Is blue waffle really an STD? This question, popping up in online discussions, sparks curiosity and concern. Understanding the term “blue waffle” and its potential connection to sexually transmitted infections (STIs) is crucial for navigating the often confusing world of online information. We’ll dive into the meaning of this term, explore common STIs and their transmission, and debunk potential misinformation.
This exploration will provide a clear explanation of how to distinguish between factual information and misinformation about STIs. We’ll discuss reliable sources for accurate sexual health information and explore the potential harm of spreading misinformation. Ultimately, we aim to provide a resource for anyone seeking reliable knowledge about this topic.
Defining “Blue Waffle”
The term “blue waffle,” when encountered in online discussions related to sexually transmitted infections (STIs), often carries a perplexing and potentially misleading connotation. It’s crucial to understand that this term isn’t a recognized medical condition or a standard diagnostic term within the medical community. This ambiguity necessitates a careful examination of its various interpretations and potential origins.The phrase’s meaning is often shrouded in ambiguity, frequently appearing in online forums and social media conversations about sexual health.
So, is blue waffle really an STD? The short answer is no. It’s important to get accurate information from reliable sources, not just online rumours. Thinking about potential health concerns like psoriasis and family planning, for example, can be really helpful in understanding how different conditions impact choices. For more on the relationship between psoriasis and family planning, check out this resource from Valley Ridge Health: psoriasis and family planning.
Ultimately, the best way to stay informed about sexual health is to consult with a healthcare professional. So, no, blue waffle is not an STD.
Its use can range from playful attempts at euphemism to outright misinformation. Deconstructing the possible interpretations helps clarify the lack of medical validity associated with the term.
Possible Interpretations of “Blue Waffle”
The lack of a standardized definition for “blue waffle” in the context of STIs necessitates an analysis of its diverse interpretations within online discussions. Understanding these different usages is essential to navigating the often-confusing world of online health information.
- Euphemism or Codeword: In some online circles, “blue waffle” might be used as a coded or euphemistic term for a specific STI. This usage is problematic, as it obscures the actual condition and can lead to confusion and potential health risks.
- Misinformation or Misunderstanding: The term could represent a misunderstanding or misrepresentation of a real STI. This is especially prevalent in online environments where information is not rigorously vetted.
- Urban Legend or Online Meme: In some cases, “blue waffle” might be part of an online meme or urban legend, having no basis in reality. These fabricated terms often circulate through social media and can lead to anxieties and misinformation.
Origins and Potential Connections
The origins of the term “blue waffle” remain unclear in the context of STIs. It’s possible the term originated from a specific online community or cultural reference, but without a definitive source, its exact history remains unknown. The absence of a clear origin makes it difficult to assess its potential connection to sexual health or cultural contexts. This lack of transparency underscores the importance of critically evaluating online information.
