Restless legs syndrome physical exercise is a powerful tool for managing the discomfort and disruption this condition can bring. Understanding the connection between movement and symptom relief is key to finding effective strategies. This guide delves into the potential benefits of various exercise types, offering practical recommendations for incorporating physical activity into a daily routine, while addressing potential challenges and considerations specific to RLS.
From understanding the science behind exercise and RLS symptom alleviation to exploring specific exercises and routines tailored to different needs, this comprehensive resource provides valuable insights and practical advice. We’ll also examine the crucial relationship between exercise, sleep, and RLS, highlighting the importance of creating a holistic approach to managing the condition.
Understanding Restless Legs Syndrome (RLS)
Restless legs syndrome (RLS), a neurological disorder, is characterized by an irresistible urge to move the legs, often accompanied by unpleasant sensations. This urge is typically worse at rest, particularly in the evening or at night, and is frequently relieved by movement. Understanding RLS involves recognizing its symptoms, potential causes, and impact on daily life.RLS is a chronic condition that can significantly impact sleep quality and overall well-being.
Symptoms frequently worsen over time if left unmanaged, leading to fatigue, daytime sleepiness, and difficulties concentrating. This can, in turn, impact personal and professional life, affecting relationships and work performance.
Symptoms and Characteristics of RLS
RLS is defined by the persistent urge to move the legs, often accompanied by unpleasant sensations, such as tingling, crawling, itching, or burning. These sensations are frequently described as uncomfortable and are typically worse at rest, particularly in the evening or at night. The urge to move the legs is often so strong that it interferes with sleep, causing wakefulness and impacting overall well-being.
Causes and Risk Factors of RLS
The precise cause of RLS remains unknown, but several factors are linked to its development. Genetic predisposition is a significant risk factor, as RLS often runs in families. Certain medical conditions, such as iron deficiency, kidney failure, and diabetes, can increase the likelihood of developing RLS. Pregnancy, particularly in the third trimester, can also trigger or exacerbate RLS symptoms.
Furthermore, certain medications, such as anti-nausea drugs and antidepressants, can potentially induce or worsen RLS.
Progression and Impact of RLS
The progression of RLS can vary significantly from person to person. Some individuals experience mild symptoms that only occur occasionally, while others experience more severe symptoms that interfere substantially with their daily lives. The impact of RLS can be substantial, affecting sleep quality, leading to fatigue and daytime sleepiness. This can hinder concentration, impacting work performance, and potentially leading to social isolation.
In some cases, RLS can negatively affect relationships due to the sleep disruption and associated fatigue.
Finding the right physical exercise routine for restless legs syndrome can be tricky, but it’s definitely worth the effort. One thing to consider, especially if you experience heavy menstrual periods, is potential iron deficiency anemia, which can exacerbate restless legs symptoms. Checking out the link on heavy menstrual periods iron deficiency anemia could offer valuable insight into how these two issues are connected.
Ultimately, a tailored exercise plan that accounts for potential underlying conditions, like iron deficiency, will help manage restless legs syndrome more effectively.
Comparison with Other Neurological Conditions
| Characteristic | RLS | Parkinson’s Disease | Multiple Sclerosis |
|---|---|---|---|
| Symptoms | Urge to move legs, unpleasant sensations (tingling, crawling) | Tremors, rigidity, bradykinesia (slow movement) | Muscle weakness, numbness, vision problems, cognitive changes |
| Cause | Unknown; genetic predisposition, medical conditions | Progressive degeneration of nerve cells | Autoimmune response damaging the myelin sheath |
| Impact on Daily Life | Sleep disturbance, fatigue, daytime sleepiness, possible social isolation | Difficulty with daily tasks, balance problems, potential speech difficulties | Varying degrees of disability depending on the affected areas |
Potential Triggers for RLS Episodes
Several factors can trigger or worsen RLS symptoms. These include:
- Iron Deficiency: Low iron levels in the blood are strongly associated with RLS. Individuals with low iron levels often experience worsening symptoms, particularly at night. Iron supplements can help alleviate symptoms.
- Stress and Fatigue: Stressful situations and feelings of tiredness can exacerbate RLS symptoms. Managing stress levels and ensuring adequate rest can help minimize these effects.
- Certain Medications: Some medications, such as anti-nausea drugs, antidepressants, and some anti-psychotics, can induce or worsen RLS symptoms. Consulting a physician about alternative medications or adjusting dosages may be necessary.
- Caffeine and Nicotine: Stimulants such as caffeine and nicotine can increase RLS symptoms. Reducing intake or avoiding these substances may be helpful.
