Bronchioles anatomy function and diseases are a fascinating subject, delving into the intricate structures within our lungs. These tiny airways play a critical role in respiration, and their health significantly impacts our overall well-being. This exploration will unravel the complexities of their structure, function, and the diseases that can affect them, providing a comprehensive overview for a deeper understanding.
From the branching patterns and histological differences to the mechanisms of gas exchange and disease processes, this comprehensive guide will equip you with a clearer picture of bronchiolar health. We’ll explore common disorders and their associated symptoms, treatment options, and even delve into the fascinating world of imaging techniques for diagnosis.
Bronchioles
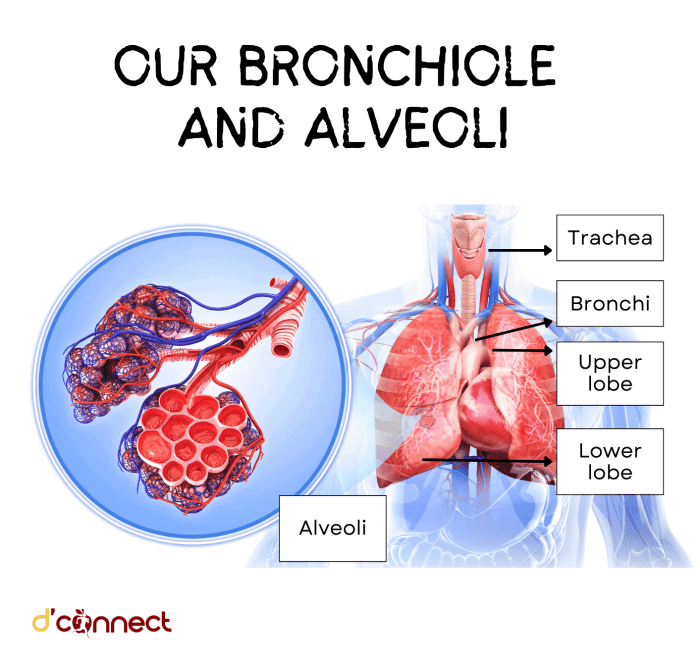
Bronchioles are the smallest branches of the respiratory tree, connecting the larger bronchi to the alveoli, the tiny air sacs where gas exchange occurs. Understanding their structure and function is crucial for comprehending how the respiratory system facilitates breathing and oxygen uptake. Their delicate architecture and specialized histology are essential components of healthy pulmonary function.The bronchioles’ intricate branching pattern and unique histological characteristics are critical for effective air distribution and gas exchange throughout the lungs.
Understanding the intricate anatomy and function of bronchioles is crucial for comprehending lung health. These tiny air passages, branching off from the larger bronchi, play a vital role in gas exchange. Unfortunately, various diseases can affect their structure and function, impacting overall respiratory health. Considering the importance of supporting healthy lung function, exploring potential supplements like those available at supplements for lung health might be beneficial for those looking to improve their respiratory well-being.
However, it’s essential to remember that these supplements shouldn’t replace proper medical care and that consulting a healthcare professional before starting any new supplement regimen is crucial for managing any potential underlying bronchiolar diseases.
This detailed exploration delves into the structural features and histological differences between the various types of bronchioles, illuminating their significance in respiration.
Bronchiolar Structure and Branching Patterns
Bronchioles exhibit a characteristic branching pattern, progressively decreasing in diameter as they approach the alveoli. This branching ensures that inhaled air reaches all parts of the lungs efficiently. The branching structure resembles an inverted tree, with the larger bronchi forming the trunk and the bronchioles forming the numerous branches. The progressively smaller diameters are essential for maintaining a high surface area for gas exchange.
Different bronchioles have different diameters and branching patterns, allowing for efficient airflow and optimal gas exchange.
Histological Differences between Terminal and Respiratory Bronchioles
Terminal bronchioles represent the final segment of the conducting zone, where air movement occurs but gas exchange does not. Respiratory bronchioles, on the other hand, are the first segment of the respiratory zone, where gas exchange begins. The key histological difference lies in the presence of alveoli budding off the respiratory bronchioles. Terminal bronchioles have a simple cuboidal epithelium with cilia and lack alveoli, while respiratory bronchioles have a similar epithelium but exhibit alveoli opening directly onto their walls.
