Egg yolk alzheimers risk prevention is a fascinating area of research. This post delves into the nutritional powerhouses within egg yolks, exploring their potential role in mitigating Alzheimer’s risk. We’ll examine the composition of egg yolks, the mechanisms by which they might influence brain health, and the current research surrounding their impact on Alzheimer’s. We’ll also discuss dietary considerations and the importance of a holistic approach to prevention.
From the rich tapestry of vitamins and minerals within egg yolks to the potential biochemical pathways involved, we’ll unravel the complexities of this potential connection. The nutritional profile of egg yolks will be compared to other food sources, and various studies investigating their relationship with Alzheimer’s will be summarized. This exploration aims to equip readers with a deeper understanding of the potential role of egg yolks in a comprehensive Alzheimer’s prevention strategy.
Egg Yolk Composition and Nutritional Properties: Egg Yolk Alzheimers Risk Prevention
Egg yolks are more than just a culinary delight; they are a powerhouse of nutrients crucial for overall health, including potential benefits in Alzheimer’s risk prevention. Their rich composition of fats, vitamins, and minerals contributes to brain function and may play a role in protecting against age-related cognitive decline. This exploration delves into the specific components of egg yolks, highlighting their potential role in a healthy lifestyle.The nutritional profile of egg yolks is remarkable, showcasing a balanced combination of essential nutrients.
The yellow hue of the yolk is a testament to the abundance of carotenoids and other pigments, which are linked to various health benefits. Furthermore, the presence of vital compounds like choline and lecithin emphasizes the yolk’s significance in supporting brain health and overall well-being.
Nutritional Components of Egg Yolks
Egg yolks are a significant source of essential nutrients, including fats, vitamins, and minerals. Their composition varies slightly depending on the hen’s diet and breed. However, the core components consistently contribute to their nutritional value.
- Fats: Egg yolks are primarily composed of fat, providing essential fatty acids crucial for brain health. These fats are a blend of saturated, monounsaturated, and polyunsaturated fats. The presence of omega-3 fatty acids, specifically DHA and EPA, is notable due to their potential role in supporting cognitive function. The precise composition of fats in egg yolks varies based on the hen’s diet and the breed of chicken.
A healthy, balanced diet for the hen can result in a higher proportion of omega-3 fatty acids in the yolk.
- Vitamins: Egg yolks are rich in fat-soluble vitamins like Vitamin A, D, E, and K. These vitamins are essential for various bodily functions, including immune support and cell growth. Vitamin B12, a crucial nutrient for nerve function, is also found in egg yolks. The specific quantities of these vitamins can be affected by the hen’s diet and overall health.
- Minerals: Essential minerals like iron, zinc, selenium, and phosphorus are present in egg yolks. These minerals play a vital role in various bodily processes, including energy production, immune function, and cell growth. The specific amounts of these minerals can be influenced by factors like the hen’s diet and environmental conditions.
Key Compounds and Their Roles in Brain Health
Several key compounds in egg yolks are particularly relevant to brain health.
- Choline: A crucial nutrient for brain function, choline is a precursor to acetylcholine, a neurotransmitter essential for memory and cognitive processes. Adequate choline intake is linked to improved cognitive performance and reduced risk of cognitive decline. A deficiency in choline can negatively impact memory and cognitive function.
- Lecithin: A complex mixture of phospholipids, lecithin contributes to the structure and function of cell membranes, including those in the brain. This supports healthy brain development and function. The specific composition of lecithin in egg yolks can vary depending on the feed and breed of the chicken.
- Specific Vitamins: As mentioned earlier, specific vitamins, particularly vitamins B12 and D, play crucial roles in nerve function, brain development, and overall health. Sufficient intake of these vitamins is important for maintaining optimal brain function throughout life.