Table of “Blue Waffle” Interpretations
| Term | Definition | Possible Meaning | Example Use |
|---|---|---|---|
| Blue Waffle | A term not recognized in medical contexts. | Euphemism for a specific STI, misunderstanding of an existing STI, or an online meme. | “I heard someone talking about a blue waffle. Is that a new STI?” |
| Blue Waffle | A coded term, potentially harmful. | Used to conceal information about an STI, leading to potentially delayed diagnosis and treatment. | “My partner mentioned a blue waffle. Should I be concerned?” |
Examining the Concept of STIs
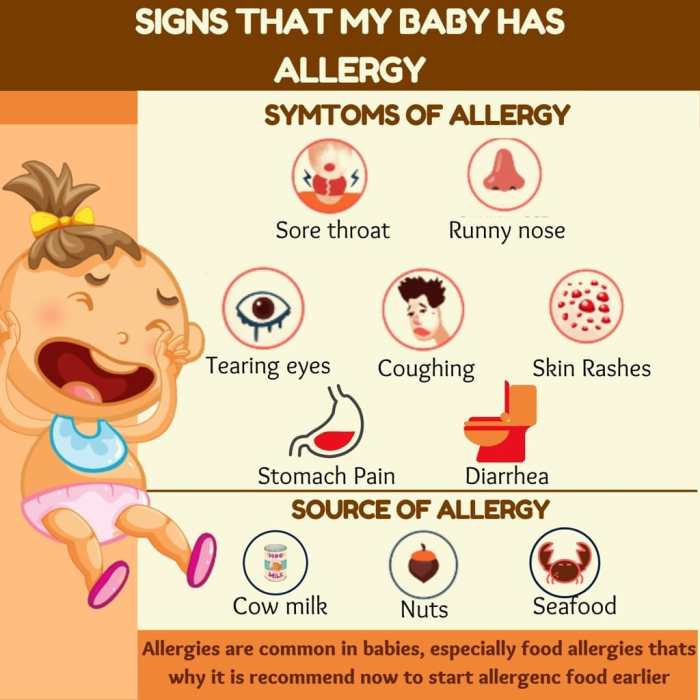
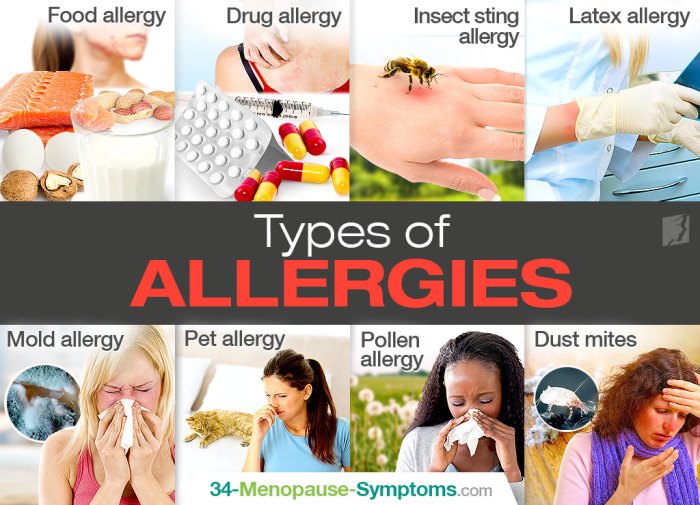
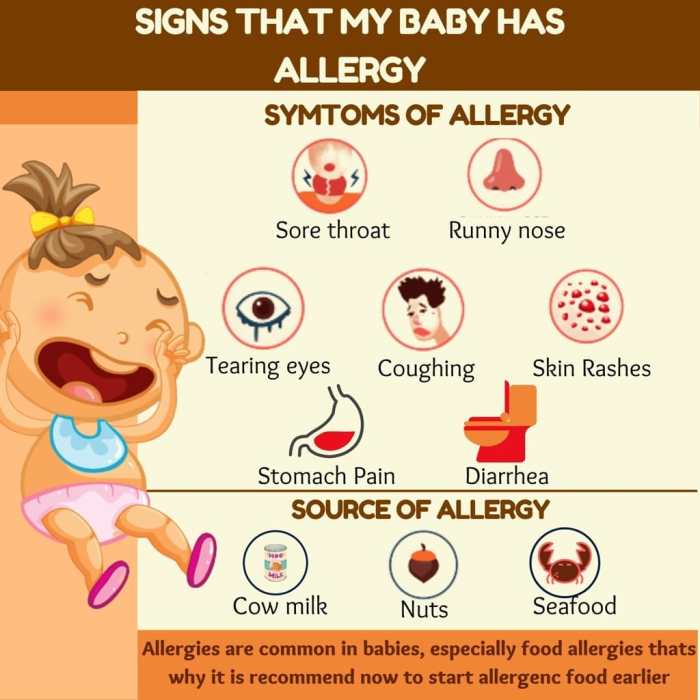
Sexually transmitted infections (STIs), previously known as sexually transmitted diseases (STDs), are a significant public health concern. Understanding how STIs are transmitted, the symptoms they can cause, and the importance of accurate information is crucial for preventing their spread and ensuring the well-being of individuals and communities. Comprehensive knowledge empowers individuals to make informed choices and seek timely medical attention when necessary.Accurate information about STIs is essential for effective prevention and treatment.