Components of the Bronchiolar Wall
The bronchiolar wall is composed of three primary layers: epithelium, smooth muscle, and connective tissue. The epithelium, the innermost layer, undergoes a significant transition as the bronchioles become smaller. Smooth muscle plays a vital role in regulating airflow by constricting or dilating the bronchioles. The connective tissue, the outermost layer, provides structural support to the bronchiolar wall. The presence and thickness of these components vary among different types of bronchioles.
Epithelial Lining Changes
As you move from larger bronchi to terminal bronchioles, the epithelial lining undergoes significant changes. In larger bronchi, the epithelium is pseudostratified columnar with goblet cells and cilia. As the bronchioles become smaller, the epithelium transitions to simple columnar and eventually to simple cuboidal, with a reduction in goblet cells and cilia. This transition reflects the decreasing need for mucus secretion and mucociliary clearance as the primary function shifts to gas exchange.
Bronchioles, the tiny air passages in our lungs, are crucial for gas exchange. Their intricate anatomy and function are essential for healthy breathing. However, various diseases can affect these delicate structures, causing significant respiratory issues. Interestingly, some research suggests a potential link between respiratory problems and autoimmune conditions like hypothyroidism and rheumatoid arthritis. This connection warrants further study, as understanding the potential interplay between these conditions could lead to improved treatments and management strategies.
Ultimately, a deeper understanding of bronchioles anatomy, function, and diseases is vital for effective respiratory care. hypothyroidism and rheumatoid arthritis link
Comparison of Bronchioles and Bronchi
| Feature | Bronchi | Bronchioles |
|---|---|---|
| Epithelium | Pseudostratified columnar with goblet cells and cilia | Simple cuboidal to simple columnar, with few or no goblet cells and cilia |
| Smooth Muscle | Present, but less prominent | Present, prominent and highly developed, crucial for bronchoconstriction and bronchodilation |
| Cartilage | Present, forming C-shaped cartilage rings | Absent |
| Glands | Present, mucous glands | Absent |
| Elastic Fibers | Present | Present |
| Function | Airway conduction | Airway conduction and initial site of gas exchange |
Bronchiolar Function
Bronchioles, the smallest airways in the lungs, play a critical role in pulmonary ventilation. They are the final conduits for air before it reaches the alveoli, the sites of gas exchange. Understanding their function is essential for comprehending how the respiratory system works. This section delves into the intricate mechanisms of bronchiolar function, examining the roles of smooth muscle, secretions, and epithelium in maintaining healthy respiration.
Role in Pulmonary Ventilation, Bronchioles anatomy function and diseases
Bronchioles are responsible for the final stages of air movement into the alveoli. Their structure and function are adapted to facilitate efficient gas exchange. The bronchiolar tree’s extensive branching maximizes the surface area available for gas exchange with the alveoli.
Bronchiolar Smooth Muscle Regulation of Airflow
Bronchiolar smooth muscle plays a crucial role in regulating airflow. This smooth muscle layer encircles the bronchioles and can contract or relax, adjusting the diameter of the airways. This control over bronchiolar diameter is essential for adjusting airflow based on the body’s needs, for instance during exercise or in response to stimuli like allergens. Constriction of the smooth muscle, often mediated by neurotransmitters or inflammatory mediators, reduces airflow, a key feature in asthma and other respiratory conditions.
Significance of Bronchiolar Secretions
Bronchiolar secretions, including mucus and surfactant, are vital for maintaining lung health. Mucus traps foreign particles and pathogens, preventing them from reaching the alveoli. Surfactant, a complex mixture of lipids and proteins, reduces surface tension within the alveoli, preventing their collapse during exhalation. Imbalances in these secretions can contribute to respiratory issues.
Function of the Bronchiolar Epithelium in Gas Exchange
The bronchiolar epithelium, a single layer of cells lining the bronchioles, is critical for gas exchange. Specialized cells within this epithelium facilitate the movement of oxygen and carbon dioxide between the air in the bronchioles and the surrounding capillaries. The delicate structure of the epithelium, with its close proximity to capillaries, optimizes the efficiency of gas exchange.
Mechanisms of Bronchiolar Clearance
Bronchiolar clearance mechanisms remove foreign particles and mucus from the airways. Cilia, hair-like projections on the epithelial cells, beat in a coordinated manner, moving mucus and trapped debris towards the pharynx for expectoration. This process is crucial for preventing the accumulation of secretions and maintaining a clear airway.