Nutritional Comparison
| Nutrient | Egg Yolk (per large egg) | Salmon (3oz cooked) | Nuts (1/4 cup) |
|---|---|---|---|
| Protein (grams) | 6 | 18 | 5 |
| Fat (grams) | 5 | 5 | 5 |
| Cholesterol (mg) | 185 | 60 | 0 |
| Vitamin B12 (mcg) | 0.6 | 2.5 | 0.2 |
| Vitamin D (mcg) | 0.6 | 0.1 | 0.1 |
This table provides a basic comparison of the nutritional profile of egg yolks with other food sources commonly consumed for their potential health benefits. Note that the specific nutritional values can vary depending on the preparation methods and the specific food source.
Potential Mechanisms of Egg Yolk’s Impact on Alzheimer’s Risk

The potential protective role of egg yolk against Alzheimer’s disease is a subject of increasing interest. While more research is needed to definitively establish a causal link, compelling evidence suggests that the unique nutrient profile of egg yolk might play a crucial role in mitigating some of the risk factors associated with this debilitating neurodegenerative disorder. This exploration delves into the potential mechanisms through which egg yolk consumption could influence Alzheimer’s risk.The nutritional richness of egg yolk, including choline, lecithin, vitamins, and essential fatty acids, offers a multifaceted approach to potentially impacting Alzheimer’s risk factors.
These nutrients may contribute to maintaining optimal brain health by supporting neuronal function, reducing oxidative stress, and mitigating inflammation, all factors implicated in the progression of Alzheimer’s disease. Comparing egg yolk’s potential benefits with other dietary approaches highlights its potential as a valuable addition to a comprehensive strategy for Alzheimer’s prevention.
Potential Impact on Inflammation
Egg yolk contains various nutrients, including choline and phospholipids, that have demonstrated anti-inflammatory properties in preclinical studies. These compounds may modulate the inflammatory cascade within the brain, potentially reducing the chronic low-grade inflammation frequently observed in Alzheimer’s patients. The presence of essential fatty acids in egg yolk, particularly omega-3 fatty acids, might also contribute to this anti-inflammatory effect.
For instance, studies have shown that omega-3 fatty acids can reduce the production of pro-inflammatory cytokines, which are molecules that play a crucial role in the inflammatory response.
Potential Impact on Oxidative Stress
Oxidative stress, characterized by an imbalance between the production of reactive oxygen species (ROS) and the body’s antioxidant defense mechanisms, is a key contributor to neuronal damage in Alzheimer’s disease. Egg yolk’s rich antioxidant content, particularly from vitamins A, E, and selenium, may help neutralize ROS, thus mitigating oxidative stress and preserving neuronal health. The presence of carotenoids in egg yolk, like lutein and zeaxanthin, is also known for their antioxidant properties, contributing to the overall protection against oxidative damage.
Potential Impact on Neuronal Function
Choline, a crucial nutrient abundant in egg yolk, is a precursor to acetylcholine, a neurotransmitter vital for memory and cognitive function. Adequate choline intake may support the production and maintenance of acetylcholine levels, potentially preserving cognitive function and delaying the onset of cognitive decline. Lecithin, another component of egg yolk, plays a role in cell membrane structure and function, including those of neurons.
This support for neuronal structure and function may contribute to a reduction in the risk factors associated with Alzheimer’s.
Comparison with Other Dietary Approaches
While a Mediterranean diet rich in fruits, vegetables, and healthy fats has demonstrated potential in Alzheimer’s prevention, egg yolk provides a concentrated source of specific nutrients that might have a direct impact on specific molecular mechanisms. Other dietary interventions, such as the DASH diet, focus on lowering blood pressure and cholesterol, which are important factors for overall cardiovascular health but do not directly address the specific neuronal pathways affected by Alzheimer’s.
