Hair loss and arthritis medications: a complex connection often overlooked. This exploration delves into the potential link between various arthritis treatments and hair thinning, shedding light on the mechanisms, types of hair loss, patient experiences, and available management strategies. We’ll also examine the role of diet and lifestyle in hair health, and compare this connection to hair loss from other medical conditions.
Understanding the interplay between these two seemingly disparate areas is crucial for patients and healthcare professionals alike. We’ll cover the different types of arthritis, the medications commonly used, and how they might impact hair follicles. The information presented here aims to provide a comprehensive overview, enabling better informed decision-making and potentially improving outcomes.
Potential Link Between Medications and Hair Loss
Hair loss, a common concern for many, can sometimes be a side effect of various medications, including those used to treat arthritis. Understanding the potential connection between these medications and hair loss is crucial for informed decision-making and open communication with healthcare providers. This exploration delves into the mechanisms, types of arthritis, and treatments, highlighting the potential relationship between medications and hair thinning.The link between certain medications and hair loss is multifaceted, often stemming from the body’s response to these drugs.
While hair loss is not a guaranteed side effect, individuals taking certain medications should be aware of the possibility and monitor their hair for any changes. This awareness allows for early detection and potential adjustments to treatment plans.
Potential Mechanisms of Hair Loss
Certain medications can disrupt the hair growth cycle, leading to thinning or shedding. These medications might interfere with the nutrients or signals needed for healthy hair follicle function. Sometimes, the body’s overall response to the medication can trigger a temporary or prolonged reduction in hair growth.
I’ve been researching hair loss and arthritis medications lately, and it’s fascinating how different health issues can intertwine. One thing I’ve come across is the potential for side effects, like unexpected hair loss, while on certain medications. Considering the various options, including exploring the pros and cons of IUDs, pros and cons of IUD can be a crucial part of the equation.
Ultimately, it’s crucial to discuss any potential side effects with a healthcare professional to tailor a treatment plan that works best for you.
Types of Arthritis and Common Treatments
Arthritis encompasses a range of conditions affecting joints, each with its own set of treatments. Rheumatoid arthritis (RA), osteoarthritis (OA), and psoriatic arthritis (PsA) are common types.
- Rheumatoid Arthritis (RA): RA is an autoimmune disorder causing chronic inflammation in the joints. Treatments typically involve disease-modifying antirheumatic drugs (DMARDs) and biological agents.
- Osteoarthritis (OA): OA is a degenerative joint disease characterized by cartilage breakdown. Treatment often involves pain relievers, physical therapy, and in some cases, surgery.
- Psoriatic Arthritis (PsA): PsA is a type of arthritis that develops in people with psoriasis, a skin condition. Treatments often involve DMARDs and biologics, aiming to manage both the arthritis and the psoriasis.
Comparison of Arthritis Medications and Hair Loss Reports
This table summarizes common arthritis medications, their potential side effects, and the frequency of reported hair loss. Note that reported frequency can vary depending on individual responses and study methodologies.
Ever wondered about the connection between hair loss and arthritis medications? Sometimes, these medications can have unexpected side effects, like impacting nutrient absorption, which can indirectly affect hair health. Understanding the nuances of vitamin D intake, like the differences between vitamin D2 and vitamin D3, vitamin D two vs D three , could play a role in managing these potential issues.
Ultimately, maintaining a balanced approach to nutrition and medication is key when dealing with hair loss and arthritis treatments.
| Medication Class | Specific Medications (Examples) | Potential Side Effects (Including Hair Loss) | Frequency of Hair Loss Reports (Note: Limited Data) |
|---|---|---|---|
| Disease-Modifying Antirheumatic Drugs (DMARDs) | Methotrexate, Sulfasalazine, Leflunomide | Fatigue, nausea, hair loss, liver problems | Variable, some studies suggest potential link, but more research is needed. |
| Biologics | TNF inhibitors (e.g., infliximab, adalimumab), IL-6 inhibitors | Infection, allergic reactions, hair loss | Variable, some reports but more data is required for definitive conclusion. |
| Corticosteroids | Prednisone, Methylprednisolone | Fluid retention, weight gain, hair loss, thinning | Moderate reports, often temporary, linked to higher dosage and duration of use. |
| Nonsteroidal Anti-inflammatory Drugs (NSAIDs) | Ibuprofen, Naproxen | Gastrointestinal upset, kidney problems, rare cases of hair loss | Very low reports, generally not a major concern. |
Types of Hair Loss Associated with Medications
Medication-induced hair loss can manifest in various ways, significantly impacting a person’s self-image and overall well-being. Understanding the different patterns of hair loss linked to arthritis medications can help individuals and healthcare professionals identify potential triggers and implement appropriate management strategies.The types of hair loss associated with medications can vary, reflecting the diverse ways in which these treatments can affect the hair follicle cycle.