Misconceptions and rumors can hinder efforts to address the issue, leading to delayed diagnosis and treatment, increased transmission rates, and potentially severe health consequences. A clear understanding of the facts, along with readily available resources, can help mitigate these negative impacts.
Common Sexually Transmitted Infections
Knowledge of common STIs is vital for proactive health management. This knowledge allows individuals to recognize potential symptoms and seek prompt medical attention.
- Chlamydia: This bacterial infection is frequently asymptomatic, particularly in women. Symptoms, when present, can include abnormal vaginal discharge, painful urination, and lower abdominal pain.
- Gonorrhea: Similar to chlamydia, gonorrhea can be asymptomatic, particularly in women. Symptoms can include painful urination, abnormal discharge, and in severe cases, pelvic inflammatory disease.
- Syphilis: Syphilis progresses through stages, each with different symptoms. Early symptoms can include sores (chancres) at the site of infection, which can easily go unnoticed. Later stages can lead to serious complications affecting various organs.
- Human Papillomavirus (HPV): HPV is a common viral infection, often transmitted through skin-to-skin contact during sexual activity. While many HPV infections resolve without causing symptoms, some types can lead to genital warts or cervical cancer.
- HIV/AIDS: HIV, if left untreated, can progress to AIDS. Initial symptoms can be flu-like, making it difficult to identify. Over time, HIV can damage the immune system, increasing susceptibility to opportunistic infections.
Transmission Methods of STIs
Understanding how STIs are transmitted is crucial for effective prevention strategies. Individuals can take proactive steps to minimize their risk of exposure.
- Sexual Contact: STIs are frequently transmitted through sexual contact, including vaginal, anal, and oral sex. The risk is increased with multiple partners and unprotected sexual activity.
- Blood-to-Blood Contact: Some STIs, such as HIV, can be transmitted through the exchange of blood, such as through sharing needles or contaminated blood transfusions. This emphasizes the importance of safe practices in blood donation and injection procedures.
- Mother-to-Child Transmission: Certain STIs can be transmitted from a pregnant mother to her child during childbirth or breastfeeding. This underscores the importance of prenatal care and testing for pregnant women.
Importance of Accurate Information
Accurate information regarding STIs is vital for public health. Misinformation can lead to significant negative consequences.
- Promoting Healthy Behaviors: Accurate information empowers individuals to make informed decisions about their sexual health, leading to safer behaviors and reduced transmission rates.
- Preventing Disease: Awareness of symptoms and transmission methods allows individuals to seek testing and treatment promptly, reducing the risk of complications and long-term health issues.
Impact of Misinformation
Misinformation surrounding STIs can significantly harm public health. This can result in delayed diagnosis and treatment, leading to more severe health problems.
- Delayed Treatment: False information may discourage individuals from seeking testing and treatment, leading to prolonged infection and potential complications.
- Increased Transmission: Misinformation about prevention methods can result in increased transmission rates and further spread of STIs within communities.
Prevention Strategies
Comprehensive prevention strategies are essential to mitigate the spread of STIs.
