Gold plan health insurance what is it? It’s a critical question for anyone navigating the complexities of healthcare coverage. This in-depth exploration delves into the specifics of gold plans, comparing them to other options like bronze, silver, and platinum. We’ll examine coverage details, costs, and enrollment procedures, helping you understand the ins and outs of this popular insurance type.
This article unpacks the key characteristics that distinguish a gold plan from other health insurance options. We’ll cover coverage levels, typical benefits, and a breakdown of costs, ensuring you have a clear understanding of how gold plans work. We’ll also analyze how factors like location, age, and health status affect the premium cost.
Defining Gold Plan Health Insurance

Understanding your health insurance options can feel overwhelming. Different plans offer varying levels of coverage, making it crucial to understand the nuances of each type. This exploration delves into gold plan health insurance, highlighting its characteristics, coverage, and comparison to other plans.Gold plans represent a middle ground in the spectrum of health insurance, providing a balance between cost and coverage.
They generally offer a higher level of coverage than bronze or silver plans, but less than platinum plans. This makes them an attractive option for individuals seeking a solid safety net without the premium price tag of a platinum plan.
Key Characteristics of a Gold Plan
Gold plans are distinguished from other plans by their coverage levels. They fall between the lower coverage of bronze and silver plans and the comprehensive coverage of platinum plans. This positioning directly impacts both the cost and the extent of care included.
Coverage Levels in a Gold Plan
Gold plans typically include substantial coverage for preventative care, such as routine checkups and screenings. They also provide a higher percentage of coverage for covered services like hospital stays, doctor visits, and prescription drugs, compared to bronze or silver plans. Crucially, they often offer greater flexibility in choosing healthcare providers.
Examples of Gold Plan Benefits
Examples of benefits commonly included in gold plans are:
- Preventive care: Routine checkups, immunizations, and screenings are often fully covered or have low out-of-pocket costs. This proactive approach to health is a significant advantage for many individuals.
- Hospital care: Gold plans typically cover a substantial portion of hospital stays, including pre- and post-operative care. This comprehensive coverage is vital for major medical procedures.
- Prescription drugs: Coverage for prescription medications is typically a significant aspect of a gold plan. The specifics of this coverage, however, can vary by plan, so it’s crucial to understand the details.
- Mental health services: Many gold plans now include coverage for mental health services, such as therapy and counseling, which is essential for overall well-being.
Comparison with Other Plans
Understanding how gold plans stack up against other options is crucial for informed decision-making.
| Plan Type | Cost | Coverage | Features |
|---|---|---|---|
| Bronze | Lowest | Lowest | Limited coverage for preventative care and essential services. |
| Silver | Mid-range | Mid-range | Moderate coverage, good balance of cost and benefit. |
| Gold | Mid-range to Higher | Higher | Comprehensive coverage for preventative care, hospital stays, and essential services. |
| Platinum | Highest | Highest | Extensive coverage, including many preventative care services, and a high percentage of cost coverage for most medical services. |
The table above illustrates the trade-offs between cost, coverage, and features for different plan types. Note that costs and coverage percentages can vary based on the specific plan and individual circumstances. Factors like age, location, and pre-existing conditions can influence the premiums and coverage levels.
Understanding Coverage Details

Gold plans offer comprehensive health coverage, but the specific details of what’s covered and how much you’ll pay can vary significantly. Understanding the specifics of your plan is crucial for making informed decisions about your healthcare. This section dives deep into the details of coverage, including typical medical services, out-of-pocket costs, and preventive care.
Medical Services Typically Covered
Gold plans generally cover a wide range of medical services, including doctor visits, hospital stays, prescription drugs, and mental health services. They typically include preventive care like immunizations and screenings, as well as emergency care. The extent of coverage depends on the specific plan and your location.
Out-of-Pocket Maximums and Deductibles
Out-of-pocket maximums and deductibles are key components of understanding your financial responsibility. The out-of-pocket maximum is the most you’ll pay in a given year for covered services, while the deductible is the amount you pay out-of-pocket before your insurance begins to pay. Gold plans typically have lower deductibles and out-of-pocket maximums compared to other plans. For example, a gold plan might have a deductible of $2,000 and an out-of-pocket maximum of $6,000, while a bronze plan might have a higher deductible and out-of-pocket maximum.