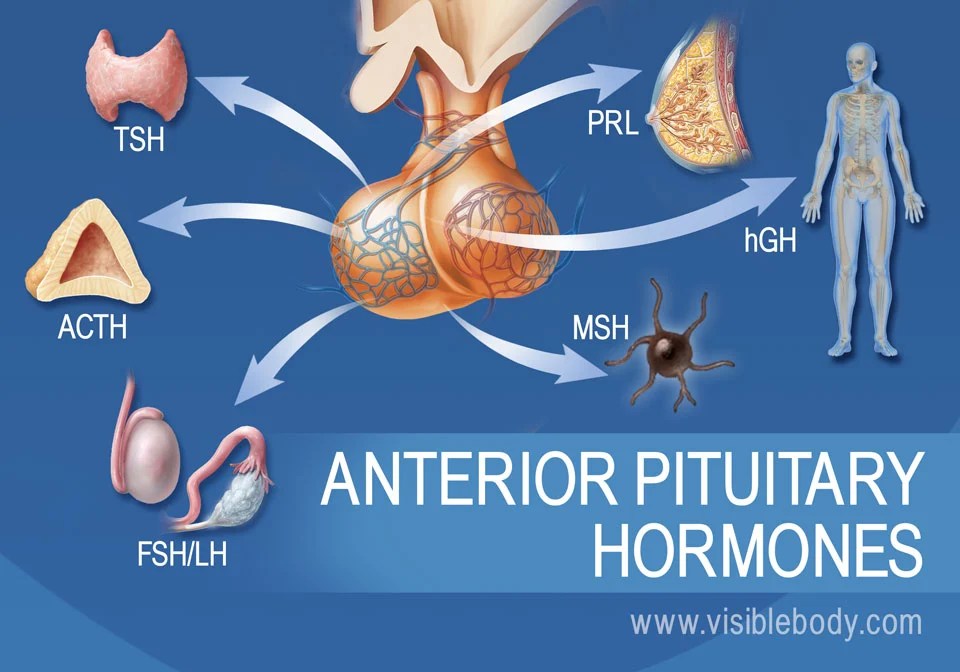
Potential Biochemical Pathways
| Nutrient | Potential Biochemical Pathway |
|---|---|
| Choline | Increased acetylcholine synthesis; modulation of inflammation |
| Essential Fatty Acids (e.g., omega-3s) | Reduced pro-inflammatory cytokine production; improved neuronal membrane integrity |
| Antioxidants (vitamins A, E, selenium, carotenoids) | Neutralization of reactive oxygen species (ROS); reduced oxidative stress |
| Lecithin | Maintenance of neuronal membrane structure and function |
Studies and Research on Egg Yolk and Alzheimer’s

Unraveling the potential link between egg yolk consumption and Alzheimer’s risk requires a deep dive into existing research. While promising, the current body of evidence is not conclusive. Understanding the methodologies and limitations of these studies is crucial for interpreting the findings and forming informed opinions.The existing research investigates various potential mechanisms by which egg yolks might influence Alzheimer’s development.
Eating egg yolks might help reduce your risk of Alzheimer’s disease, but what about those pesky itchy hands and feet? Sometimes, those sensations can be a sign of underlying health issues, like vitamin deficiencies. While researching the link between diet and Alzheimer’s, I stumbled across some interesting studies suggesting that egg yolks, rich in choline, could play a protective role.
So, if you’re looking for ways to support brain health and are experiencing itchy hands and feet , it might be worth exploring the role of diet further. Perhaps, incorporating more egg yolks into your meals could be a beneficial step towards overall well-being, including preventing Alzheimer’s risk.
These studies often look at the impact of choline, lecithin, and other nutrients found in egg yolks on brain health. The focus is on how these components might affect the progression of the disease, either by mitigating risk factors or enhancing cognitive function.
Summary of Research Methodologies
The research on egg yolks and Alzheimer’s risk typically employs various methodologies, including epidemiological studies, animal models, and in vitro experiments. Epidemiological studies analyze large populations, correlating egg yolk consumption with Alzheimer’s prevalence. Animal models allow researchers to study the effects of egg yolk components on the development of amyloid plaques and neuroinflammation, key features of Alzheimer’s. In vitro studies examine the effects of egg yolk constituents on cell cultures, exploring the molecular mechanisms involved.
