Headache on the right side can be a frustrating and sometimes concerning experience. This comprehensive guide delves into the complexities of right-sided headaches, exploring their diverse types, potential causes, and effective management strategies.
We’ll examine various classifications of these headaches, from tension headaches to migraines, and discuss the nuanced symptoms, pain intensity, and duration associated with each. Understanding the underlying causes, including potential medical conditions and neurological factors, is crucial. We’ll also look at how to differentiate right-sided headaches from other types and when to seek immediate medical attention.
Defining Right-Sided Headaches
Right-sided headaches, while often a symptom of a broader issue, can vary significantly in their causes, characteristics, and treatment. Understanding the nuances of these headaches is crucial for accurate diagnosis and effective management. Pinpointing the specific type of right-sided headache can help guide appropriate medical interventions.Right-sided headaches can be a complex presentation of various underlying conditions. The location of pain on the right side of the head is often a key indicator, but not the sole determinant, of the potential cause.
This localization requires careful evaluation by healthcare professionals to distinguish between benign conditions and more serious ones.
Types of Right-Sided Headaches
Different types of headaches localized to the right side of the head can arise from diverse causes, necessitating a thorough assessment to determine the root cause. These can include tension headaches, migraines, cluster headaches, and others. The symptoms and characteristics often overlap, making diagnosis challenging without a comprehensive medical evaluation.
Classifications of Right-Sided Headaches
Headaches localized to the right side of the head can be categorized based on potential causes. Vascular issues, such as changes in blood flow to the head, may play a role. Muscle tension, triggered by stress, posture, or other factors, is another potential culprit. Neurological conditions, although less common, could also contribute to right-sided headache pain.
Common Characteristics and Symptoms
Right-sided headaches exhibit varying intensities, durations, and accompanying sensations. The pain can range from mild to severe, and the duration can span from a few minutes to several days. Accompanying symptoms might include nausea, vomiting, sensitivity to light or sound, and visual disturbances. The specific symptoms and their intensity can provide clues about the underlying cause.
Nuances in Pain Intensity, Duration, and Accompanying Sensations
The intensity of the pain, its duration, and accompanying symptoms are critical factors in distinguishing different types of right-sided headaches. A sharp, throbbing pain localized to a specific area on the right side, lasting several hours, could suggest a migraine. A persistent, dull ache across the right temple, potentially associated with muscle tension, might indicate a tension headache.
The presence or absence of other symptoms, like aura or sensitivity to light, can significantly aid in proper diagnosis.
Table of Common Right-Sided Headaches
| Headache Type | Symptoms | Possible Causes | Severity |
|---|---|---|---|
| Tension Headache | Dull, aching pain, often described as a band-like tightness around the head; can be on one or both sides; often accompanied by muscle stiffness, fatigue, and stress. | Muscle tension, stress, poor posture, eye strain, dehydration, caffeine withdrawal, or even certain foods. | Mild to Moderate |
| Migraine | Moderate to severe throbbing pain, typically on one side of the head; often accompanied by nausea, vomiting, sensitivity to light and sound, and visual disturbances (aura). | Genetics, hormonal fluctuations, stress, certain foods or drinks, changes in sleep patterns, and environmental factors. | Moderate to Severe |
| Cluster Headache | Severe, piercing pain, usually on one side of the head, often around the eye; can be accompanied by tearing, nasal congestion, and swelling. | Unknown, but likely related to abnormal brain activity, and may have a cyclical pattern. | Severe |
| Secondary Headaches | A wide variety of symptoms depending on the cause, including throbbing pain, pressure, or a stabbing sensation; could be accompanied by fever, stiff neck, or neurological issues. | Underlying medical conditions like sinus infections, brain tumors, or aneurysms. | Variable, depending on the cause. Can be mild to severe. |
Potential Causes of Right-Sided Headaches: Headache On The Right Side
Right-sided headaches, while often benign, can stem from a variety of underlying issues. Understanding the potential causes is crucial for proper diagnosis and treatment. Pinpointing the source allows for targeted interventions and potentially prevents more severe complications. This exploration delves into the medical conditions, neurological factors, vascular concerns, dental problems, and sinus infections that can contribute to right-sided head pain.Right-sided headaches can be a symptom of a multitude of conditions, ranging from common issues like tension headaches to more serious underlying medical problems.
Ever had a headache on the right side that just won’t quit? Sometimes, seemingly simple pain can stem from more complex issues. Conditions like reflex sympathetic dystrophy syndrome RSD, a disorder affecting the nerves and causing chronic pain, what is reflex sympathetic dystrophy syndrome rsd , can sometimes manifest as a persistent right-sided headache. It’s always a good idea to talk to a doctor to rule out any underlying medical conditions, especially if the headache is severe or accompanied by other symptoms.