| STI | Transmission Methods | Symptoms | Prevention |
|---|---|---|---|
| Chlamydia | Sexual contact | Often asymptomatic, but can include abnormal discharge, painful urination | Safe sex practices, regular testing |
| Gonorrhea | Sexual contact | Often asymptomatic, but can include painful urination, abnormal discharge | Safe sex practices, regular testing |
| Syphilis | Sexual contact, blood-to-blood contact | Sores (chancres), skin rashes, internal organ damage | Safe sex practices, regular testing |
| HPV | Skin-to-skin contact | Often asymptomatic, but can lead to genital warts, cervical cancer | Safe sex practices, vaccination |
| HIV/AIDS | Sexual contact, blood-to-blood contact, mother-to-child transmission | Flu-like symptoms initially, immune system damage | Safe sex practices, safe injection practices, antiretroviral therapy |
Exploring Misinformation and Urban Legends
The internet and social media have become fertile ground for the spread of misinformation, and sexual health topics are unfortunately no exception. Rumors and false claims about sexually transmitted infections (STIs) can have serious consequences, causing unnecessary fear and anxiety, and potentially hindering individuals from seeking crucial medical care. Understanding the patterns of misinformation and the impact it has on public health is crucial to fostering informed decision-making and promoting accurate knowledge.Misinformation about STIs often circulates rapidly, fueled by the ease of online sharing and the tendency for people to believe and share information they encounter without critically evaluating its validity.
This is particularly concerning given the emotional and potentially harmful implications for those who encounter and believe these rumors. It’s vital to examine the factors that contribute to the spread of these narratives and the ways in which they can be challenged.
Prevalence of Misinformation and Rumors
Misinformation about STIs often stems from a combination of factors, including the desire to sensationalize events, the spread of inaccurate or incomplete information, and the exploitation of anxieties surrounding sexual health. A lack of comprehensive sex education, combined with a fear of the unknown, can make individuals more susceptible to believing unsubstantiated claims.
Common Patterns in the Spread of Misinformation
Several patterns contribute to the rapid spread of misinformation about STIs. These include the use of emotional language to evoke fear and anxiety, the creation of compelling but false narratives, and the exploitation of existing biases and prejudices. The lack of verifiable sources, the use of anonymity in online forums, and the rapid sharing of information without verification all play a role in amplifying the spread of misinformation.
Impact of Rumors on Sexual Health
Rumors and misinformation about STIs can have a significant negative impact on individuals’ sexual health. The fear and anxiety generated by these false claims can deter people from seeking testing and treatment, leading to delayed diagnosis and potential complications. Furthermore, this fear can create barriers to open communication about sexual health, making it more difficult to address concerns and obtain accurate information.
Examples of Similar Urban Legends in Health Topics
Similar patterns of misinformation are observed in other health topics. For example, there are numerous urban legends surrounding vaccinations, claiming they cause autism or other serious health problems. These myths, despite being thoroughly debunked by scientific evidence, persist in some communities. The same mechanisms of emotional appeal, sensationalism, and rapid online dissemination drive the spread of these unsubstantiated claims.
Common Misconceptions about STIs
| Misconception | Reality |
|---|---|
| Certain STIs can only be transmitted through vaginal sex. | STIs can be transmitted through various sexual contact methods, including oral and anal sex. |
| You can tell if someone has an STI by looking at them. | Many STIs have no noticeable symptoms in the early stages. |
| You only get an STI if you have multiple sexual partners. | STIs can be transmitted through a single sexual encounter with an infected partner. |
| Some STIs can be cured with home remedies. | STIs require professional medical treatment and cannot be cured with home remedies. |
Analyzing Potential Interpretations of “Blue Waffle”: Is Blue Waffle Really An Std

The term “blue waffle” has emerged as a curious and often perplexing phrase, especially in online discussions and certain subcultures. Its meaning is not immediately obvious, and its presence in the context of sexual activities adds an intriguing layer of ambiguity. Deciphering the potential interpretations requires examining the term’s possible connections to sexual activity, exploring its use across cultures, and understanding its potential metaphorical and playful applications.The term’s ambiguity stems from its lack of a universally accepted definition.
Its presence in sexual contexts, especially in online communities, suggests a coded or shared understanding. Understanding this code requires careful consideration of cultural contexts and the nuances of language use. It’s important to remember that the interpretation of “blue waffle” can vary widely.