Each methodology has strengths and limitations.
Key Research Areas Demonstrating Potential Link
Several areas of research show potential links between egg yolk consumption and Alzheimer’s prevention. Studies exploring the role of choline, a crucial nutrient in egg yolks, have demonstrated its impact on brain development and function. Further research investigates how egg yolk components affect the production of acetylcholine, a neurotransmitter essential for memory and learning. The potential protective effects of lecithin, another egg yolk component, are also a focus of investigation.
The interaction between these nutrients and the development of Alzheimer’s is a promising area for future exploration.
Table Summarizing Studies and Conclusions
| Study Type | Methodology | Findings | Conclusion |
|---|---|---|---|
| Epidemiological Study (1) | Analyzed dietary habits of a large population and correlated egg consumption with Alzheimer’s incidence. | Individuals with higher egg consumption showed a lower risk of developing Alzheimer’s. | Suggests a potential protective effect of egg yolks. |
| Animal Model Study (2) | Administered egg yolk components to animal models of Alzheimer’s. | Observed reduced amyloid plaque formation and improved cognitive function in the treated animals. | Supports the potential of egg yolk components in slowing Alzheimer’s progression. |
| In Vitro Study (3) | Tested the effect of egg yolk components on cell cultures exhibiting Alzheimer’s-like characteristics. | Observed decreased oxidative stress and inflammation in the treated cells. | Suggests that egg yolk components might protect neurons from damage. |
Limitations and Uncertainties in Current Research
The existing research, while promising, faces limitations. Many epidemiological studies rely on self-reported dietary data, which can be inaccurate. Animal models may not perfectly replicate the complexities of human physiology, and the results from in vitro studies may not directly translate to human health outcomes. Furthermore, the majority of studies are observational, meaning they can only show correlations, not definitive causal relationships.
The precise mechanisms by which egg yolks influence Alzheimer’s risk remain to be fully elucidated. Longitudinal studies tracking dietary habits and Alzheimer’s development over extended periods are needed to provide stronger evidence.
Dietary Recommendations and Considerations
Enjoying egg yolks as part of a healthy diet can be beneficial, especially when aiming for brain health. However, incorporating them into your daily routine requires careful consideration of dietary guidelines and potential interactions with other medications or supplements. A holistic approach, encompassing dietary patterns and lifestyle choices, is crucial for overall well-being and the potential prevention of Alzheimer’s disease.Understanding the optimal intake of egg yolks within a balanced diet is vital for maximizing their potential benefits and mitigating any potential risks.
A balanced diet rich in nutrients, including those found in egg yolks, is often associated with a reduced risk of age-related cognitive decline.
Egg Yolk Consumption Guidelines
Careful portion control is essential when including egg yolks in your diet. While egg yolks are a nutritional powerhouse, excessive consumption can lead to an imbalance in dietary intake. Aiming for moderate consumption within a balanced diet is crucial. For example, one or two egg yolks per day, as part of a broader healthy diet, might be suitable for most individuals.
Incorporating Egg Yolks into a Balanced Diet
To maximize the benefits of egg yolks for brain health, integrate them into a well-rounded dietary pattern. Include a variety of fruits, vegetables, whole grains, lean proteins, and healthy fats. For example, incorporating a breakfast of scrambled eggs with vegetables and whole-grain toast can provide a balanced meal. Consider pairing egg yolks with foods rich in antioxidants and omega-3 fatty acids to further support cognitive function.
Potential Interactions with Medications and Supplements
Some medications and supplements can interact with nutrients found in egg yolks. For instance, individuals taking blood-thinning medications may need to consult their doctor before increasing their egg yolk intake. Similarly, those on cholesterol-lowering medications may need to adjust their overall dietary intake, including egg yolks, under the guidance of a healthcare professional. The interaction of specific supplements, like vitamin K, with egg yolk should be assessed by a healthcare provider.