- Alcohol Consumption: Alcohol consumption, especially in large quantities, can contribute to worsening RLS symptoms.
- Changes in Temperature: Sudden changes in temperature can also trigger RLS episodes, particularly if the individual is in a cold environment. Maintaining a consistent temperature, especially in the bedroom, can help.
Physical Exercise and RLS
Physical exercise can play a crucial role in managing restless legs syndrome (RLS) symptoms. While there’s no cure for RLS, regular physical activity can often reduce the intensity and frequency of uncomfortable sensations, leading to improved sleep and overall well-being. This approach is often a complementary therapy, working alongside other treatments.Engaging in regular physical activity offers numerous benefits for individuals with RLS.
These benefits extend beyond simply reducing symptoms, encompassing improvements in mood, energy levels, and sleep quality. Understanding the types of exercise, the mechanisms behind their effectiveness, and the importance of consulting a healthcare professional is key to a successful approach.
Potential Benefits of Physical Exercise for RLS
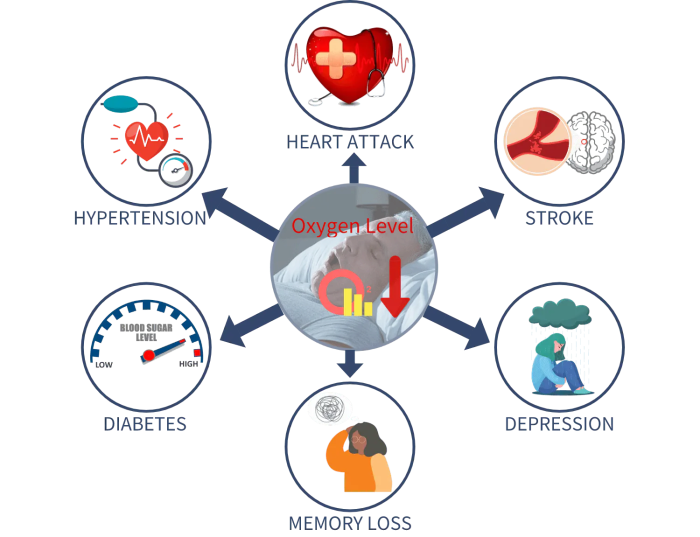
Regular physical activity can significantly impact RLS symptoms. Studies suggest that exercise can reduce the urge to move, improve sleep quality, and enhance mood. The positive effects are often attributed to improved blood circulation, reduced muscle tension, and the release of endorphins. Exercise also helps regulate the body’s natural sleep-wake cycle, contributing to better sleep, which can lessen RLS symptoms.
Types of Exercise Beneficial for RLS Management
A variety of exercises can be beneficial in managing RLS symptoms. Aerobic exercises, such as brisk walking, jogging, swimming, or cycling, are often recommended due to their positive impact on overall health and blood circulation. Strength training exercises, including weightlifting or resistance band workouts, can also contribute to symptom relief by strengthening muscles and improving overall body function.
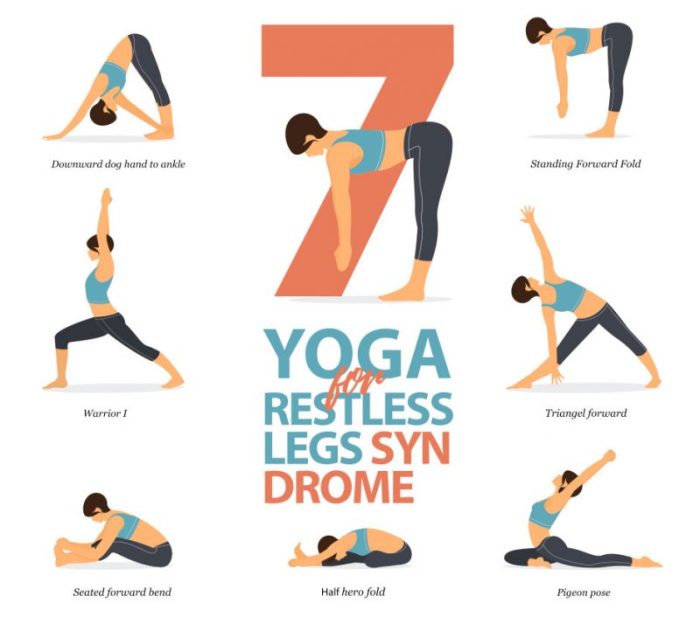
Yoga and tai chi, with their emphasis on stretching and mindfulness, can be particularly helpful in reducing muscle tension and promoting relaxation.