Potential Connections to Sexual Activities
The connection between “blue waffle” and sexual activities likely arises from its association with specific imagery or concepts. This association could be a result of online slang, cultural references, or even a combination of both. The term itself doesn’t explicitly describe a sexual act; instead, its meaning is often derived from the context in which it’s used. This context can include shared understandings within particular communities or online platforms.
Different Interpretations in Cultural Contexts
The interpretation of “blue waffle” varies significantly depending on the cultural context. In some cultures, it might be associated with specific sexual practices or have a completely different meaning. Understanding these diverse interpretations is crucial to avoid misinterpretations or miscommunications. The use of the term in a playful or metaphorical way can also influence its meaning.
Playful or Metaphorical Usage
The term “blue waffle” might also be employed in a playful or metaphorical context. It could be a creative way to refer to something else entirely, potentially unrelated to sexual activity. This metaphorical use can be influenced by humor or shared understandings within a specific group. Understanding the potential for playful use helps to deconstruct the term’s meaning and its implications.
Implications of Using “Blue Waffle” in a Sexual Context
Using “blue waffle” in a sexual context can carry several implications, depending on the specific situation. It could be intended to create a sense of intimacy, excitement, or even humor. However, it could also lead to misinterpretations or misunderstandings, particularly if the recipient isn’t familiar with the specific cultural or online context. Careful consideration of the audience and the potential for misinterpretation is crucial.
Table of Interpretations and Potential Meanings
| Interpretation | Potential Meaning | Contextual Clues |
|---|---|---|
| Coded Sexual Reference | A veiled or indirect reference to a sexual act or activity | Used in online forums, chat rooms, or private messages; often accompanied by suggestive imagery or innuendo. |
| Playful Metaphor | A non-literal or humorous reference to something else | Used in a lighthearted manner, often in contexts not explicitly sexual. |
| Cultural Specific Slang | A term with a meaning unique to a particular group or community. | Used within a specific subculture or online community; lack of understanding outside that community. |
| Misinformation or Urban Legend | A term used to spread false information or create a sense of mystery. | Used to perpetuate rumors or misconceptions. |
Distinguishing Fact from Fiction
Navigating the world of health information, especially concerning sensitive topics like sexually transmitted infections (STIs), can be tricky. Misinformation and urban legends often spread faster than factual data, leading to confusion and anxiety. Developing critical thinking skills is crucial to separating truth from falsehood. This section will Artikel strategies to discern accurate information from fabricated claims.Reliable sources of health information are essential for making informed decisions about your well-being.
By understanding the characteristics of trustworthy sources and comparing them to unreliable ones, you can avoid potentially harmful misconceptions.
Identifying Reliable Sources
Reliable sources for sexual health information are crucial for avoiding misinformation. These sources prioritize accuracy, evidence-based research, and expert consensus. They are transparent about their funding and methodology, ensuring objectivity. Reputable sources provide detailed explanations, supporting their claims with evidence, and avoid sensationalism or alarmist language.
Comparing Reliable and Unreliable Sources
Distinguishing between reliable and unreliable sources is paramount for navigating the complexities of health information. Reliable sources are characterized by their commitment to accuracy, evidence-based research, and transparency. Conversely, unreliable sources often prioritize sensationalism, lack rigorous methodology, and may be driven by profit or agenda.
| Reliable Source | Unreliable Source | Explanation |
|---|---|---|
| Reputable medical organizations (e.g., CDC, WHO, Planned Parenthood) | Social media posts, blogs by unqualified individuals, forums with unverified information | Official health organizations conduct rigorous research and compile data from various studies to provide accurate and comprehensive information. Conversely, social media and blogs often lack expert review and verification. |
| Peer-reviewed scientific journals | Websites with vague or unverifiable sources, conspiracy theories | Peer-reviewed journals ensure the quality of published research through rigorous evaluation by other experts in the field. Unverified websites and conspiracy theories are typically not supported by credible evidence. |
| Government health websites (e.g., the National Institutes of Health) | Blogs or websites promoting specific products or therapies | Government websites often compile data from diverse research and are subject to stringent review processes. Websites promoting products often have commercial interests that may compromise objectivity. |
| Trusted medical professionals (doctors, nurses, counselors) | Self-proclaimed “experts” or “healers” | Medical professionals have undergone extensive training and are committed to evidence-based practice. Unsubstantiated “experts” lack formal credentials and may disseminate inaccurate or dangerous information. |
Evaluating Information Critically
Critical evaluation of information is paramount for distinguishing fact from fiction. Look for evidence-based claims, logical reasoning, and clear citations. Beware of vague or sensational language. Seek multiple sources to corroborate information. Scrutinize the source’s credentials and any potential biases.