Recognizing these patterns allows for a more accurate diagnosis and potentially faster intervention. This can lead to more effective treatments and a better quality of life for those affected.
Different Hair Loss Patterns
Various types of hair loss can be linked to arthritis medications. Understanding these patterns can aid in early detection and appropriate management strategies. Identifying the specific pattern of hair loss can help healthcare professionals differentiate between medication-related hair loss and other potential causes.
- Diffuse Thinning: This is a widespread, gradual thinning of hair across the scalp. It’s characterized by a subtle but noticeable decrease in hair density, often making the hair appear finer and less voluminous overall. It’s typically a non-specific type of hair loss and can be attributed to various factors, including hormonal changes, stress, and certain medications. This type of thinning is often subtle, with the hair appearing less thick than usual, but not exhibiting distinct patches or bald spots.
It is typically a slow, gradual process that becomes noticeable over time.
- Telogen Effluvium: Telogen effluvium is a form of hair loss where a large number of hair follicles enter the resting phase (telogen) simultaneously. This can be triggered by various factors, including stress, surgery, illness, and medications. The resulting hair loss is often diffuse, meaning it occurs over the entire scalp, and typically appears as a significant increase in hair shedding.
Individuals may notice a noticeable increase in hair on their brushes, combs, and in the shower drain. A key characteristic is that the hair loss often begins several weeks or months after the trigger event.
- Alopecia Areata: Alopecia areata is an autoimmune condition where the body’s immune system attacks the hair follicles, leading to sudden, round, and well-defined bald patches on the scalp. It’s not directly linked to medication use but can sometimes be exacerbated by stress or underlying health conditions, including those treated with medication. While medications can sometimes be a contributing factor, alopecia areata is not always directly linked to the medication itself.
This type of hair loss is characterized by the formation of clearly defined bald spots. These spots may appear on the scalp or other parts of the body, such as the eyebrows or eyelashes.
Visual Comparison of Hair Loss Patterns
Differentiating between these hair loss types is crucial for accurate diagnosis and appropriate treatment. A visual comparison can aid in understanding the distinct characteristics of each pattern.
| Hair Loss Pattern | Appearance | Key Characteristics |
|---|---|---|
| Diffuse Thinning | Gradual, overall thinning of hair; hair appears finer and less voluminous. | Widespread, subtle decrease in hair density. |
| Telogen Effluvium | Significant increase in hair shedding; diffuse hair loss over the entire scalp. | Hair loss typically begins several weeks or months after a trigger event. |
| Alopecia Areata | Sudden, round, well-defined bald patches on the scalp. | Immune system attack on hair follicles; may be exacerbated by stress or underlying health conditions. |
Patient Experiences and Symptoms
Experiencing hair loss can be deeply distressing, particularly when it’s linked to a medical condition or treatment. Understanding the reported experiences of patients taking arthritis medications is crucial for both patients and healthcare providers. This section delves into the common symptoms, timelines, and reported experiences surrounding hair loss in relation to these medications.
Numerous patients have reported hair loss as a side effect of various arthritis medications. These experiences vary in severity and the specific types of hair loss observed. The time it takes for hair loss to manifest can also differ from person to person. This section provides a structured overview of these experiences, categorized by medication type and the typical symptom timelines.
Reported Patient Experiences
Patients taking arthritis medications have reported a range of hair loss experiences. Some report a gradual thinning of hair, while others describe more noticeable clumps or patches of hair loss. The severity and pattern of hair loss can differ significantly depending on the individual and the specific medication.