Identifying the specific cause is essential for effective management.
Neurological Factors in Right-Sided Headaches
Neurological factors play a significant role in headaches, influencing both their frequency and severity. Conditions like migraines, cluster headaches, and tension-type headaches can manifest on one side of the head. While the exact mechanisms aren’t fully understood, nerve irritation, abnormal brain activity, and chemical imbalances are believed to contribute. These factors can be influenced by various triggers, including stress, sleep deprivation, or even specific foods.
Vascular Issues and Right-Sided Headaches
Vascular issues are another important consideration in right-sided headaches. Blood vessel abnormalities or inflammation in the head and neck region can cause pain. Conditions such as temporal arteritis, a form of inflammation in the arteries of the head, can present with severe, throbbing headaches, often localized to one side. Aneurysms, weakened or bulging blood vessels, might also lead to unilateral headaches, particularly if they are situated in the right hemisphere of the brain.
Proper diagnosis and monitoring are critical for managing such situations.
Dental Problems and Right-Sided Headaches
Dental problems can sometimes trigger or exacerbate headaches, particularly on one side. Inflammation or infection in the teeth, jaw joints, or surrounding structures can send pain signals to the head. For instance, a toothache or temporomandibular joint (TMJ) disorder might manifest as a headache localized to the right side of the head, often accompanied by jaw pain or tenderness.
Early identification and treatment of dental issues are important to prevent the headache from persisting.
Sinus Infections and Right-Sided Headaches
Sinus infections, especially if localized to the maxillary sinuses (located on the right side of the face), can cause pain that radiates to the head. Inflammation and pressure within the sinuses can trigger a throbbing or aching sensation, often concentrated on the right side of the head. This pain may be accompanied by nasal congestion, fever, and facial tenderness.
Effective management of sinus infections is essential to alleviate the headache and prevent complications.
Table: Medical Conditions and Right-Sided Headaches
| Medical Condition | Potential Headache Impact | Mechanism | Severity |
|---|---|---|---|
| Sinusitis (Maxillary) | Throbbing or aching pain, often localized to the right side of the head. | Inflammation and pressure within the sinuses. | Moderate to severe, potentially accompanied by fever and nasal congestion. |
| Migraine | Unilateral throbbing pain, often accompanied by nausea and sensitivity to light. | Abnormal brain activity and nerve irritation. | Moderate to severe. |
| Temporal Arteritis | Severe, throbbing headache, localized to one side. | Inflammation of the arteries in the head. | Severe; requires immediate medical attention. |
| TMJ Disorder | Pain in the jaw joint and surrounding areas, sometimes radiating to the right side of the head. | Inflammation or dysfunction of the jaw joint. | Mild to moderate, often accompanied by jaw clicking or popping. |
Differentiating Right-Sided Headaches from Other Types
Understanding the nuances of headaches is crucial for accurate diagnosis and effective treatment. While a headache on the right side of the head might seem simple, distinguishing it from other types of headaches and pinpointing the underlying cause is essential for appropriate medical intervention. This section delves into differentiating characteristics, exploring potential causes, and providing a framework for understanding right-sided headaches.Right-sided headaches, like those located on the left side or the entire head, are a symptom, not a diagnosis.
Precisely defining what constitutes a “right-sided headache” and differentiating it from other forms of cephalalgia requires a comprehensive understanding of its potential triggers, symptoms, and comparison to other types of headaches.
Comparing Right-Sided Headaches with Left-Sided Headaches
Right-sided and left-sided headaches, while often sharing similar symptoms, may have underlying differences in their causes and presentation. A thorough evaluation, considering the patient’s medical history, lifestyle, and specific symptoms, is critical in distinguishing these types of headaches. It is important to note that the location of the pain is often a subjective experience and can vary between individuals.
Differentiating Right-Sided Headaches from General Headaches
A general headache encompasses a wide spectrum of pain sensations, ranging from mild discomfort to severe throbbing. A key aspect of differentiating a right-sided headache from a general headache lies in the specific location of the pain. General headaches can manifest in various areas of the head, whereas a right-sided headache is consistently localized to the right side of the cranium.
Other distinguishing factors may include the intensity, duration, and accompanying symptoms.
Differences in Potential Causes
The potential causes of right-sided headaches can overlap with those of other types of headaches. While many common triggers, such as stress, eye strain, or dehydration, may affect both types of headaches, certain underlying conditions may be more frequently associated with right-sided pain. Further investigation and medical evaluation are necessary to establish a definitive diagnosis.