Checking for the presence of verifiable citations and evidence-based claims is vital.
So, is blue waffle actually an STD? The short answer is no. While it might sound like a fun, flirty nickname, it’s not a sexually transmitted infection. Instead, focusing on foot care is crucial, especially when it comes to conditions like ingrown toenails. If you’re looking for a comprehensive overview of ingrown toenail care and treatment options, check out this informative guide: ingrown toenail overview and more.
Ultimately, there’s no need to worry about blue waffle being an STD; it’s just a fun, and somewhat misleading, term.
Addressing Potential Harm
Misinformation, particularly about sensitive topics like sexually transmitted infections (STIs), can have devastating consequences. The spread of inaccurate or fabricated claims can lead to significant health risks and exacerbate existing societal anxieties. This section delves into the potential harms of believing or spreading misinformation regarding STIs, including the “blue waffle” myth.
Negative Consequences of Believing Misinformation, Is blue waffle really an std
Misinformation about STIs can significantly impact individuals’ health decisions, often leading to delayed or avoided medical care. A person who believes a false claim might delay seeking testing or treatment, potentially exacerbating the infection and increasing the risk of complications or transmission to others. The anxiety and fear surrounding STIs can also cause emotional distress and mental health issues.
So, is a blue waffle really an STD? Definitely not. While it might sound like a weird question, it highlights how important it is to rely on credible sources for health information. Thinking about heart failure causes and risk factors, like high blood pressure or a family history of the condition heart failure causes and risk factors , can help us understand the importance of accurate information.
Misinformation about things like STDs can be quite harmful, so it’s essential to check reliable sources before drawing any conclusions.
The lack of access to accurate information can lead to a cascade of negative effects, ultimately hindering individuals’ ability to make informed choices about their health.
Impact on Health Decisions
The impact of misinformation on health decisions is profound. People who believe inaccurate claims about STIs, like the “blue waffle” myth, may delay or avoid necessary testing and treatment. This can result in the progression of an infection, potentially leading to more severe health complications. The fear and anxiety generated by misinformation can also make individuals reluctant to discuss their health concerns with healthcare professionals, further hindering appropriate medical intervention.
This can also affect their relationships with partners.
Misinformation Leading to Avoidance of Medical Care
The fear of judgment, stigma, or embarrassment associated with STIs, often amplified by misinformation, can lead individuals to avoid seeking necessary medical care. This avoidance can have serious health consequences. For example, a person who believes that a particular symptom is not associated with an STI may delay seeking professional help, allowing the infection to progress to a more advanced stage.
This delay can lead to irreversible damage to their health.
Strategies for Countering Misinformation
Combating the spread of misinformation requires a multifaceted approach. This includes promoting accurate and evidence-based information through reputable sources, like public health organizations and medical professionals. Critical thinking skills need to be developed to allow individuals to evaluate the validity of information they encounter. Social media platforms should take proactive measures to curb the spread of misinformation by implementing fact-checking tools and flagging false or misleading content.
Building trust in reliable sources and encouraging open communication about STIs is crucial to combating this issue.
