Cancer ribbons colors meanings sets the stage for a fascinating exploration of the symbolism behind these powerful visual representations of hope and solidarity. From the initial use of ribbons in cancer awareness to the evolution of colors and their associations, this comprehensive guide delves into the history, meanings, and cultural contexts surrounding these vital symbols.
We’ll uncover the specific meanings behind each ribbon color, tracing their connection to various cancers and the emotional messages they convey. This journey explores the global perspectives on ribbon usage, highlighting cultural variations and ensuring accurate representation in diverse communities. It also considers the importance of responsible use and avoids misinterpretations, offering practical applications and a deeper understanding of the significance of these symbols.
Introduction to Cancer Ribbons: Cancer Ribbons Colors Meanings
The use of ribbons to symbolize support for various causes, including cancer, has become a powerful visual tool for raising awareness and fostering a sense of community. The evolution of different colored ribbons associated with specific cancers reflects the growing understanding and importance of early detection, treatment, and research. These symbols have transcended mere decoration, becoming potent reminders of the fight against a disease that affects millions globally.The concept of using colored ribbons to represent specific causes gained traction in the late 20th century, becoming increasingly prominent in the 1990s.
The adoption of different ribbon colors facilitated the creation of targeted campaigns, allowing individuals and organizations to focus on specific types of cancer and their related needs. This approach also helps to raise awareness of the diverse range of cancers and the varying experiences of those affected.
Evolution of Cancer Ribbon Colors
The use of ribbons as symbols for cancer awareness has significantly evolved, reflecting the growing understanding of different types of cancer. The choice of colors is often tied to the specific type of cancer, as well as the associated organizations dedicated to supporting those affected. This visual representation has proved invaluable in raising public awareness, encouraging donations, and promoting research.
Cancer Ribbon Color Associations
The use of various colors to represent specific types of cancer has created a recognizable visual language. This system allows for quick identification of the cause being supported, facilitating the mobilization of resources and the expression of solidarity. Each color is carefully selected to resonate with the specific needs and challenges associated with a particular cancer.
| Ribbon Color | Associated Cancer Type | Organization/Cause Description |
|---|---|---|
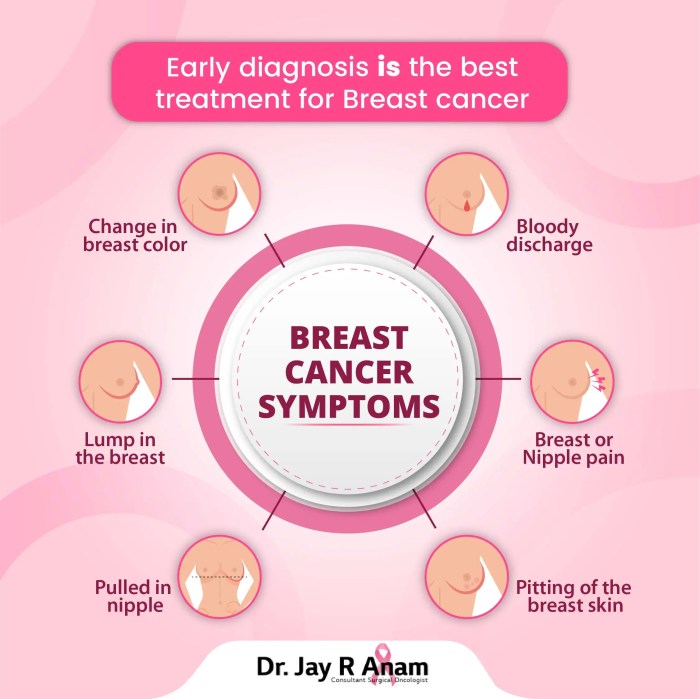
| Pink | Breast Cancer | Pink ribbons are widely recognized as representing breast cancer. Numerous organizations, including Susan G. Komen for the Cure, actively promote breast cancer awareness and research, often through fundraising initiatives. The color pink is widely associated with femininity and compassion, making it a strong visual symbol. |
| Purple | Lupus | Purple ribbons are associated with lupus, an autoimmune disease. The Lupus Foundation of America, for example, utilizes purple to raise awareness about this condition and to provide support to those affected. Lupus often presents challenges due to its complex nature and impact on everyday life. |
| Blue | Prostate Cancer | Blue ribbons are commonly used to raise awareness for prostate cancer. Organizations like the American Cancer Society and the Prostate Cancer Foundation focus on research, early detection, and support for those battling prostate cancer. Early diagnosis and treatment can significantly improve outcomes. |
| Yellow | Leukemia | Yellow ribbons symbolize leukemia, a blood cancer. Organizations like the Leukemia & Lymphoma Society champion research and treatment for leukemia and other blood cancers, providing support and resources for patients and their families. The disease often requires extensive and specialized care. |