Distinct Symptoms Differentiating Right-Sided Headaches
While common headache symptoms like throbbing pain, tenderness, and sensitivity to light and sound are present in many types of headaches, certain symptoms might be more pronounced in right-sided headaches. For example, some individuals may experience nausea, vomiting, or a stiff neck alongside the right-sided pain. The specific combination of symptoms provides valuable clues for accurate diagnosis.
Diagnostic Criteria for Right-Sided Headaches
No specific diagnostic criteria solely define a “right-sided headache.” Instead, diagnosis relies on evaluating the presenting symptoms, medical history, and ruling out other potential causes. A thorough examination, including physical assessment, neurological tests, and potentially imaging studies, is essential to determine the underlying cause. This comprehensive approach helps to rule out more serious conditions.
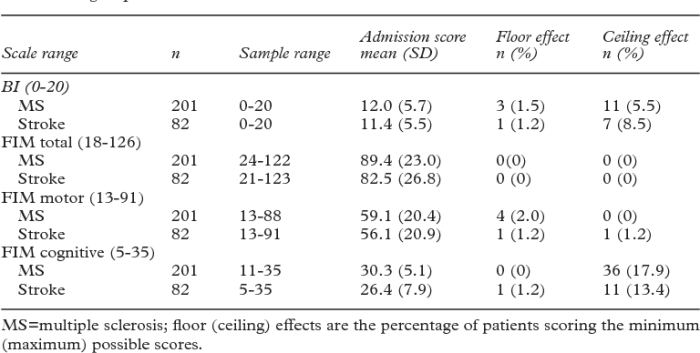
Comparison Table of Right-Sided and Left-Sided Headaches
| Feature | Right-Sided Headache | Left-Sided Headache |
|---|---|---|
| Typical Pain Location | Consistently localized to the right side of the head. | Consistently localized to the left side of the head. |
| Associated Symptoms (Examples) | Nausea, vomiting, stiff neck, sensitivity to light and sound. | Nausea, vomiting, stiff neck, sensitivity to light and sound. |
| Potential Causes (Examples) | Tension, migraine, sinus infections, cluster headaches, medication overuse. | Tension, migraine, sinus infections, cluster headaches, medication overuse. |
Right-Sided Headache Management
Right-sided headaches, while often mirroring general headache characteristics, can stem from various triggers and underlying conditions. Effective management involves a multi-faceted approach targeting the root cause where possible and providing relief from the pain itself. This section delves into strategies for managing right-sided headaches, from simple home remedies to more involved medical interventions.
Home Remedies for Right-Sided Headaches
Home remedies can be valuable initial approaches for managing mild to moderate right-sided headaches. These methods often involve readily available ingredients and techniques.
Ever experienced a headache on the right side? While it can stem from various causes, sometimes it’s surprisingly connected to your oral health. Understanding the nuances of a thorough dental exam, like checking for TMJ issues or impacted teeth, can be key to uncovering the root of the problem. A visit to the dentist, and specifically understanding the dental exam , might reveal a surprising link to that pesky right-sided headache.
It’s always a good idea to explore all possibilities when dealing with persistent headaches.
- Applying a cold compress to the forehead or temples can help constrict blood vessels and reduce inflammation, potentially lessening pain.
- Gentle massage to the temples and surrounding areas can ease muscle tension, a frequent contributor to headaches.
- Rest in a quiet, dark room, avoiding bright lights and loud noises, can allow the body to focus on recovery.
- Staying hydrated by drinking plenty of water can help alleviate dehydration-related headaches.
- Over-the-counter pain relievers, like ibuprofen or acetaminophen, can be effective in reducing pain intensity.
- Certain foods and beverages, such as caffeine, can trigger or worsen headaches, so limiting or avoiding them may prove beneficial.
Over-the-Counter Medications for Right-Sided Headaches
Over-the-counter (OTC) medications are often a first-line defense against right-sided headaches. Their accessibility and generally safe profile make them a convenient option.
- Nonsteroidal anti-inflammatory drugs (NSAIDs), like ibuprofen and naproxen, can effectively reduce inflammation and pain associated with headaches.
- Acetaminophen is another common OTC medication used for pain relief. It works by reducing the production of pain signals in the brain.
- It is crucial to follow dosage instructions carefully and avoid exceeding recommended limits to prevent potential side effects.
- If headaches persist or worsen despite OTC medication use, consulting a healthcare professional is advisable.
Lifestyle Modifications to Prevent Right-Sided Headaches
Adopting healthy lifestyle habits can play a significant role in preventing right-sided headaches. Consistent practices can often reduce the frequency and severity of these headaches.
Ever experienced a headache on the right side? It can be a real pain, literally! Sometimes, unusual symptoms like this can be linked to surprising things, like the side effects of weight loss drugs. Have you been trying different weight loss strategies lately? If so, it’s worth exploring if the acne you’re experiencing might be connected to weight loss drugs acne.