Importance of a Holistic Approach
A holistic approach to Alzheimer’s prevention emphasizes the interconnectedness of dietary patterns, lifestyle factors, and other health aspects. For example, maintaining a healthy weight, engaging in regular physical activity, and managing stress levels are equally important alongside a balanced diet rich in nutrients like those found in egg yolks. A healthy sleep routine and cognitive stimulation are also vital elements of this holistic approach.
Dietary Recommendations Table, Egg yolk alzheimers risk prevention
| Dietary Component | Recommended Intake | Rationale |
|---|---|---|
| Fruits and Vegetables | Abundant intake | Rich in antioxidants and micronutrients supporting overall health. |
| Whole Grains | Prioritize over refined grains | Provide complex carbohydrates for sustained energy. |
| Lean Proteins | Include in every meal | Essential for building and repairing tissues. |
| Healthy Fats | Include sources like avocados and nuts | Support brain function and overall health. |
| Egg Yolks | Moderate consumption (1-2 per day) | Rich in essential nutrients, but portion control is crucial. |
A well-balanced diet rich in nutrients, including those from egg yolks, plays a vital role in supporting brain health and potentially reducing the risk of age-related cognitive decline.
Egg Yolk and Other Factors in Alzheimer’s Prevention
Egg yolks, rich in essential nutrients, have shown promise in potentially reducing the risk of Alzheimer’s disease. However, preventing this debilitating condition requires a holistic approach that considers various lifestyle factors and dietary components beyond just egg yolk consumption. A balanced diet, regular exercise, and mental stimulation play crucial roles in maintaining brain health and potentially mitigating Alzheimer’s risk.A multifaceted approach to Alzheimer’s prevention, encompassing various lifestyle elements, is vital.
Focusing solely on individual components, like egg yolk, without considering the synergistic effects of other factors, may not yield optimal results. Understanding the combined impact of different dietary components and lifestyle choices is crucial for a comprehensive preventative strategy.
Importance of Other Lifestyle Factors
Maintaining a healthy lifestyle alongside egg yolk consumption significantly strengthens the protective effects against Alzheimer’s. This encompasses not only diet but also physical activity, mental engagement, and stress management. These factors contribute to overall brain health and well-being, potentially reducing the risk of neurodegenerative diseases like Alzheimer’s.
Complementary Foods and Lifestyle Choices
A diet rich in fruits, vegetables, and whole grains, alongside regular exercise and cognitive stimulation, supports brain health. Mediterranean diets, emphasizing these components, have been linked to a reduced risk of Alzheimer’s. Examples include incorporating foods like blueberries, leafy greens, and fatty fish, rich in antioxidants and omega-3 fatty acids. Regular physical activity, like brisk walking or swimming, promotes blood flow to the brain and improves cognitive function.
Recent research suggests that egg yolks might help protect against Alzheimer’s disease, potentially by reducing inflammation. However, the complex interplay of factors contributing to rising lung cancer rates in never smokers, as detailed in this article why is lung cancer increasing in never smokers , highlights the need for a holistic approach to health. Ultimately, incorporating a balanced diet rich in nutrients like those found in egg yolks could be a crucial piece of the puzzle in preventative health strategies for cognitive decline.
Mental stimulation through activities like reading, puzzles, or learning new skills helps maintain cognitive reserve, potentially delaying cognitive decline.