| Orange | Ovarian Cancer | Orange ribbons represent ovarian cancer. The Ovarian Cancer National Alliance (OCNA), among other groups, works to raise awareness and provide resources for individuals affected by ovarian cancer. Early detection is critical for better treatment outcomes. |
Understanding the Symbolism
Ribbons, often simple yet powerful symbols, play a crucial role in cancer awareness campaigns. They transcend language barriers and connect individuals globally, fostering a sense of shared purpose and empathy. Beyond their aesthetic appeal, these ribbons carry specific meanings related to different types of cancer and the emotions associated with the fight against the disease. This deeper understanding of the symbolism helps us appreciate the profound impact these seemingly simple accessories have on individuals and communities affected by cancer.The use of colors in cancer ribbons isn’t arbitrary; each hue is meticulously chosen to represent various aspects of the cancer experience.
These colors evoke feelings of hope, resilience, and solidarity, creating a visual language that resonates across cultures and unites people in their collective efforts to combat cancer. The cultural context surrounding these colors and the interpretations they carry are significant factors in understanding the ribbons’ impact.
The Symbolic Meaning of Ribbons
The ribbon itself, as a simple yet versatile piece of fabric, carries significant symbolic weight. Its gentle form and malleability allow it to be molded into a myriad of shapes and colors, representing the various facets of the cancer experience. From conveying hope and resilience to symbolizing solidarity and support, the ribbon is a powerful visual representation of the fight against cancer.
Colors and their Messages
The choice of color for a ribbon is crucial, conveying specific messages about hope, resilience, and solidarity. Each color carries its own weight and cultural associations, making it vital to understand the different interpretations. Pink, for instance, is strongly associated with breast cancer, while other colors represent different cancers and support systems. Understanding the nuances of these colors helps us appreciate the complexity of the messages they convey.
Cultural Interpretations of Colors
The meaning of colors can vary across cultures. While some colors may evoke universal emotions, like hope and strength, their specific connotations can differ depending on cultural backgrounds. Understanding these nuances is essential to avoid misinterpretations or misunderstandings.
Potential Misinterpretations
It is important to be mindful of potential misinterpretations when interpreting the symbolism of cancer ribbons. Different cultures may have distinct associations with colors, and what one culture perceives as a symbol of hope, another may interpret differently. For instance, the color white may represent purity in one culture but mourning in another.
Table of Ribbon Colors and Symbolism
| Color | Commonly Associated Cancer | General Symbolic Meaning | Potential Cultural Variations |
|---|---|---|---|
| Pink | Breast Cancer | Hope, resilience, femininity | May be associated with different emotions in some cultures |
| Purple | Lupus | Awareness, advocacy, remembrance | May represent royalty or spirituality in some cultures |
| Orange | Leukemia | Energy, warmth, vitality | May be associated with harvest or celebration in some cultures |
| Light Blue | Prostate Cancer | Strength, hope, courage | May hold different cultural connotations in some regions |
| Yellow | Childhood Cancer | Joy, optimism, childhood innocence | May represent different aspects of joy or happiness |
Specific Ribbon Colors and Meanings
Beyond the unifying message of hope and support, cancer ribbons come in a spectrum of colors, each with its own specific meaning. These colors serve as powerful visual reminders of the diverse battles fought against this pervasive disease, representing the various types of cancer and the emotions they evoke. Understanding these nuances allows us to appreciate the depth and breadth of the fight against cancer.Different colors have evolved to represent distinct cancer types and to offer a personalized message of solidarity and remembrance.