Gold plan health insurance, basically, offers comprehensive coverage. But, while you’re researching different plans, consider what impact eating a protein bar daily might have on your body. For example, what happens to your body when you eat a protein bar every day could affect your overall health, and that’s something to factor into your insurance decisions.
Ultimately, a gold plan is a good choice for those seeking extensive protection.
Preventive Care Services
Gold plans often include a wide array of preventive care services. These services are designed to catch health problems early, when they are often easier and less expensive to treat. Examples of preventive care services might include routine checkups, vaccinations, screenings for various conditions like cancer, and wellness programs. These services are often covered at no or low cost to the patient.
Copays, Coinsurance, and Out-of-Pocket Expenses
Copays, coinsurance, and out-of-pocket expenses are additional costs you may encounter when using your health insurance. A copay is a fixed amount you pay for a specific service, like a doctor’s visit. Coinsurance is a percentage of the cost of a service you pay, and out-of-pocket expenses encompass all the costs you pay before your insurance kicks in. Gold plans often have lower copays and coinsurance amounts than other plans, which can help reduce your out-of-pocket costs.
Common Exclusions or Limitations
While gold plans offer broad coverage, there are often some exclusions or limitations. These might include services related to certain pre-existing conditions, experimental treatments, or services provided by out-of-network providers. It’s important to review the specific plan documents to understand any exclusions.
Coverage Details Table
| Component | Description | Example |
|---|---|---|
| Out-of-Pocket Maximum | The maximum amount you’ll pay out-of-pocket for covered services in a plan year. | $6,000 |
| Deductible | The amount you pay out-of-pocket before your insurance starts paying. | $2,000 |
| Copay | A fixed amount you pay for a specific service. | $25 for a doctor’s visit |
| Coinsurance | A percentage of the cost of a service you pay. | 20% of the cost of a hospital stay |
| Covered Services | Types of medical services included. | Doctor visits, hospital stays, prescription drugs, preventive care. |
| Exclusions | Services not covered by the plan. | Experimental treatments, certain pre-existing conditions. |
Factors Influencing Gold Plan Cost
Gold plans, offering comprehensive health coverage, are a valuable investment in your well-being. However, understanding the factors that contribute to their premium costs is crucial for making informed decisions. This section delves into the key elements that shape the price of a gold plan, from location and age to your health status and medical history.Understanding these factors allows you to compare plans effectively and choose the most suitable coverage for your individual needs and financial situation.
Comparing costs across various plans and regions provides a clearer picture of the overall market landscape.
Location’s Impact on Gold Plan Premiums
Geographic location significantly impacts gold plan premiums. Higher costs of medical care in specific regions often translate into higher premiums. This is because the demand for healthcare services and the average cost of treatments vary considerably from one area to another. For instance, metropolitan areas with specialized hospitals and advanced medical facilities typically have higher healthcare costs, resulting in more expensive gold plans.
Rural areas, on the other hand, may have fewer facilities, affecting the availability of specialized care and potentially influencing premiums.
Age and Gold Plan Premiums
Age is a key determinant in gold plan premiums. Generally, younger individuals tend to have lower premiums compared to older adults. This is because younger people are statistically less likely to require extensive medical care. As individuals age, their risk of developing chronic conditions increases, leading to higher potential healthcare costs and consequently, higher premiums.
Health Status and Gold Plan Costs
Your health status directly influences the cost of a gold plan. Individuals with pre-existing conditions, such as chronic diseases or a history of major illnesses, typically face higher premiums. This is because their potential healthcare needs and costs are greater than those of healthier individuals. Insurance companies assess this risk to determine the appropriate premium level.
Medical History’s Role in Premium Determination
A comprehensive medical history is crucial for accurate premium calculation. Past medical procedures, diagnoses, and treatments all contribute to the risk assessment for insurance companies. A history of serious illnesses or procedures necessitates a higher premium, reflecting the increased likelihood of future healthcare needs. This assessment considers factors like the severity and frequency of past health issues.