Table of Bronchiolar Component Functions
| Component | Function |
|---|---|
| Smooth Muscle | Regulates airflow by constricting or dilating bronchioles |
| Mucus | Traps foreign particles and pathogens |
| Surfactant | Reduces surface tension in alveoli, preventing collapse |
| Epithelium | Facilitates gas exchange between air and blood |
| Cilia | Moves mucus and debris towards the pharynx |
Diseases Affecting Bronchioles
Bronchioles, the smallest airways in the lungs, are vital for gas exchange. However, various diseases can affect their structure and function, leading to respiratory distress and other complications. Understanding these diseases is crucial for accurate diagnosis and effective treatment.Bronchiolar diseases encompass a spectrum of conditions, ranging from acute infections to chronic obstructive conditions. The underlying causes, symptoms, and treatments can vary significantly, making a precise diagnosis and personalized treatment approach essential.
Pathological changes, ranging from inflammation to structural damage, are key to comprehending these diseases.
Common Bronchiolar Diseases
Bronchiolar diseases affect the structure and function of the bronchioles, often leading to inflammation, narrowing, or obstruction of the airways. This can significantly impair gas exchange, resulting in respiratory symptoms.
Bronchioles, those tiny air passages in our lungs, are crucial for gas exchange. Their delicate structure and function are vital for breathing. However, various diseases can affect their anatomy and impair respiratory function. For instance, asthma and bronchitis often involve bronchiole inflammation. Wondering if preventative measures like the HPV vaccine are useful even if you’ve already been exposed?
Check out this helpful resource to understand the efficacy of the HPV vaccine for those already infected: does hpv vaccine help if already infected. Ultimately, understanding bronchiole anatomy, function, and the diseases that impact them is key to maintaining good respiratory health.
Asthma
Asthma is a chronic inflammatory disorder of the airways, including the bronchioles. It is characterized by intermittent episodes of wheezing, shortness of breath, chest tightness, and coughing, particularly at night or in the early morning. Pathologically, asthma involves bronchospasm, edema, and mucus hypersecretion in the bronchiolar walls. Diagnosis often involves a detailed medical history, physical examination, and pulmonary function tests.
Treatment focuses on managing inflammation and bronchospasm using inhaled corticosteroids, bronchodilators, and leukotriene modifiers.
Bronchiolitis
Bronchiolitis is an acute inflammatory condition, primarily affecting infants and young children. It’s typically caused by viral infections, most commonly respiratory syncytial virus (RSV). Symptoms include rapid breathing, wheezing, coughing, and a runny nose. Pathologically, bronchiolitis is characterized by inflammation and edema of the bronchiolar walls, leading to airway narrowing. Diagnosis relies on clinical presentation and often involves chest X-rays or pulse oximetry.
Treatment primarily focuses on supportive care, including hydration, supplemental oxygen, and monitoring for complications.
Bronchiectasis
Bronchiectasis is a chronic progressive disease characterized by abnormal widening and scarring of the bronchi and bronchioles. It’s often associated with recurrent infections, cystic fibrosis, or other underlying conditions. Symptoms include chronic cough with sputum production, shortness of breath, and recurrent respiratory infections. Pathologically, bronchiectasis results in permanent dilation and destruction of the bronchial walls. Diagnosis often involves chest X-rays, high-resolution computed tomography (HRCT) scans, and sputum cultures.
Treatment involves managing infections with antibiotics, bronchodilators, and postural drainage.
Bronchiolitis Obliterans
Bronchiolitis obliterans, also known as BO, is a chronic obstructive lung disease characterized by the obliteration (blocking) of the bronchioles. It often develops after an initial lung injury, such as a viral infection or a transplantation. Symptoms include progressive dyspnea (difficulty breathing), cough, and fatigue. Pathologically, BO involves the fibrosis and narrowing of the bronchioles, leading to impaired airflow.
Diagnosis involves detailed medical history, pulmonary function tests, and HRCT scans. Treatment options are often limited and may include immunosuppressive therapies or lung transplantation in severe cases.