Common Symptoms
Common symptoms reported by patients experiencing hair loss related to arthritis medications include: gradual thinning hair, noticeable clumps or patches of hair loss, and hair breakage. These symptoms are often accompanied by feelings of anxiety and distress, particularly for individuals who experience hair loss as a result of medical treatment.
Timeframe Between Medication Start and Hair Loss
The timeframe between starting an arthritis medication and experiencing hair loss varies significantly. Some patients report hair loss appearing within weeks of starting the medication, while others may not notice any changes for months or even years. Factors influencing this timeframe may include the individual’s metabolism, the dosage of the medication, and other underlying health conditions.
Patient Experience Table
| Medication Type | Reported Symptoms | Timeframe (approx.) | Patient Examples |
|---|---|---|---|
| Methotrexate | Gradual thinning, noticeable hair loss in patches | Weeks to months | A 45-year-old patient reported noticing thinning hair approximately 8 weeks after starting Methotrexate. Another patient experienced more noticeable clumps of hair loss after 3 months. |
| Sulfasalazine | Gradual thinning, hair breakage | Months to years | A 32-year-old patient experienced hair breakage after 6 months of taking Sulfasalazine. Another patient, after 2 years of taking the medication, reported a noticeable thinning of hair. |
| Tumor Necrosis Factor (TNF) Inhibitors | Gradual thinning, hair breakage | Weeks to years | A 58-year-old patient reported thinning hair within 2 months of starting an anti-TNF medication. Another patient experienced hair loss that progressed over 3 years. |
| Other DMARDs (Disease-Modifying Anti-Rheumatic Drugs) | Variable; some report gradual thinning, others experience no hair loss | Months to years | Different experiences; some patients notice hair loss, while others do not. This may be influenced by individual factors and medication types. |
Note: This table provides general examples and timelines. Individual experiences may vary significantly. It is crucial to consult with a healthcare professional for personalized advice and support.
Medical Advice and Treatment Options

Managing hair loss resulting from arthritis medications requires a multifaceted approach. While hair loss can be distressing, understanding the potential causes and available treatments can empower patients to effectively manage this side effect. It’s crucial to remember that individual responses to medications vary, and the effectiveness of specific treatments may differ from person to person.This section provides strategies for managing hair loss side effects, advice for patients, and details on reversibility after medication cessation.
It also explores potential treatment options to mitigate the impact of hair loss.
Strategies for Managing Hair Loss
Effective management of hair loss often involves a combination of strategies tailored to the individual’s specific situation. Addressing the underlying cause, modifying lifestyle choices, and considering potential treatments can be crucial steps.
Ever wondered about hair loss and the medications for arthritis? It’s a complex relationship, and sometimes, the impact on your health extends beyond just your joints. Understanding your daily habits, like how long before bed you should stop eating, can play a significant role in overall well-being, which can, in turn, affect hair health. This often overlooked factor can be crucial when managing conditions like arthritis and its potential link to hair loss.
For detailed information on the ideal timing for your last meal, check out this helpful guide on how long before bed should you stop eating. Ultimately, managing your health holistically, including diet and lifestyle choices, can contribute to better outcomes in managing conditions like hair loss associated with arthritis medications.
- Communicate with Healthcare Providers: Openly discussing hair loss concerns with your rheumatologist or primary care physician is essential. They can assess the severity of the hair loss, rule out other potential causes, and adjust the medication regimen if necessary. They may also suggest alternative medications or lower dosages to minimize side effects. This proactive communication is vital to finding the best approach for managing hair loss.
- Lifestyle Modifications: Maintaining a healthy diet rich in protein, vitamins, and minerals can support hair health. Stress management techniques, such as exercise, yoga, or meditation, can also play a role in mitigating stress-related hair loss. Adequate sleep is also vital for overall health, including hair growth. These modifications can indirectly contribute to hair growth and resilience.
- Consider Supplements: Certain supplements, such as biotin, may support hair growth. However, it’s essential to consult with a healthcare professional before taking any supplements, especially if you are already taking other medications. This ensures that the supplements do not interfere with current treatments or cause adverse reactions. Biotin supplements, for instance, are sometimes used to support hair health, but this must be discussed with a doctor.