The symbolic power of these colors is deeply rooted in the history of cancer awareness campaigns, fostering a shared sense of purpose and resilience in the face of adversity.
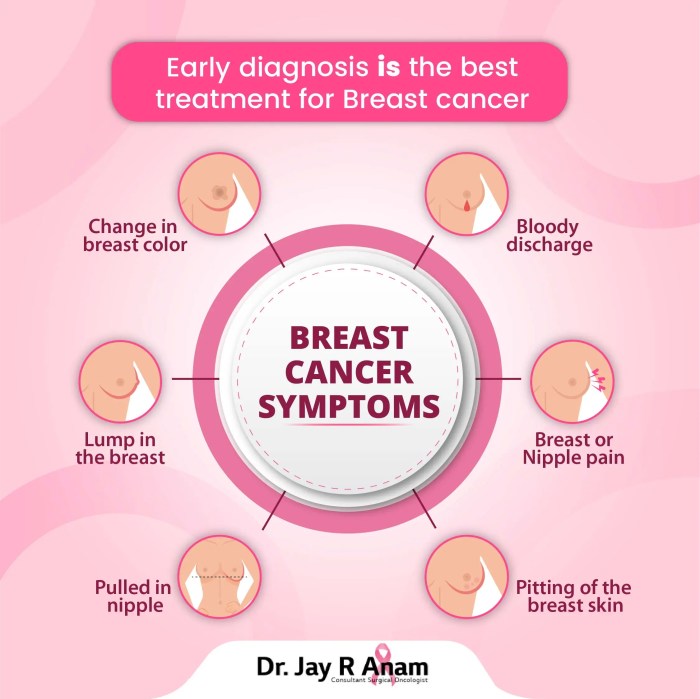
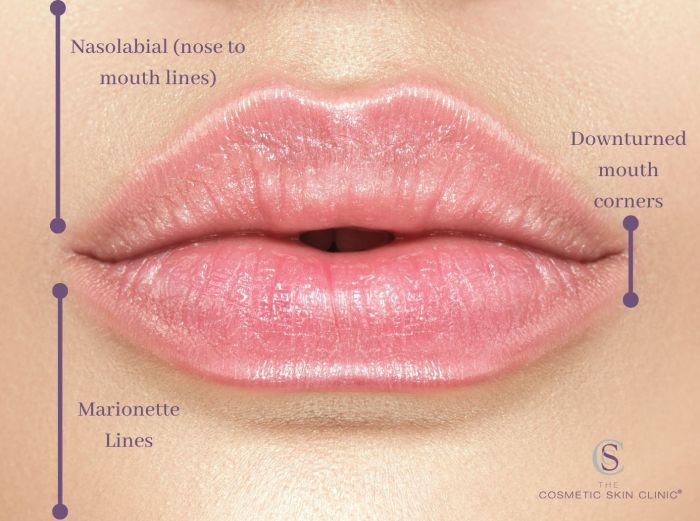
Pink Ribbon: Breast Cancer Awareness
The iconic pink ribbon, instantly recognizable, symbolizes breast cancer awareness. Its widespread adoption has transformed it into a universal symbol of support for those affected by this common cancer. The campaign’s early focus on breast cancer awareness and early detection has led to significant improvements in survival rates. The pink ribbon’s significance extends beyond awareness; it embodies the strength, resilience, and hope of individuals and communities impacted by breast cancer.
Purple Ribbon: Ovarian Cancer Awareness
The purple ribbon signifies ovarian cancer awareness. Its adoption is relatively recent, highlighting the need for greater public awareness surrounding this often-overlooked form of cancer. While not as widely recognized as the pink ribbon, the purple ribbon’s significance lies in its focus on increasing early detection and research funding to combat this type of cancer. The color purple represents a collective effort to support those affected by ovarian cancer.
Orange Ribbon: Childhood Cancer Awareness
The vibrant orange ribbon stands for childhood cancer awareness. Its purpose is to bring attention to the unique challenges and needs of children facing this disease. Childhood cancers often present with distinct characteristics, requiring tailored treatments and support systems. The orange ribbon serves as a powerful reminder of the importance of supporting these vulnerable populations and advocating for research and better treatment options.