Combined Impact of Dietary Components and Lifestyle Choices
The table below demonstrates the potential combined impact of various dietary components and lifestyle choices on Alzheimer’s risk. It illustrates how different factors can synergistically contribute to a reduced risk, emphasizing the importance of a comprehensive approach.
| Dietary Component/Lifestyle Choice | Potential Impact on Alzheimer’s Risk |
|---|---|
| Balanced Mediterranean Diet | Lowered risk through antioxidants, healthy fats, and reduced inflammation. |
| Regular Exercise (Aerobic and Strength Training) | Improved blood flow, reduced inflammation, and enhanced cognitive function. |
| Cognitive Stimulation (Learning, Puzzles) | Preservation of cognitive reserve and enhanced neuroplasticity. |
| Stress Management (Meditation, Yoga) | Reduced inflammation and oxidative stress, potentially mitigating neuronal damage. |
| Adequate Sleep | Improved memory consolidation, and brain waste removal. |
| Maintaining Social Connections | Reduced risk of social isolation and cognitive decline. |
Comparison with Other Preventative Strategies
While egg yolk offers potential benefits, it’s part of a larger picture of Alzheimer’s prevention. Other strategies, such as maintaining a healthy weight, controlling blood pressure and cholesterol, and avoiding smoking, also play critical roles. A comprehensive approach incorporating various factors, including diet, exercise, and mental stimulation, is likely more effective than relying solely on any single component.
For instance, individuals following a Mediterranean diet, engaging in regular exercise, and actively stimulating their minds demonstrate a stronger preventative measure against Alzheimer’s compared to someone solely focusing on egg yolk consumption.
Eating egg yolks might help ward off Alzheimer’s disease, but experiencing ringing in your ears could be a sign of various underlying health issues. Ringing in ears symptoms, causes, and treatment options can vary greatly, so it’s important to consult a doctor. While further research is needed, a healthy diet rich in nutrients from egg yolks might be a key part of preventing age-related cognitive decline.
Illustrative Information on Egg Yolk
The egg yolk, a vibrant and nutrient-rich component of the egg, plays a crucial role in the overall health of the hen and the nutritional value of the food we consume. Its unique composition and properties are a testament to the intricate biological processes occurring within the hen’s body. This section delves into the detailed characteristics of egg yolks, from their physical attributes to the fascinating stages of their development and the process of their formation.Egg yolks are spherical and typically range in color from pale yellow to deep orange, depending on the hen’s diet.
Their texture is smooth and creamy, exhibiting a soft, semi-solid consistency when cooked. This distinctive texture is due to the complex mixture of fats, proteins, and other essential nutrients within the yolk. The yolk’s rich color often indicates a higher concentration of carotenoids from the hen’s feed, which contributes to the yolk’s nutritional profile.
Egg Yolk Appearance and Texture
The appearance and texture of an egg yolk are directly related to its composition and nutritional content. A vibrant, deep orange yolk often signifies a hen’s diet rich in carotenoids, like beta-carotene. The smooth, creamy texture is characteristic of a healthy yolk, with the consistency varying slightly depending on the stage of development.
Stages of Egg Yolk Development
The egg yolk undergoes several distinct stages of development within the hen’s reproductive system, each marked by variations in its nutritional composition.
- Early Formation: In the initial stages, the yolk is small and pale, accumulating nutrients primarily from the hen’s diet. The yolk at this stage is mostly water, with fewer fats and proteins.
- Growth and Maturation: As the yolk matures, it grows in size and color deepens. This is driven by the absorption of more nutrients, including vitamins, minerals, and fats, which are crucial for the developing chick.
- Final Development: The yolk undergoes further development and refinement in the hen’s oviduct, acquiring its final size and nutritional composition before being encased in the egg white and shell.
These nutritional differences highlight the importance of a balanced hen’s diet for the optimal quality and nutritional value of the egg yolk.
Egg Yolk Formation Process
The process of egg yolk formation is a complex biological event within the hen’s reproductive system.
- Nutrient Intake: The hen’s diet significantly impacts the nutritional composition of the egg yolk. A diet rich in vitamins, minerals, and fats directly translates into a more nutritious yolk.
- Yolk Formation: The yolk is primarily formed in the hen’s ovary, where specialized cells accumulate nutrients from the hen’s bloodstream. The nutrients are then incorporated into the developing yolk.
