatment involved addressing the SLE with appropriate medications and therapy, coupled with cognitive behavioral therapy (CBT) to manage the skin picking behavior. This combined approach allowed the patient to better manage both conditions and improve her quality of life.
- Case 2: A Middle-Aged Individual with Psoriasis and Skin Picking Rituals: This individual experienced chronic psoriasis, leading to noticeable skin lesions and significant discomfort. This resulted in repetitive skin picking behaviors, further irritating the skin and hindering healing. The repetitive picking became a ritualistic behavior that provided a temporary sense of relief. Treatment included topical medications for the psoriasis, stress management techniques, and habit reversal training. A key component of the intervention was the development of alternative coping mechanisms for stress and anxiety to break the skin picking cycle.
- Case 3: A Person with Rheumatoid Arthritis (RA) and Skin Picking for Emotional Regulation: This individual struggled with chronic RA, marked by joint pain and stiffness. To manage the intense pain and emotional distress, the patient developed skin picking habits. The picking offered a momentary distraction from the physical discomfort and the accompanying anxiety. Treatment focused on pain management for the RA and mindfulness-based stress reduction techniques to help regulate emotional responses.
The goal was to provide the patient with healthier ways to manage their pain and stress, thereby reducing the urge to pick at their skin.
Challenges in Treatment
Treating individuals with both skin picking and autoimmune disorders presents unique challenges. The symptoms of each condition can exacerbate the other, creating a complex feedback loop. The emotional distress associated with both conditions can also significantly impact treatment adherence.
- Symptom Overlap: Skin lesions associated with autoimmune conditions can be mistaken for skin picking injuries, complicating the diagnosis and treatment process. Accurate identification of both conditions is crucial for effective intervention.
- Emotional Distress: The significant emotional distress often associated with both skin picking and autoimmune disorders can hinder treatment engagement. Addressing the emotional aspects of the conditions through supportive therapy and counseling is critical for successful management.
- Medication Interactions: Some medications used to treat autoimmune disorders may have side effects that exacerbate skin picking behaviors. Careful monitoring and adjustments to medication regimens may be necessary to mitigate these effects.
Potential for Improved Quality of Life
Appropriate intervention strategies can significantly improve the quality of life for individuals experiencing both skin picking and autoimmune disorders. By addressing both conditions holistically, patients can experience reduced symptoms, decreased emotional distress, and improved overall well-being.
- Holistic Approach: A multidisciplinary approach involving dermatologists, psychologists, and other healthcare professionals is essential to address the multifaceted nature of these conditions.
- Patient-Centered Care: Individualized treatment plans that consider the specific needs and preferences of each patient are vital for promoting adherence and positive outcomes.
- Long-Term Support: Ongoing support and follow-up care are critical to maintain progress and prevent relapses.
Research and Future Directions
The connection between skin picking and autoimmune disorders is a complex and relatively unexplored area. While anecdotal evidence and some preliminary studies suggest a potential link, further research is crucial to understand the underlying mechanisms and develop effective interventions. This section will explore the current research landscape and highlight promising avenues for future investigation.
Current Research on the Link
Current research investigating the link between skin picking and autoimmune disorders is limited. Several studies have noted a potential association, but more rigorous investigations are needed to confirm a causal relationship. These studies often focus on observing correlations between the presence of both conditions in patient populations. However, they typically lack the in-depth analysis required to determine the underlying causal pathways.
Need for Further Investigation into Underlying Mechanisms
To fully understand the connection, more research is necessary to uncover the underlying mechanisms. Exploring the potential role of stress, neurobiological factors, and genetic predispositions in both conditions is crucial. It is important to investigate the interplay between the immune system’s response and the psychological factors associated with skin picking. The development of sophisticated methodologies for studying these intricate interactions is vital for future progress.
For example, longitudinal studies tracking individuals with both skin picking and autoimmune disorders over extended periods could reveal valuable insights.
Potential Areas for Future Research
Future research should explore several key areas to better understand the interplay between skin picking and autoimmune disorders. This includes investigations into:
- Neurobiological pathways: Examining the impact of stress hormones on immune function and skin picking behaviors, particularly focusing on the interplay between the central nervous system and the immune response.