It represents a collective call for more funding and resources for pediatric cancer research.
Different cancer ribbons represent various cancers, but have you considered that everyday products like laundry detergent can also cause allergic reactions? Learning about the signs and symptoms of such allergies, like those from laundry detergent allergies signs symptoms and treatment , is crucial. Understanding these reactions can help us better appreciate the importance of each ribbon’s specific message, especially when we consider the variety of potential health impacts.
Ultimately, knowing the meanings behind cancer ribbons is a powerful way to support those battling this disease.
Yellow Ribbon: Leukemia Awareness, Cancer ribbons colors meanings
The bright yellow ribbon signifies leukemia awareness. This cancer affects the blood-forming cells, resulting in diverse symptoms and treatments. The yellow ribbon is a powerful symbol of support for those facing this form of cancer, highlighting the need for increased research and improved treatments for all types of leukemia. The color embodies the spirit of perseverance and hope in the fight against leukemia.
Teal Ribbon: Lung Cancer Awareness
The teal ribbon represents lung cancer awareness. Lung cancer remains a significant global health concern, often associated with smoking. The teal ribbon symbolizes the need for increased public awareness of the risks associated with smoking and the importance of early detection. This color represents a call for prevention strategies and better treatments for this prevalent cancer.
Table of Ribbon Colors and Meanings
| Ribbon Color | Cancer Type | Emotional Message |
|---|---|---|
| Pink | Breast Cancer | Support, resilience, hope, awareness |
| Purple | Ovarian Cancer | Support, awareness, hope, resilience |
| Orange | Childhood Cancer | Support, awareness, hope, advocacy |
| Yellow | Leukemia | Support, awareness, hope, research |
| Teal | Lung Cancer | Awareness, prevention, hope, research |
Global Perspectives on Cancer Ribbons
Cancer ribbons, powerful symbols of solidarity and awareness, transcend geographical boundaries. However, their use and interpretation can vary significantly across different countries and cultures. Understanding these nuances is crucial for effective global cancer awareness campaigns. Different cultural contexts bring different meanings to the same symbol, highlighting the importance of careful consideration when adapting campaigns to specific communities.
Cultural Variations in Ribbon Usage
Different countries and cultures have unique traditions, beliefs, and interpretations of colors and symbols. This leads to diverse approaches to cancer awareness campaigns. For instance, some cultures may attach different meanings to colors associated with ribbons. In some communities, the color pink might not be the primary focus of breast cancer awareness campaigns, as it might not hold the same symbolic value.
This requires a nuanced understanding of the cultural context to develop campaigns that are both effective and respectful.
Adaptation of Cancer Awareness Campaigns
Effective cancer awareness campaigns must adapt to diverse cultural contexts. To ensure inclusivity and impact, campaigns must consider the specific values and beliefs of the target communities. This includes using appropriate language, imagery, and symbols. For example, in some Asian cultures, campaigns might focus on the importance of family support and traditional healing practices in addition to modern medical interventions.
Such adaptations increase the campaign’s reach and impact, ensuring that it resonates with diverse audiences.
Comparison of Ribbon Color Meanings Globally
The symbolism of cancer ribbons varies across cultures. While pink is universally associated with breast cancer awareness, its prominence might differ in specific communities. Similarly, the use of other colors for other types of cancer may not be as consistent. The meanings of colors, particularly in relation to illness and well-being, can be influenced by historical, religious, or social contexts.
For instance, some cultures might associate certain colors with good fortune or healing, potentially affecting the way ribbon colors are perceived.