Comparison of Gold Plan Premiums with Other Plans
Gold plans, due to their extensive coverage, typically have higher premiums compared to plans with less comprehensive benefits. Silver, bronze, and platinum plans offer varying levels of coverage and thus different premium costs. The premium difference reflects the trade-off between the scope of benefits and the cost. It’s essential to weigh the benefits of comprehensive coverage against the associated higher premium.
Impact of Regional Medical Care Costs on Gold Plan Pricing
The cost of medical care in a specific region directly impacts the pricing of gold plans. High medical costs, including hospital services, specialized treatments, and medications, drive up premiums. Regions with a higher concentration of expensive medical facilities or treatments will typically see higher premiums for gold plans.
Factors Influencing Gold Plan Costs: A Summary
| Factor | Impact on Cost |
|---|---|
| Location | Higher costs in areas with more expensive medical care |
| Age | Generally, higher premiums for older individuals due to increased risk |
| Health Status | Higher premiums for individuals with pre-existing conditions |
| Medical History | Premiums adjusted based on past medical procedures and diagnoses |
| Regional Medical Care Costs | Higher costs in regions with high medical care expenses |
Accessing and Utilizing Gold Plans
Navigating the complexities of a gold plan can feel daunting, but understanding the enrollment, claims process, and provider support can make it much smoother. This section provides a clear pathway for effectively using your gold plan, empowering you to maximize its benefits.Successfully utilizing a gold plan involves more than just understanding its coverage; it requires a proactive approach to enrollment, claims submission, and provider interaction.
A well-structured approach will allow you to smoothly navigate the process and receive the care you need without unnecessary stress.
Enrollment Process
The enrollment process for a gold plan typically involves submitting necessary documentation and completing the required forms. This often includes providing personal information, employment details, and possibly medical history. Thorough preparation and accurate completion of the required documents will significantly reduce any potential delays in the enrollment process.
Gold plan health insurance, essentially, offers comprehensive coverage, but understanding its specifics is key. A crucial aspect to consider, particularly for families, is how it might address conditions like congenital adrenal hyperplasia. Learning more about this rare genetic disorder can help you assess if a gold plan provides sufficient coverage for potential treatments and ongoing care, as outlined in this helpful overview: congenital adrenal hyperplasia overview.
Ultimately, the best gold plan for you depends on your individual needs and budget.
- Gather required documents. This might include proof of residency, employment verification, and any pre-existing medical conditions that need to be disclosed. These documents are critical to ensure a smooth and timely enrollment process.
- Complete online or paper applications. Most gold plans now have online portals to facilitate the application process, but paper applications may still be required. Follow the specific instructions provided by your insurance provider to avoid errors.
- Review and submit the application. Carefully review all submitted information for accuracy. Submit the application through the designated channels provided by the insurance provider.
Claim Submission Procedures
Submitting claims efficiently and accurately is crucial for receiving reimbursements under your gold plan. Following the specific guidelines of your plan will ensure your claim is processed promptly.
- Understand claim forms. Familiarize yourself with the claim forms and the required information. The accuracy of the information on the form is paramount for the smooth processing of your claim.
- Gather supporting documentation. This often includes medical bills, receipts, and any other relevant paperwork. Organize this documentation meticulously to avoid delays.
- Submit claims electronically or via mail. Many plans offer online portals for submitting claims, which can significantly speed up the process. Refer to your provider’s guidelines for the preferred method.
Claims Process Navigation, Gold plan health insurance what is it
A clear understanding of the claims process will help you manage your expectations and track the progress of your claims.
- Check claim status online. Most gold plans offer online portals to check the status of your claims. This allows you to monitor the progress and anticipate any potential issues.
- Contact the insurance provider. If you encounter any issues or have questions regarding your claim, contact your insurance provider’s customer service department. They can provide clarification and assist in resolving any problems.
- Appeal decisions. If your claim is denied, you may be able to appeal the decision. Familiarize yourself with the appeal process Artikeld by your insurance provider.
Provider Support for Gold Plan Members
Your health insurance provider plays a vital role in supporting you as a gold plan member. They offer various resources to help you navigate the plan and maximize its benefits.
- Customer service representatives. These representatives can answer questions about the plan’s coverage, procedures, and benefits.
- Online portals. Many providers offer user-friendly online portals to access your account information, submit claims, and track the status of your claims.