Table of Potential Harms of Believing in Misinformation
| Aspect | Potential Harm |
|---|---|
| Health Outcomes | Delayed or avoided medical care, progression of infection, increased risk of complications, potential transmission to others |
| Emotional Well-being | Anxiety, fear, stress, stigma, emotional distress, mental health issues |
| Relationship Dynamics | Strained relationships with partners, difficulties in open communication about health concerns |
| Societal Impact | Increased stigma surrounding STIs, hindering public health efforts, decreased access to prevention and treatment |
Describing Relevant Health Resources
Reliable information and professional guidance are crucial when navigating health concerns, especially those related to sexual health. Misinformation can be harmful, and taking action based on false or incomplete data can lead to unnecessary stress and potentially dangerous situations. This section Artikels trusted resources for accurate information and emphasizes the importance of seeking professional medical advice.Accurate information empowers individuals to make informed decisions about their health.
Knowing where to find trustworthy resources and understanding the role of healthcare providers can greatly improve the experience of seeking and receiving appropriate support.
Trusted Organizations for Sexual Health Information
Numerous organizations provide comprehensive and evidence-based information about sexual health. These resources offer factual data and promote responsible behavior. Their expertise and commitment to public health make them invaluable for anyone seeking knowledge.
- The Centers for Disease Control and Prevention (CDC): The CDC is a leading public health agency in the United States. Their website offers a wealth of information on sexually transmitted infections (STIs), including prevention strategies, testing options, and treatment recommendations. They provide resources for individuals and healthcare professionals alike.
- Planned Parenthood: Planned Parenthood is a well-respected organization dedicated to sexual and reproductive health. They offer a variety of services, including education, testing, and treatment for STIs. Their website and local clinics provide vital resources for individuals seeking care.
- World Health Organization (WHO): The WHO is a global organization focused on international public health. They provide essential information on various health topics, including STIs, and their website is a valuable resource for those seeking a global perspective on sexual health issues.
Importance of Seeking Professional Medical Advice
Consulting a healthcare provider is essential for accurate diagnosis and treatment of any health concern, including potential STIs. A healthcare professional can provide personalized guidance based on individual circumstances.
“Seeking medical attention allows for a thorough evaluation and tailored treatment plan.”
Healthcare providers have the expertise to conduct appropriate testing, interpret results, and recommend the most effective course of action. This professional guidance is crucial in ensuring accurate diagnoses and appropriate management of any identified health issues.
Role of Healthcare Providers in Addressing Sexual Health Concerns
Healthcare providers play a critical role in providing comprehensive sexual health care. They are trained to address concerns in a confidential and supportive manner.
- Confidential Discussions: Healthcare providers understand the sensitivity of sexual health concerns and prioritize creating a confidential and comfortable environment for patients.
- Accurate Diagnoses: Providers use their expertise to accurately diagnose and treat potential health issues.
- Personalized Care: They tailor their recommendations to the specific needs of each patient, taking into account individual circumstances.
Credible Online Resources for Sexual Health Information
Reliable online resources can supplement, but not replace, professional medical advice. It is essential to evaluate the source and ensure it is reputable. Carefully consider the credentials of the author and the organization behind the website.
- National Institutes of Health (NIH): The NIH provides a comprehensive collection of health information. Their resources are a valuable source for accurate and evidence-based information.
- Mayo Clinic: The Mayo Clinic is a renowned medical institution that offers extensive health information. Their website provides comprehensive information on various health conditions, including sexual health.
Examples of Credible Resources
| Resource | Description | Contact Information | Services |
|---|---|---|---|
| CDC | Centers for Disease Control and Prevention | (Website) | STI information, prevention, treatment |
| Planned Parenthood | Reproductive health organization | (Website, local clinics) | Education, testing, treatment for STIs |
| WHO | World Health Organization | (Website) | Global perspective on sexual health |
Last Point
In conclusion, while the term “blue waffle” might be used in various contexts, it’s crucial to approach such information with caution. Understanding the difference between fact and fiction regarding STIs is essential for maintaining good sexual health. Reliable sources, medical professionals, and careful consideration of information are key to making informed decisions about your well-being.