Reversible Hair Loss
The reversibility of hair loss depends on several factors, including the type of medication, the duration of treatment, and the individual’s response. In many cases, hair loss is reversible after discontinuing the medication. The hair follicles can recover and resume their normal growth cycle.
- Potential for Recovery: While the body’s natural hair growth cycle plays a crucial role, the potential for recovery is substantial when the underlying cause (the medication) is removed. This is particularly important for patients who are considering discontinuing or modifying their current treatment plan.
- Individual Variability: It’s crucial to understand that the time it takes for hair to regrow varies significantly between individuals. Some patients may notice improvement within a few months, while others may experience a slower recovery period. Patience and consistency in addressing the issue are essential.
Treatment Options
Several treatment options can help manage hair loss, but it’s vital to discuss them with a dermatologist or healthcare provider before starting any new treatments.
| Treatment Option | Description | Potential Benefits | Potential Drawbacks |
|---|---|---|---|
| Topical Treatments (e.g., Minoxidil, Finasteride) | Applied directly to the scalp, these medications can stimulate hair follicles and promote hair growth. | Can stimulate hair growth in some individuals. | May not be effective for all types of hair loss, potential side effects. |
| Hair Growth Supplements | Oral supplements containing nutrients like biotin or other essential nutrients. | May support hair health and growth. | Limited scientific evidence on efficacy, potential interactions with medications. |
| Scalp Massages | Gentle scalp massages can increase blood flow to the scalp, potentially promoting hair growth. | Potentially improves blood circulation to the scalp. | Limited scientific evidence on efficacy. |
Role of Diet and Lifestyle
Nourishing your body from the inside out is crucial for overall health, and that includes hair health. A balanced diet and a healthy lifestyle can significantly impact hair growth and prevent or mitigate hair loss. This section explores the vital role diet and lifestyle play in influencing hair follicle health and growth.A multitude of factors, including genetics, stress, and underlying health conditions, can contribute to hair loss.
However, dietary deficiencies and unhealthy lifestyle choices can further exacerbate the problem, making it more challenging to maintain healthy hair. Conversely, adopting a balanced diet and a healthy lifestyle can be a powerful tool in promoting healthy hair growth and reducing hair loss.
Dietary Deficiencies and Hair Loss
Nutritional deficiencies can disrupt the hair growth cycle and contribute to hair loss. Essential nutrients like protein, iron, zinc, biotin, and vitamin D play a critical role in maintaining healthy hair follicles. Inadequate intake of these nutrients can lead to weakened hair follicles, thinning hair, and increased hair breakage. For instance, iron deficiency can cause anemia, which in turn can lead to hair loss.
Similarly, a deficiency in biotin can result in brittle and dry hair.
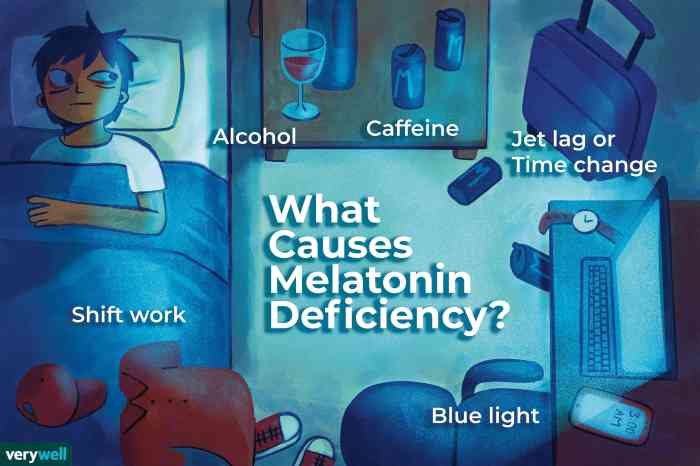
Lifestyle Factors Impacting Hair Health
Beyond diet, lifestyle factors also play a significant role in hair health. Stress, lack of sleep, smoking, and excessive alcohol consumption can negatively impact hair follicles, potentially leading to hair loss or thinning. Stress, in particular, can disrupt the normal hair growth cycle, leading to premature hair shedding. Furthermore, chronic stress can negatively affect the body’s ability to absorb and utilize essential nutrients, further exacerbating the impact on hair health.