Visual Representation of Global Ribbon Usage
| Cancer Type | Primary Ribbon Color(s) | Cultural Considerations | Example Campaign Adaptations |
|---|---|---|---|
| Breast Cancer | Pink (most common), but variations exist in some Asian and African cultures. Some cultures might use other colors or patterns with different cultural meanings | In some Asian cultures, there might be a preference for colors associated with good fortune or healing. Consideration of gender roles and societal expectations is crucial. | In some Asian communities, campaigns might focus on the importance of family support and traditional healing practices. |
| Prostate Cancer | Light Purple/Lavender | The specific shade and association with the color might vary across cultures. Consideration of color preferences and symbolism within the community is important. | Some campaigns might incorporate images or symbols that are culturally relevant to the community being targeted. |
| Leukemia | Gold/Yellow | Colors with connotations of hope or joy are used in some cultures. Understanding the nuances of these associations is critical. | In certain cultures, campaigns might use symbols of strength or courage to connect with the audience. |
| Lung Cancer | Light Blue | The significance of light blue might vary depending on the cultural context. It might hold specific meanings in certain communities. | Consideration of cultural traditions and beliefs is crucial in designing campaigns. |
This table provides a basic overview of the potential variations in ribbon usage globally. Further research into specific cultural contexts is necessary for a comprehensive understanding.
Practical Applications and Considerations
The vibrant colors of cancer ribbons serve as powerful symbols of hope, resilience, and support for those affected by cancer. However, the meaningful use of these ribbons requires careful consideration to ensure accurate representation and avoid misinterpretations. Proper application fosters respect and empathy, reinforcing the message of solidarity and awareness.Effective use of cancer ribbons transcends mere decoration; it becomes a powerful tool for raising awareness and fostering community.
This section provides a practical guide on appropriate display and use, emphasizing the importance of accurate representation and avoiding misinterpretations.
Knowing the different colors of cancer ribbons can be a powerful way to show support, but sometimes, understanding your body’s signals is crucial too. For example, a look at your urinalysis results can provide valuable insight into your overall health, as you can see from this helpful resource on what do your urinalysis results mean. Ultimately, whether it’s supporting a cause or understanding your own health, paying attention to the subtle signs can be a great way to take care of yourself and others.
Appropriate Use and Display
The proper display of cancer ribbons is crucial for conveying the intended message effectively. It’s essential to understand the specific meaning behind each color to ensure accurate representation. The placement and context of the ribbon should also align with the message of support and solidarity. Avoid using ribbons in ways that might diminish their significance or lead to misinterpretations.
Accurate Representation of Ribbon Meanings
Maintaining the integrity of cancer ribbon symbolism is paramount. Each ribbon color carries a specific association with a type of cancer or a cause related to cancer. Misrepresenting or misusing a ribbon can lead to confusion and diminish the impact of the message. Careful consideration of the ribbon’s intended meaning is essential to avoid any misinterpretation or misapplication.
Avoiding Misinterpretation of Ribbon Colors
Misinterpreting ribbon colors can inadvertently lead to confusion and misrepresentation of the intended message. For example, using a breast cancer ribbon to symbolize a different type of cancer would dilute the specific message and could be seen as disrespectful to those affected by breast cancer. Understanding the specific cancer type or cause associated with each ribbon color is crucial for appropriate use.
Examples of Appropriate and Inappropriate Uses
Appropriate use of cancer ribbons involves displaying them in a manner that respects their intended meaning. For instance, wearing a breast cancer ribbon during Breast Cancer Awareness Month is a suitable and supportive gesture. Conversely, displaying a childhood cancer ribbon to commemorate a different type of cancer is inappropriate and disrespectful to the specific cause. In summary, it’s essential to use the ribbons accurately to avoid misunderstandings.Inappropriate use, on the other hand, involves misrepresenting the ribbon’s meaning or displaying it in a way that diminishes its significance.
For instance, using a leukemia ribbon as a general cancer awareness ribbon is inappropriate. This diminishes the specific message and risks misrepresenting the cause.
Dos and Don’ts for Using Cancer Ribbons
This table provides a clear guideline for the appropriate use of cancer ribbons, emphasizing the importance of accuracy and respect.