- Genetic predisposition: Identifying genetic markers that might increase the risk of both skin picking and autoimmune disorders. This would involve comparing the genetic profiles of individuals with both conditions to those with only one or neither. This would help establish a genetic correlation.
- Psychological factors: Investigating the role of anxiety, depression, and other psychological factors in exacerbating both skin picking and autoimmune responses. This could involve exploring how psychological interventions for skin picking might also impact the progression or severity of autoimmune conditions.
- Immunological mechanisms: Studying the potential effects of skin picking on immune cell activity and the inflammatory response. This would investigate how physical trauma from skin picking could trigger or worsen autoimmune reactions.
Summary Table of Current Research Findings
| Autoimmune Disorder | Current Research Findings (Summary) |
|---|---|
| Rheumatoid Arthritis | Some studies suggest a potential link between skin picking and increased inflammation in rheumatoid arthritis patients. However, the nature and strength of the correlation are still being investigated. |
| Psoriasis | Limited research exists on the association between skin picking and psoriasis. Preliminary findings suggest a possible connection between psychological stress and skin picking, potentially exacerbating psoriasis symptoms. |
| Lupus | Anecdotal evidence and small case studies indicate a potential correlation between skin picking and lupus flares, but rigorous, large-scale studies are lacking. |
| Other Autoimmune Disorders | For many other autoimmune disorders, the research is virtually nonexistent or extremely limited. Further research is crucial to investigate potential connections. |
Patient Education and Support
Navigating skin picking and autoimmune disorders can be challenging, but understanding these conditions and accessing the right support is crucial for effective management. This involves more than just medical treatment; it requires a holistic approach that empowers individuals to take control of their well-being. Effective patient education plays a vital role in this process, equipping individuals with the knowledge and tools necessary for long-term management.
Available Resources
Numerous resources are available to individuals facing skin picking and autoimmune disorders. These range from educational materials to support groups and online communities. Knowing where to turn for help is an essential first step in managing these conditions.
Support Groups and Online Communities, Skin picking and autoimmune disorders
Support groups and online communities offer a vital lifeline for those struggling with skin picking and autoimmune disorders. These platforms provide a safe space to connect with others who understand the challenges faced, share experiences, and offer mutual encouragement. The shared understanding and empathy found within these communities can significantly improve coping mechanisms and overall well-being. Participating in support groups can offer invaluable practical advice and strategies for managing symptoms, emotional distress, and daily life challenges.
Importance of Patient Education
Patient education is paramount in effectively managing both skin picking and autoimmune disorders. Understanding the nature of the conditions, their potential triggers, and available management strategies is critical for individuals to take an active role in their health. Knowledge empowers individuals to make informed decisions, adhere to treatment plans, and develop healthy coping mechanisms. This knowledge can also reduce anxiety and promote a sense of control.
Key Takeaways for Patients and Caregivers
- Understanding the condition: Familiarize yourself with the specific symptoms, triggers, and potential long-term effects of both skin picking and your particular autoimmune disorder. This knowledge will help you anticipate and manage challenges more effectively.
- Seeking professional support: Consult with healthcare providers specializing in both skin picking and autoimmune disorders. This will help you create a comprehensive treatment plan and address any concerns.
- Identifying triggers: Actively work to identify specific situations, emotions, or environmental factors that trigger skin picking or worsen autoimmune symptoms. Keeping a journal can be a helpful tool in this process.
- Developing coping mechanisms: Explore and implement coping strategies for managing urges to pick and managing the symptoms of your autoimmune disorder. Techniques such as mindfulness, relaxation exercises, and behavioral therapies can be highly effective.
- Building a support network: Connect with support groups or online communities. Sharing experiences with others who understand can be incredibly helpful and validating.
- Prioritizing self-care: Implement strategies for stress reduction, healthy sleep, and balanced nutrition. These factors play a significant role in managing both conditions.
Final Conclusion
In conclusion, the intricate relationship between skin picking and autoimmune disorders underscores the need for a multifaceted approach to understanding and managing these conditions. The interconnectedness of psychological factors, physical manifestations, and treatment strategies emphasizes the importance of a holistic perspective. This discussion has explored the potential mechanisms, diagnostic considerations, and therapeutic interventions available. Future research is crucial to further unravel the complex interplay between these conditions and to refine treatment strategies that best support individuals affected by both.