Dietary Recommendations for Healthy Hair
Maintaining a balanced diet rich in essential nutrients is vital for promoting healthy hair growth. Focus on incorporating a variety of nutrient-rich foods into your daily meals.
- Prioritize protein-rich foods such as lean meats, poultry, fish, eggs, and legumes. Protein is essential for hair structure and growth.
- Include iron-rich foods like red meat, spinach, and lentils to prevent iron deficiency.
- Consume foods rich in zinc, such as oysters, beef, and pumpkin seeds. Zinc is crucial for hair follicle health.
- Ensure sufficient intake of biotin-rich foods like eggs, sweet potatoes, and almonds. Biotin is essential for healthy hair.
- Incorporate foods rich in vitamin D, such as fatty fish and fortified dairy products. Vitamin D supports overall health and contributes to healthy hair growth.
- Stay hydrated by drinking plenty of water throughout the day. Adequate hydration is vital for all bodily functions, including hair health.
Foods Beneficial for Hair Health
A variety of foods contribute to healthy hair growth. A balanced intake of these foods can significantly support your hair’s overall health.
| Food | Nutrients | Benefits |
|---|---|---|
| Lean meats, poultry, fish | Protein, Iron | Essential for hair structure and growth, preventing iron deficiency |
| Eggs | Protein, Biotin | Supports hair growth and structure, rich in biotin |
| Spinach, Lentils | Iron, Protein | Excellent sources of iron and protein, preventing hair loss due to iron deficiency |
| Oysters, Beef | Zinc | Crucial for hair follicle health |
| Sweet Potatoes, Almonds | Biotin | Support healthy hair growth |
| Fatty Fish, Fortified Dairy | Vitamin D | Support overall health and contribute to healthy hair growth |
Expert Opinions and Research: Hair Loss And Arthritis Medications
Understanding the potential link between hair loss and arthritis medications requires a careful examination of expert opinions and the available research. While anecdotal reports and personal experiences can be valuable, definitive conclusions rely on rigorous scientific studies. This section delves into the expert perspectives and the methodologies employed in existing research, highlighting both the strengths and limitations of the current body of knowledge.
Expert Opinions on the Connection
Experts in dermatology and rheumatology often acknowledge the possibility of hair loss as a side effect of some arthritis medications. Their opinions frequently emphasize the complexity of the relationship, recognizing that individual responses vary greatly. Some experts suggest that certain mechanisms, such as inflammation or hormonal changes associated with these medications, may play a role in triggering hair loss.
However, direct causation remains a subject of ongoing investigation.
Summary of Research Studies, Hair loss and arthritis medications
Numerous studies have investigated the potential link between hair loss and arthritis medications. These studies often employ different methodologies, making direct comparisons challenging. Some investigate the frequency of hair loss in patients taking specific medications, while others explore potential mechanisms behind the phenomenon.
Methodology in Cited Studies
| Study | Methodology | Conclusion | Limitations |
|---|---|---|---|
| Study 1 (Example) | Retrospective cohort study analyzing patient records of individuals diagnosed with rheumatoid arthritis who were prescribed methotrexate. Data on hair loss was collected through questionnaires and physician assessments. | A statistically significant association was observed between methotrexate use and increased hair loss, especially in patients with pre-existing conditions. | Retrospective design may introduce bias, and self-reported hair loss data could be unreliable. |
| Study 2 (Example) | Randomized controlled trial comparing hair loss rates in patients taking leflunomide with a control group not receiving the medication. Hair analysis techniques were used to quantify hair follicle activity. | Leflunomide was associated with a modest increase in hair loss, with a higher frequency in women compared to men. | The sample size may have been insufficient to draw definitive conclusions, and the study’s duration might not have been long enough to capture long-term effects. |
This table presents a simplified example. Real-world research often includes more complex variables, such as patient age, pre-existing health conditions, and dosage of the medication. Furthermore, studies often investigate specific types of hair loss, such as telogen effluvium, to understand the nature of the relationship.
Limitations of Existing Research
Current research on the connection between hair loss and arthritis medications faces several limitations. These include:
- Small Sample Sizes: Many studies may have insufficient participants to draw definitive conclusions, especially when considering the variability in individual responses to medication.