Table of Common Bronchiolar Diseases
| Disease | Cause | Symptoms | Treatment |
|---|---|---|---|
| Asthma | Chronic inflammation of airways | Wheezing, shortness of breath, chest tightness, coughing | Inhaled corticosteroids, bronchodilators, leukotriene modifiers |
| Bronchiolitis | Viral infections (e.g., RSV) | Rapid breathing, wheezing, coughing, runny nose | Supportive care (hydration, oxygen) |
| Bronchiectasis | Recurrent infections, cystic fibrosis | Chronic cough with sputum, shortness of breath, recurrent infections | Antibiotics, bronchodilators, postural drainage |
| Bronchiolitis Obliterans | Lung injury (viral, transplant) | Progressive dyspnea, cough, fatigue | Immunosuppressive therapies, lung transplantation (severe cases) |
Bronchiolar Disorders: Bronchioles Anatomy Function And Diseases
Bronchioles, the smallest airways in the lungs, play a crucial role in gas exchange. Disruptions to their function can lead to a range of respiratory conditions, impacting individuals across various demographics. Understanding the pathophysiology, clinical presentations, and management strategies for bronchiolar disorders is vital for effective diagnosis and treatment.
Asthma Pathophysiology and Bronchiolar Function
Asthma is a chronic inflammatory disorder characterized by airway hyperresponsiveness and bronchospasm. In asthma, the bronchiolar smooth muscle contracts, narrowing the airways and obstructing airflow. This constriction is often triggered by allergens, irritants, or exercise. Inflammation of the bronchiolar lining also plays a significant role. Inflammatory cells release mediators that further contribute to bronchoconstriction and airway remodeling, leading to long-term structural changes that worsen airflow limitations.
The inflammatory process in asthma is multifaceted, involving various immune cells and mediators. Bronchiolar hyperresponsiveness is a hallmark of asthma, where the airways react excessively to stimuli.
Bronchiolar Inflammation in COPD
Chronic Obstructive Pulmonary Disease (COPD) is a progressive lung disease characterized by chronic inflammation and airflow limitation. Bronchiolar inflammation is a key component of COPD’s pathophysiology. The inflammatory response in COPD involves chronic exposure to noxious stimuli, such as cigarette smoke. This leads to an accumulation of inflammatory cells in the bronchiolar walls. The inflammation causes damage to the bronchiolar structures, impairing their function and leading to irreversible airflow obstruction.
The inflammation is characterized by the infiltration of neutrophils, macrophages, and lymphocytes into the bronchiolar walls. This inflammatory process is a major contributor to the progressive decline in lung function observed in COPD.
Bronchiolitis Obliterans Mechanisms
Bronchiolitis obliterans is a chronic lung disease characterized by the scarring and obliteration (closure) of the bronchioles. This condition can develop after various lung injuries or conditions. Mechanisms behind bronchiolitis obliterans are varied and complex. In some cases, it arises as a complication of a previous lung infection or transplant rejection. In other instances, it may result from exposure to toxic substances.
The underlying process often involves an immune-mediated response to the injury, leading to the proliferation of fibroblasts and the formation of scar tissue within the bronchiolar walls. The scarring ultimately obstructs airflow, leading to progressive respiratory failure. A key aspect is the development of fibrosis, where excessive connective tissue forms, obstructing the bronchioles.
Clinical Presentations of Bronchiolar Diseases in Different Populations
The clinical presentations of bronchiolar diseases can vary across different populations due to factors such as age, underlying health conditions, and environmental exposures. Infants and children may present with acute wheezing and respiratory distress, while adults may exhibit chronic cough, shortness of breath, and progressive dyspnea. Individuals with pre-existing respiratory conditions or weakened immune systems may be more susceptible to bronchiolar diseases.
Furthermore, environmental factors like exposure to pollutants can influence the severity and presentation of these conditions.
Case Studies Illustrating Bronchiolar Diseases
Case studies are valuable in demonstrating the diagnosis and management of bronchiolar diseases. A case study of a young child with recurrent wheezing episodes could lead to a diagnosis of asthma, with appropriate management involving inhaled corticosteroids and bronchodilators. Similarly, a case of a middle-aged smoker with progressive dyspnea and cough may suggest COPD, requiring smoking cessation and pulmonary rehabilitation.
Specific management strategies may involve targeted therapies for the specific disease presentation.