| Dos | Don’ts |
|---|---|
| Wear a breast cancer ribbon during Breast Cancer Awareness Month. | Use a breast cancer ribbon to symbolize a different type of cancer. |
| Display a childhood cancer ribbon in a child’s room to raise awareness. | Use a leukemia ribbon as a general cancer awareness ribbon. |
| Wear a ribbon in support of a friend or family member battling cancer. | Wear multiple ribbon colors without understanding their specific meanings. |
| Support a local charity event by displaying a specific ribbon. | Use a ribbon inappropriately in a commercial context that distorts the meaning. |
| Educate yourself on the meanings of various ribbons. | Wear ribbons in a disrespectful or frivolous manner. |
Beyond the Ribbon
Beyond the vibrant hues of the cancer awareness ribbons, a spectrum of other powerful symbols contribute to the global fight against cancer. These diverse representations, often deeply rooted in culture and personal experience, embody hope, resilience, and the collective spirit of support. They transcend the visual language of ribbons, offering alternative avenues for raising awareness and fostering a sense of community among those affected by cancer.These supplementary symbols serve as reminders of the multifaceted nature of the battle against cancer, encompassing not just the physical disease but also the emotional and psychological challenges faced by patients and their families.
Knowing the different colors of cancer ribbons can be really insightful, right? From pink for breast cancer to purple for lymphoma, each hue tells a story. But sometimes, we need to remember that health challenges come in all forms. For example, understanding the treatment options for conditions like asthma, especially when using albuterol saba inhalers, is crucial.
Learning more about albuterol sabas and asthma can help us better understand the struggles and triumphs of managing these health issues. Ultimately, remembering these different cancer ribbon colors and their meanings reminds us of the diverse battles people face, and the importance of supporting those in need.
The diversity of these symbols underscores the importance of recognizing and valuing the experiences of those directly impacted, while simultaneously uniting individuals in a shared pursuit of knowledge, research, and treatment.
Alternative Symbols in Cancer Awareness
Various symbols, beyond the familiar ribbons, have emerged as powerful tools in cancer awareness campaigns. These symbols frequently represent the journey of cancer patients, the resilience of those affected, or the hope for a brighter future.
Visual Representations of Cancer Awareness Symbols
Different methods of raising awareness extend beyond the traditional ribbon. These methods tap into the creative potential of the community, enabling various expressions of support and unity.
“The fight against cancer is not just about medical advancements; it’s about supporting the community and inspiring hope.”
- Images of flowers and plants: Flowers, especially blooming ones, often symbolize rebirth, resilience, and hope. Their vibrant colors and delicate beauty are a stark contrast to the often challenging reality of cancer, thereby instilling a sense of optimism. Consider a delicate orchid or a sunflower—each a potent symbol of enduring strength.
- Inspirational quotes and slogans: Powerful words can effectively communicate the spirit of resilience and support. Slogans like “We Stand Together” or “Hope is a Powerful Weapon” convey a sense of solidarity and empowerment, often accompanied by compelling imagery that resonates deeply with the audience. Examples of these quotes can be found on banners, posters, and social media posts.
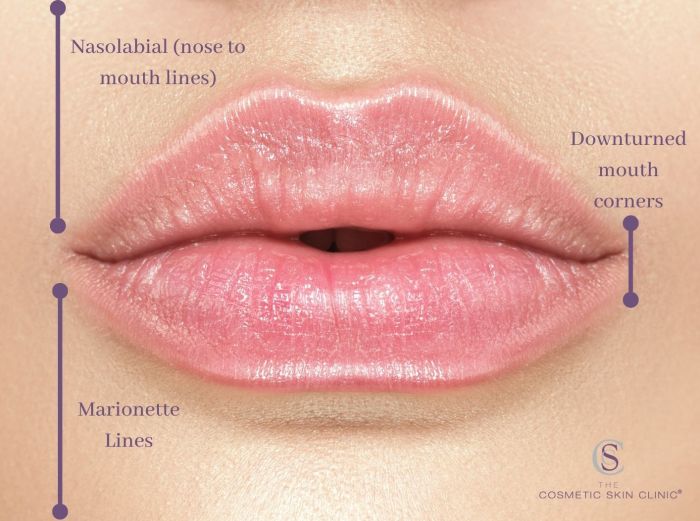
- Educational infographics and illustrations: These tools, often accompanied by clear and concise text, make complex information easily accessible to a wider audience. Infographics can visually explain the different types of cancer, treatment options, and preventative measures. They empower individuals with knowledge and promote proactive steps to address the issue.