- Educational materials. Providers often provide educational materials to help members understand their coverage and utilize their plan effectively.
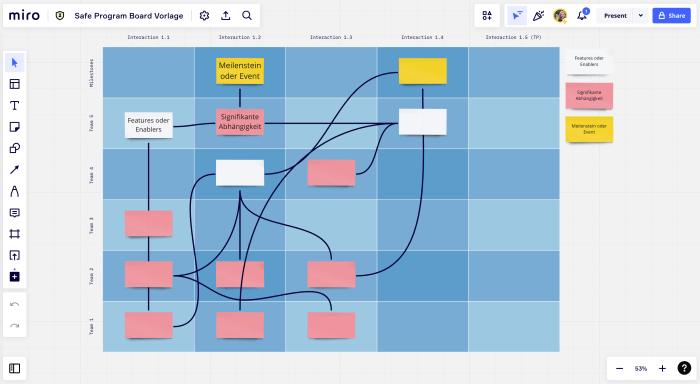
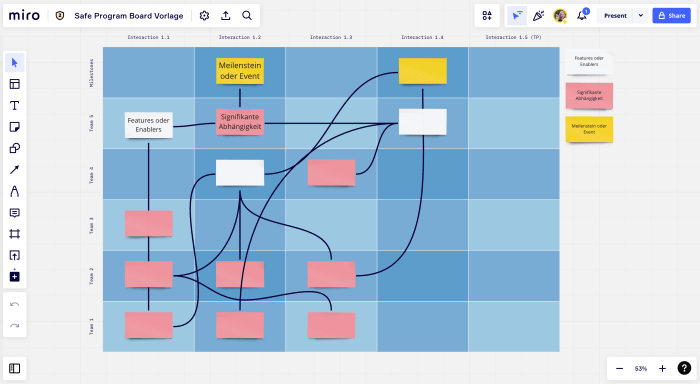
Flow Chart for Using a Gold Plan
 This flowchart provides a visual representation of the steps involved in using a gold plan. The flow chart should be well-labeled and clearly display the steps involved in enrolling, submitting claims, navigating the claims process, and utilizing provider support.
This flowchart provides a visual representation of the steps involved in using a gold plan. The flow chart should be well-labeled and clearly display the steps involved in enrolling, submitting claims, navigating the claims process, and utilizing provider support.
Illustrative Examples of Gold Plans: Gold Plan Health Insurance What Is It
Gold plans, with their comprehensive coverage, can be a significant investment in your health. Understanding the specifics of a particular gold plan can help you make informed decisions about your healthcare choices. Let’s look at a hypothetical example to illustrate the features, benefits, and costs typically associated with a gold plan.
Hypothetical Gold Plan: “Guardian Gold”
This hypothetical plan, “Guardian Gold,” from a fictional insurance provider, exemplifies a typical gold plan. It prioritizes comprehensive health coverage, providing substantial benefits for a wide range of services.
Gold plan health insurance, essentially, offers comprehensive coverage, but what does that truly mean in practice? Understanding the different types of diagnostic medical equipment, like MRIs and X-rays, common types of diagnostic medical equipment , is key to knowing how your insurance will handle those procedures. Ultimately, a gold plan aims to provide maximum coverage for a wide range of medical needs.
Features and Benefits of Guardian Gold
Guardian Gold offers a robust suite of benefits, including preventative care, hospital stays, and prescription drugs. This plan emphasizes proactive health management, aiming to prevent costly illnesses through routine check-ups and screenings. Preventive care services, such as annual physicals and vaccinations, are fully covered, making health maintenance more accessible.
Cost Structure of Guardian Gold
The monthly premium for Guardian Gold is a significant factor to consider. This premium varies based on factors like age, location, and pre-existing conditions. While the premium may be higher than plans with less comprehensive coverage, it often reflects the breadth of benefits included. In addition to the monthly premium, there might be co-pays for certain services and deductibles.
The total cost is influenced by the individual’s utilization of the plan’s services. A breakdown of the cost structure is detailed below.