Diagnostic Criteria for Bronchiolar Diseases
| Disease | Diagnostic Criteria |
|---|---|
| Asthma | History of recurrent wheezing, shortness of breath, chest tightness, and cough; reversible airflow obstruction; positive response to bronchodilators. |
| COPD | History of exposure to noxious stimuli (e.g., cigarette smoke); chronic cough, sputum production, shortness of breath; airflow limitation that is not fully reversible; radiographic evidence of emphysema or chronic bronchitis. |
| Bronchiolitis Obliterans | Progressive dyspnea, cough, and wheezing; evidence of bronchiolar narrowing and obliteration on imaging studies; exclusion of other potential causes. |
Imaging of Bronchioles
![Arbre bronchique [Anatomie] - fiches-anatomie.com Bronchioles anatomy function and diseases](https://lyricapills.com/wp-content/uploads/2025/06/schema_arbre_bronchique-1.png)
Visualizing the intricate network of bronchioles, the tiny air passages within the lungs, is crucial for diagnosing and monitoring respiratory diseases. While direct visualization of bronchioles is challenging, various imaging techniques offer valuable insights into their structure and function. These techniques are essential for assessing the impact of diseases on these crucial components of the respiratory system.Imaging plays a critical role in understanding the subtle changes within the bronchioles that often precede or accompany more overt symptoms.
By identifying specific patterns and abnormalities, radiologists and pulmonologists can formulate more precise diagnoses and develop targeted treatment plans.
Bronchoscopy
Bronchoscopy is a direct visualization technique where a flexible or rigid tube with a camera is inserted into the airways. This allows for detailed examination of the bronchi and bronchioles, facilitating the identification of abnormalities such as inflammation, narrowing, or tumors. It is particularly useful for obtaining biopsies and collecting samples for further analysis. However, bronchoscopy can be invasive, carries risks such as bleeding and infection, and may not provide a comprehensive view of the entire bronchiolar network.
High-Resolution Computed Tomography (HRCT)
HRCT is a powerful imaging modality that provides detailed cross-sectional views of the lungs. It excels at revealing subtle changes in the bronchiolar walls, such as thickening or inflammation, which might be missed by other techniques. HRCT’s high resolution allows for the visualization of bronchiolar abnormalities, and its ability to distinguish between different tissues makes it a valuable tool for diagnosing conditions like bronchiolitis obliterans.
While HRCT is excellent for visualizing the bronchioles, it might not directly assess their functional capacity, and the procedure involves exposure to ionizing radiation.
Magnetic Resonance Imaging (MRI)
MRI, although not as commonly used for evaluating bronchioles as HRCT, can provide valuable information in certain situations. MRI can be particularly useful for assessing the presence of edema or fluid accumulation within the bronchioles. Its ability to visualize soft tissues makes it potentially useful for distinguishing different types of inflammation and identifying specific pathologies. MRI’s lack of ionizing radiation is a significant advantage, however, its image quality for assessing bronchioles may not be as sharp as that obtained with HRCT, and the process can take longer.
Ventilation-Perfusion (VQ) Scanning
VQ scans are functional imaging techniques that evaluate the distribution of ventilation (air flow) and perfusion (blood flow) in the lungs. This technique is crucial for identifying regional ventilation-perfusion mismatches, a hallmark of many bronchiolar diseases. By analyzing the ventilation and perfusion patterns, clinicians can determine if there are areas of the lung where air flow or blood flow is impaired, which is often a result of bronchiolar dysfunction.
VQ scans do not directly visualize the bronchioles themselves, but they provide vital functional information.
Image Interpretation in Bronchiolar Disorders
Interpreting imaging findings in bronchiolar disorders requires careful consideration of the specific clinical presentation and other diagnostic data. For instance, a patient with chronic cough and dyspnea accompanied by HRCT findings of bronchiolar wall thickening may suggest a diagnosis of chronic bronchiolitis. Detailed analysis of the location, extent, and pattern of abnormalities is essential for accurate diagnosis and guiding treatment strategies.
Radiologists and pulmonologists often use a combination of imaging techniques and clinical information to establish a comprehensive understanding of the disease.
Figure: Typical Bronchiolar Appearance on Imaging

Bronchiolar Development and Growth
Bronchiolar development is a critical process in lung maturation, shaping the intricate network of airways that facilitate gas exchange. Understanding the stages of this development, the factors influencing it, and potential consequences of disruptions is essential for comprehending respiratory health, particularly in infants and children. This intricate process is influenced by a complex interplay of genetic and environmental factors.Bronchiolar development proceeds through distinct phases, each characterized by specific structural and functional changes.