- Community events and fundraising initiatives: Organised events, such as walks, runs, or bike rides, create a sense of community and provide tangible support for cancer patients and research efforts. These events, often accompanied by powerful slogans and imagery, offer a platform for collective action and awareness.
- Artistic expressions and memorials: Art, whether in the form of paintings, sculptures, or performances, offers a powerful way to express the emotional impact of cancer. Memorial gardens and public art installations can serve as enduring symbols of remembrance and support.
“Cancer awareness is not limited to ribbons; it’s a multifaceted movement that utilizes diverse symbols and approaches to spread awareness.”
History and Significance of Alternative Symbols
The history and significance of alternative symbols in cancer awareness campaigns often intertwine with cultural traditions and personal experiences. For example, a particular flower may hold special meaning for a community affected by cancer, signifying resilience or hope. Likewise, certain colours or patterns can symbolize the journey through diagnosis, treatment, and recovery. The development of these symbols is a testament to the creative spirit of individuals and communities affected by cancer.
Visual Representations of Cancer Ribbon Information
Cancer ribbons have become powerful symbols of hope, support, and awareness in the fight against cancer. Beyond their symbolic meaning, visual representations play a crucial role in communicating these messages effectively. Infographics, illustrations, and imagery in cancer awareness campaigns can help to raise awareness and inspire action.
Infographic Summary of Cancer Ribbon Meanings
An effective infographic can visually condense the complex meanings of various cancer ribbons into a digestible format. The graphic should use clear, concise language, and visually appealing colors to highlight the significance of each ribbon. A key feature should be a color-coded legend directly associating each ribbon color with the specific type of cancer it represents. The infographic should be easily understandable to a broad audience, including those unfamiliar with the symbolism of cancer ribbons.
Using icons or symbols related to each cancer type could also be helpful for quick comprehension.
Illustrations of Cancer Ribbon Colors and Meanings
Visual aids, such as illustrations, can bring the symbolism of cancer ribbons to life. These illustrations should depict the ribbons in a variety of contexts to emphasize their broad impact.
| Ribbon Color | Cancer Type | Illustration Description |
|---|---|---|
| Pink | Breast Cancer | A vibrant pink ribbon, perhaps tied around a stylized breast or chest area, symbolizing the strength and resilience of those affected by breast cancer. The ribbon could be held by a person or an abstract figure, embodying the collective effort in fighting the disease. |
| Purple | Lymphoma | A rich purple ribbon, elegantly flowing and perhaps wrapped around a stylized lymph node or part of the lymphatic system, emphasizing the complex nature of lymphoma and the support for those undergoing treatment. The illustration might also feature a person or an abstract figure radiating a sense of hope. |
| Light Blue | Prostate Cancer | A gentle light blue ribbon, perhaps entwined with a stylized prostate gland or a person, suggesting the importance of early detection and support for those impacted by prostate cancer. The illustration should convey a sense of calm determination. |
| Orange | Leukemia | A vibrant orange ribbon, perhaps wrapped around a stylized blood cell or a person, symbolizing the fight against leukemia. The illustration should project a sense of strength and the hope for a cure. |
| Yellow | Childhood Cancer | A cheerful yellow ribbon, possibly held by a child or attached to a stylized child’s drawing or toy, highlighting the vulnerability of children affected by cancer and the need for support. The illustration should evoke a sense of compassion and hope for a better future. |
Imagery in Cancer Awareness Campaigns
Imagery is crucial in cancer awareness campaigns. Effective campaigns often utilize compelling visual elements to convey the message of hope, support, and resilience in the face of cancer. For example, photographs of people affected by cancer, or illustrations depicting the various types of cancer, can create a powerful emotional impact and help to raise awareness. The imagery should always be respectful and avoid exploitation or sensationalism.
The goal is to inspire hope and promote a sense of community.
Final Conclusion
In conclusion, cancer ribbons colors meanings extend far beyond their visual appeal. They serve as powerful reminders of the fight against cancer, embodying hope, resilience, and unity. This exploration of their history, symbolism, and global applications underscores their crucial role in raising awareness and supporting those affected by this devastating disease. By understanding the nuances of each color and its associated meaning, we can use these symbols effectively and respectfully in our efforts to combat cancer.