Regardless of the cause, persistent right-sided headaches deserve a visit to your doctor to rule out any underlying health concerns.
- Maintaining a regular sleep schedule can regulate hormone levels and reduce stress, which are common triggers for headaches.
- Adequate hydration is essential for overall health and can prevent dehydration-related headaches.
- Regular exercise, when combined with a balanced diet, can promote overall well-being and reduce the likelihood of various health issues, including headaches.
- Stress management techniques, such as meditation, yoga, or deep breathing exercises, can help mitigate stress-related headaches.
- Identifying and avoiding specific triggers, like certain foods or environmental factors, can be crucial for headache prevention.
Treatment Options Summary
This table summarizes various treatment options for right-sided headaches, highlighting their potential benefits and drawbacks.
| Treatment | Pros | Cons | Effectiveness |
|---|---|---|---|
| Over-the-counter pain relievers (NSAIDs, acetaminophen) | Readily available, relatively inexpensive, effective for mild to moderate pain. | May cause stomach upset, interactions with other medications. | Generally effective, but not for all cases. |
| Cold compress | Simple, non-invasive, often effective for reducing inflammation. | Limited effectiveness for severe pain, potential for discomfort. | Moderate effectiveness, often helpful as a complementary measure. |
| Lifestyle modifications (diet, exercise, stress management) | Long-term preventative measures, improve overall health. | Requires consistent effort, may not immediately alleviate pain. | High potential for long-term prevention and reduced frequency. |
When to Seek Medical Attention

Knowing when to seek medical attention for a right-sided headache is crucial for prompt diagnosis and treatment. Ignoring potentially serious symptoms can delay appropriate care, potentially leading to adverse health outcomes. This section Artikels the situations demanding immediate medical intervention for right-sided headaches.
Critical Situations Requiring Immediate Medical Attention, Headache on the right side
Urgent medical care is necessary for headaches accompanied by alarming symptoms or specific circumstances. These situations necessitate immediate evaluation to rule out life-threatening conditions.
Red Flags for Immediate Medical Intervention
Certain symptoms and circumstances signal the need for immediate medical attention. Ignoring these “red flags” can have serious consequences. Here’s a list of these red flags for right-sided headaches:
- Sudden, severe headache (like a thunderclap headache) that feels significantly worse than previous headaches.
- Headache accompanied by stiff neck, fever, or rash.
- Headache associated with weakness, numbness, or vision changes in one or both sides of the body.
- Headache with a sudden onset of double vision or slurred speech.
- Headache accompanied by seizures or loss of consciousness.
- Headache occurring after a head injury, even a seemingly minor one.
- Headache coupled with severe nausea and vomiting, especially if it’s persistent or worsening.
- Headache accompanied by difficulty speaking or understanding speech.
- Headache that awakens you from sleep.
- Headache accompanied by changes in mental status, such as confusion or disorientation.
New Onset or Severe Headaches
The appearance of a new, severe right-sided headache, or a significant worsening of an existing headache, necessitates immediate medical evaluation. A sudden, severe headache, particularly one that is unlike previous experiences, warrants prompt attention. It is important to remember that pain tolerance varies from person to person. What one person considers a “severe” headache might be different for another.
Symptoms Warranting Urgent Medical Evaluation
The presence of certain symptoms accompanying a right-sided headache underscores the importance of immediate medical attention. These symptoms can indicate serious underlying conditions.
- Sudden, severe pain, described as a “thunderclap” headache, that is significantly worse than previous headaches.
- Headache accompanied by neurological symptoms, such as numbness, weakness, or vision changes.
- Headache with a high fever (above 100.4°F or 38°C) or stiff neck.
- Headache that develops suddenly after a head injury, even a seemingly minor one.
- Headache accompanied by a stiff neck.
- Headache with seizures or loss of consciousness.
Circumstances Requiring Immediate Professional Care
Specific circumstances surrounding a right-sided headache demand immediate professional care. These situations highlight the potential for serious underlying conditions requiring prompt diagnosis and treatment.
- Headache occurring in conjunction with a recent head injury, even if it seems minor.
- Headache occurring after a significant trauma or accident.
- Headache accompanied by a fever or stiff neck.
- Headache that is accompanied by neurological symptoms, such as numbness, weakness, or vision changes.
- Headache that is significantly worsening or increasing in frequency.
Closing Notes
In conclusion, understanding right-sided headaches involves recognizing the variety of potential causes and symptoms. Proper diagnosis and treatment require a comprehensive approach, considering both medical conditions and lifestyle factors. By equipping yourself with the knowledge presented here, you can better navigate this often-debilitating experience and take proactive steps toward effective management.