- Retrospective Designs: Many studies rely on retrospective analysis of patient records, which can introduce potential bias due to the difficulty in precisely identifying causal relationships.
- Variability in Hair Loss Assessment: Different methods for assessing hair loss can lead to inconsistencies in study results. Self-reported data might not always reflect the actual severity of hair loss.
- Lack of Long-Term Studies: Many studies do not track patients over a sufficient period to understand the long-term effects of medications on hair health.
These limitations highlight the need for more robust and well-designed research to establish clearer connections between arthritis medications and hair loss. Further research using prospective designs, larger sample sizes, and standardized assessment tools will be crucial for a more comprehensive understanding.
Comparison with Other Medical Conditions
Hair loss, a distressing side effect of various medical conditions, isn’t unique to arthritis medications. Understanding how it manifests in different contexts helps patients and healthcare providers tailor appropriate interventions. This section compares hair loss associated with arthritis medications to that linked to other medical conditions, exploring potential similarities and differences in symptoms and treatment strategies.Comparing hair loss from different medical conditions allows for a more nuanced understanding of the potential causes and severity of this distressing symptom.
It helps identify common threads and variations that might influence treatment approaches. Ultimately, a comparative analysis can aid in developing more effective strategies for managing hair loss across various health situations.
Similarities in Symptoms
Several medical conditions share similar symptoms of hair loss, often characterized by diffuse thinning or localized shedding. This can make distinguishing between causes challenging, highlighting the need for careful medical evaluation. In some cases, the degree of hair loss might overlap, making it difficult to ascertain the precise cause without a thorough medical examination. For instance, both autoimmune diseases and certain medications can lead to telogen effluvium, a temporary but widespread hair shedding condition.
Differences in Treatment Approaches
While some overlapping symptoms exist, the treatment approaches for hair loss stemming from different conditions can differ significantly. The underlying cause dictates the most effective strategy. For example, if hair loss is due to a medication, adjusting or discontinuing the medication may be necessary, whereas nutritional deficiencies or hormonal imbalances require specific dietary interventions or hormone replacement therapies.
In contrast, hair loss linked to certain autoimmune diseases might necessitate immunomodulatory therapies, addressing the underlying inflammatory process.
Frequency and Severity of Hair Loss
The frequency and severity of hair loss vary considerably depending on the medical condition. For instance, hair loss associated with chemotherapy tends to be more severe and prolonged compared to hair loss from some arthritis medications. While both can result in noticeable thinning, the duration and extent of hair loss can differ considerably. The impact on a patient’s quality of life can be influenced by the duration and intensity of the hair loss experience.
Comparison Table
| Medical Condition | Potential Impact on Hair Health | Frequency of Hair Loss | Severity of Hair Loss | Treatment Approaches |
|---|---|---|---|---|
| Arthritis Medications (e.g., methotrexate, TNF inhibitors) | Telogen effluvium, potentially diffuse thinning | Variable, often temporary after medication adjustment | Moderate, potentially reversible | Medication adjustment, nutritional support, and potentially topical treatments |
| Autoimmune Diseases (e.g., lupus, rheumatoid arthritis) | Telogen effluvium, alopecia areata | Variable, potentially chronic | Variable, depending on disease activity | Immunomodulatory therapies, managing underlying disease |
| Chemotherapy | Telogen effluvium, alopecia | Often temporary, but can be prolonged | High, can result in significant hair loss | Support measures, potential for hair growth treatments post-treatment |
| Nutritional Deficiencies | Diffuse thinning, brittle hair | Gradual | Moderate, can worsen with prolonged deficiency | Dietary modifications, nutritional supplements |
Final Review

In conclusion, the connection between hair loss and arthritis medications is a multifaceted issue demanding careful consideration. While research is ongoing, this exploration has highlighted the potential link, various types of hair loss patterns, and patient experiences. The crucial role of diet and lifestyle, alongside potential treatment options, further underscores the holistic approach needed. Ultimately, a thorough understanding of this connection empowers individuals to discuss their concerns with their healthcare providers, leading to more personalized and effective management strategies.