Coverage Details for Guardian Gold
Guardian Gold provides comprehensive coverage for a wide range of services. The plan includes hospitalizations, doctor visits, and prescription medications. Crucially, the plan offers substantial coverage for preventative care, including routine check-ups, immunizations, and screenings. It also covers a broad spectrum of procedures, such as surgeries and diagnostic tests. Crucially, the plan covers emergency services, ensuring prompt access to critical care.
- Hospitalization: Covers a significant portion of inpatient costs, including room and board, physician fees, and lab tests. Co-pays and deductibles apply.
- Doctor Visits: Includes coverage for routine check-ups, specialist appointments, and urgent care visits. Co-pays are applicable.
- Prescription Drugs: Provides coverage for a wide range of prescription medications. Co-pays and a formulary (a list of covered drugs) are in place.
- Preventative Care: Fully covers routine check-ups, immunizations, and screenings, promoting proactive health management.
- Emergency Services: Offers comprehensive coverage for emergency room visits and transportation to hospitals.
Summary of Guardian Gold
- Comprehensive coverage for a wide array of medical services.
- Strong emphasis on preventative care.
- Significant coverage for hospitalizations and doctor visits.
- Covers a broad spectrum of prescription medications.
- Includes emergency services.
Key Features and Costs of Guardian Gold
| Feature | Description | Cost (Estimated) |
|---|---|---|
| Monthly Premium | Recurring payment for plan coverage | $450 – $600 |
| Deductible | Amount paid by the individual before the insurance kicks in | $2,000 |
| Co-pay (Doctor Visits) | Fixed amount paid at the time of service | $25 – $50 |
| Co-pay (Prescription Drugs) | Fixed amount paid for each prescription | $10 – $20 |
| Out-of-Pocket Maximum | Total amount the individual will pay out of pocket in a year | $6,000 |
Visual Representation of Gold Plan Coverage
Understanding the specifics of a gold plan’s coverage is crucial for making informed decisions. A visual representation helps to quickly grasp the different aspects of the plan, including coverage percentages, out-of-pocket costs, and preventative care benefits. This clarity is vital in comparing gold plans to other options like silver or bronze plans.
Typical Coverage Percentages for Medical Services
Gold plans generally offer a higher percentage of coverage for medical services compared to other plans. Visualizing this difference is key to understanding the financial implications. A visual representation could be a bar graph with different colored bars for various medical services, like doctor visits, hospital stays, prescription drugs, and specialist care. Each bar’s length would represent the percentage covered by the plan.
For example, a gold plan might cover 90% of a doctor’s visit, 80% of a hospital stay, and 70% of prescription medications.
Out-of-Pocket Expenses vs. Premium Cost
Visualizing the relationship between premiums and out-of-pocket costs is essential. A simple graph can illustrate this. The x-axis would represent the premium cost, and the y-axis would represent the anticipated out-of-pocket expenses for a typical year. The graph would show a positive correlation, but the slope would be less steep for a gold plan compared to a bronze plan.
This visual aids in understanding that while gold plans typically have higher premiums, the out-of-pocket costs, on average, are lower.
Preventative Care Coverage Breakdown
Gold plans often have robust preventative care coverage. This is a crucial aspect to highlight. A visual representation could be a pie chart. The pie chart would show the percentage of coverage for preventative care services, such as annual checkups, vaccinations, and screenings. A gold plan would likely show a larger portion of the pie dedicated to preventative care compared to a bronze plan.
For instance, a gold plan might cover 100% of annual checkups, while a bronze plan might cover a smaller percentage.
Comparison of Gold, Silver, Bronze, and Platinum Plans
A visual infographic is a useful tool for comparing different plan types. This infographic could use a series of stacked bar graphs or similar visual representations. Each bar would represent a different type of plan (gold, silver, bronze, and platinum) and the different bars within each graph would illustrate the coverage percentage for various medical services. This allows a quick and easy comparison of the coverage offered by each plan type, making it clear how the coverage levels differ.
For example, a gold plan would generally have higher coverage percentages for most services than a silver plan.
Final Thoughts
In conclusion, gold plan health insurance offers a balanced approach to healthcare coverage, typically providing comprehensive benefits with a higher premium cost. Understanding the specific coverage, costs, and enrollment processes is essential to making an informed decision about your healthcare needs. This guide provides a detailed overview, helping you weigh the pros and cons of a gold plan against other options.