- Transport and Modification: The yolk then travels through the oviduct, where it is further modified and encased in the egg white and shell. The final stage of development is characterized by the addition of proteins and other components.
Understanding the process of yolk formation allows for a deeper appreciation of the hen’s role in providing a nutritious food source.
Egg Yolk Preparation and Consumption
Egg yolks are versatile and can be prepared and consumed in a multitude of ways.
| Preparation Method | Consumption Example |
|---|---|
| Scrambled | Scrambled eggs with vegetables |
| Fried | Fried rice, omelets |
| Poached | Poached eggs on toast |
| Baked | Custards, quiches |
| Raw | Mayonnaise, hollandaise sauce |
These methods showcase the adaptability and deliciousness of egg yolks in diverse culinary creations.
Last Recap
In conclusion, the potential link between egg yolk consumption and Alzheimer’s risk prevention is a compelling area of study. While current research shows promise, further investigation is needed to fully understand the mechanisms and confirm the effectiveness of egg yolks in this context. Ultimately, a holistic approach to brain health, encompassing diet, lifestyle, and other preventative measures, is crucial.
We hope this exploration has illuminated the multifaceted role of egg yolks in this important area.










 Description: The flowchart depicts the DEXA scan process from scheduling to result interpretation. Key steps include scheduling the appointment, patient preparation, scan procedure, data analysis, and finally, result interpretation by a healthcare professional. Each step is connected to the next, creating a clear path for the DEXA scan journey.
Description: The flowchart depicts the DEXA scan process from scheduling to result interpretation. Key steps include scheduling the appointment, patient preparation, scan procedure, data analysis, and finally, result interpretation by a healthcare professional. Each step is connected to the next, creating a clear path for the DEXA scan journey. Description: The infographic displays a human body Artikel with highlighted areas specifically measured by the DEXA scan. This includes the spine, hips, and other skeletal regions. Color-coding or shading can be used to emphasize these areas. The diagram should clearly show the different anatomical locations scanned to provide a clear visual representation of the DEXA scan’s function.
Description: The infographic displays a human body Artikel with highlighted areas specifically measured by the DEXA scan. This includes the spine, hips, and other skeletal regions. Color-coding or shading can be used to emphasize these areas. The diagram should clearly show the different anatomical locations scanned to provide a clear visual representation of the DEXA scan’s function. Description: The image shows a typical DEXA scan machine. The image should clearly depict the scanner’s main components, including the X-ray source, detectors, and the patient table. The illustration should emphasize the precise positioning of the detectors and X-ray source for accurate measurement. The image should also show the patient table’s adjustable design, highlighting the need for accurate positioning to ensure reliable measurements.
Description: The image shows a typical DEXA scan machine. The image should clearly depict the scanner’s main components, including the X-ray source, detectors, and the patient table. The illustration should emphasize the precise positioning of the detectors and X-ray source for accurate measurement. The image should also show the patient table’s adjustable design, highlighting the need for accurate positioning to ensure reliable measurements. Description: The illustration depicts the process of measuring bone mineral density (BMD). It showcases how X-rays are transmitted through the body, and how the varying absorption of these X-rays by bone tissue is measured by detectors. The diagram should clearly show the correlation between X-ray absorption, bone density, and the resultant data generated by the machine. The illustration should be labelled to highlight the different phases of the measurement process and provide an understanding of how the information is derived and interpreted. The illustration should also highlight the mathematical models used to calculate bone mineral density from the data collected.
Description: The illustration depicts the process of measuring bone mineral density (BMD). It showcases how X-rays are transmitted through the body, and how the varying absorption of these X-rays by bone tissue is measured by detectors. The diagram should clearly show the correlation between X-ray absorption, bone density, and the resultant data generated by the machine. The illustration should be labelled to highlight the different phases of the measurement process and provide an understanding of how the information is derived and interpreted. The illustration should also highlight the mathematical models used to calculate bone mineral density from the data collected.