The intricate process begins during fetal life and continues into postnatal life, culminating in the fully developed lung structure required for efficient respiration. Factors like genetics, nutrition, and exposure to environmental stimuli significantly impact this development. A comprehensive understanding of these factors and their interplay is crucial for preventing respiratory complications later in life.
Stages of Bronchiolar Development
Bronchiolar development is a dynamic process, progressing from simple structures to complex airways. Early stages involve the formation of primordial structures, followed by branching and differentiation into specific cell types. The process continues after birth, with further refinement of the airways and their supportive tissues.
- Fetal Stage (Prenatal): The initial stages of bronchiolar development are marked by the formation of the lung buds, which grow and divide into smaller branches. The branching pattern is crucial for creating a vast network of airways. This phase is particularly sensitive to environmental influences, as the developing lungs are susceptible to factors like infection and malnutrition. These environmental exposures can disrupt the normal progression of bronchiolar development and lead to long-term lung dysfunction.
- Postnatal Stage (Early Childhood): Following birth, the bronchiolar structure continues to mature. The airways further branch and differentiate, and the supporting tissues, including smooth muscle and connective tissue, develop. This process is essential for optimizing lung function. Growth and development continue throughout childhood, allowing the lungs to adapt to changing needs. Factors like respiratory infections can affect the postnatal stage of bronchiolar development.
Factors Influencing Bronchiolar Growth and Maturation
Numerous factors contribute to the proper development and maturation of bronchioles. These factors can either promote or hinder the process, impacting the overall lung function.
- Genetic Factors: Specific genes play a crucial role in directing the differentiation and growth of bronchiolar cells. Mutations or variations in these genes can lead to developmental abnormalities. The influence of genetic factors on bronchiolar development is multifaceted, with genes regulating cell proliferation, migration, and differentiation.
- Environmental Factors: Environmental exposures, including infections, pollutants, and nutritional deficiencies, can significantly impact bronchiolar development. Maternal health during pregnancy and early childhood experiences are crucial determinants. Exposure to various environmental factors can have detrimental effects on lung development, particularly in early life.
- Hormonal Factors: Hormones play a role in regulating the growth and differentiation of bronchiolar cells. Hormonal imbalances can disrupt the normal developmental process, leading to potential lung abnormalities. Hormonal influences are particularly relevant during the prenatal and postnatal periods.
Comparison of Bronchiolar Development Across Species
The process of bronchiolar development varies across different species, reflecting adaptations to specific environmental and physiological demands.
| Species | Developmental Characteristics |
|---|---|
| Humans | Characterized by a complex branching pattern, with a significant postnatal period of maturation. |
| Mice | Display a relatively rapid development compared to humans, with a more straightforward branching pattern. |
| Dogs | Have a developmental trajectory similar to humans, although the specific timing and rates may differ. |
Consequences of Abnormal Bronchiolar Development
Abnormal bronchiolar development can result in a range of respiratory disorders, impacting lung function and overall health. These consequences can vary in severity and can have profound impacts on the individual.
- Respiratory Disorders: Abnormal bronchiolar development can contribute to conditions like bronchopulmonary dysplasia, cystic fibrosis, and asthma. These conditions are often associated with impaired lung function and can lead to significant health challenges.
- Reduced Lung Function: Individuals with abnormal bronchiolar development may experience reduced lung capacity and airflow limitations, affecting their ability to perform daily activities. These consequences can impact the individual’s quality of life.
Role of Specific Genes in Bronchiolar Development
Specific genes play a crucial role in directing the intricate process of bronchiolar development. Disruptions in these genes can have profound effects on lung function.
- Transcription Factors: Transcription factors regulate the expression of other genes involved in bronchiolar development. Mutations in these genes can disrupt the normal developmental pathway, potentially leading to respiratory complications. Transcription factors act as crucial regulators of bronchiolar development, orchestrating the expression of genes that control the process.
End of Discussion
In conclusion, understanding bronchioles anatomy function and diseases is vital for comprehending the intricate workings of the respiratory system. We’ve explored the structural nuances, the functional roles, and the various pathologies that can impact these crucial airways. By grasping the intricate interplay of these elements, we gain a deeper appreciation for the complexity and resilience of our respiratory health.
This knowledge is essential for informed decision-making and a greater understanding of our own bodies.