Mechanisms of Exercise in Alleviating RLS Symptoms
Exercise is believed to alleviate RLS symptoms through several mechanisms. Increased blood flow, improved circulation, and reduced muscle tension are among the key benefits. Exercise can also help regulate the body’s natural sleep-wake cycle, which is often disrupted in individuals with RLS. The release of endorphins, natural mood boosters, is another important factor.
Importance of Consulting a Healthcare Professional
Before initiating any new exercise regimen, especially if you have RLS, it’s crucial to consult with a healthcare professional. They can assess your individual needs and medical history to determine the most suitable exercises and intensity levels. They can also help you identify any potential health concerns or pre-existing conditions that may influence your exercise routine. This personalized approach is vital to ensure safety and effectiveness.
Comparison of Exercise Types and RLS Symptoms
Different types of exercise may have varying effects on RLS symptoms. Cardiovascular exercise, such as running or cycling, can significantly improve overall health and circulation, potentially reducing the urge to move. Strength training, while beneficial for overall muscle strength and tone, may not have as pronounced an impact on the urge to move in the short term. Yoga and tai chi, due to their focus on stretching and relaxation, may be particularly effective in reducing muscle tension and promoting relaxation, thus easing RLS symptoms.
Ultimately, a personalized approach tailored to individual needs is essential.
Recommended Exercise Routines for RLS
| Exercise Type | Description | Frequency Recommendation | Intensity Recommendation |
|---|---|---|---|
| Brisk Walking | Walking at a pace that elevates your heart rate | 3-5 times per week | Moderate intensity |
| Swimming | Swimming laps or participating in water aerobics | 2-3 times per week | Moderate to vigorous intensity |
| Yoga | Practicing yoga poses focusing on stretching and relaxation | 2-3 times per week | Gentle to moderate intensity |
| Strength Training | Lifting weights or using resistance bands | 2-3 times per week | Moderate intensity |
This table provides examples of exercise routines that might be suitable for managing RLS symptoms. It’s essential to remember that these are just examples, and the best routine will depend on individual circumstances. Consult a healthcare professional to tailor an exercise plan to your specific needs and health status.
Exercise Recommendations for RLS Management
Finding the right exercise routine can significantly improve restless legs syndrome (RLS) symptoms and overall well-being. Understanding your body’s response to different activities is key to a successful strategy. This involves not just choosing the right type of exercise, but also learning to listen to your body’s signals and adjust your approach accordingly.Exercise offers a multifaceted approach to RLS management.
Beyond physical benefits, it can positively influence sleep quality, mood, and overall energy levels, all of which can be affected by RLS. This often translates to a more fulfilling and productive daily life.
Incorporating Exercise into a Daily Routine
A consistent exercise routine is crucial for managing RLS. Begin with activities you enjoy and gradually increase the intensity and duration as your body adapts. Finding a balance between challenging your body and allowing for rest is vital.
Finding the right physical exercise for restless legs syndrome can be tricky. While some find that gentle activities like swimming or yoga help, others find high-impact workouts more beneficial. It’s all about finding what works for you. In fact, sometimes lifestyle changes, like understanding how to delay your period how to delay your period , can influence the symptoms.
Ultimately, regular, appropriate exercise can be a game-changer in managing restless legs syndrome.
- Start slowly. Begin with short, low-impact exercises, such as walking, swimming, or stationary cycling. Gradually increase the duration and intensity over several weeks.
- Consistency is key. Aim for regular exercise sessions, ideally most days of the week, to see improvements in RLS symptoms.
- Variety is important. Include a mix of cardio and strength training exercises to maintain overall fitness and target different muscle groups.
Adjusting Exercise Intensity and Duration
Adapting your exercise routine to your individual needs and RLS symptoms is crucial. Listen carefully to your body’s signals and adjust accordingly.
- Pay attention to warning signs. Symptoms like increased leg discomfort, fatigue, or muscle soreness can indicate that the intensity or duration of your exercise needs adjustment.
- Modify intensity and duration as needed. If you experience discomfort, reduce the intensity or duration of the exercise. Take rest breaks as necessary.
- Listen to your body. Don’t push yourself too hard, especially during the early stages of an exercise program. Gradually increase the intensity and duration as your body adapts.
Importance of Listening to the Body
Recognizing and responding to your body’s signals is essential for managing RLS symptoms effectively. This includes understanding potential warning signs and adjusting your exercise routine accordingly.
- Recognize warning signs. Pay attention to any changes in your RLS symptoms, such as increased leg discomfort, fatigue, or muscle soreness.
- Modify your exercise plan. If you experience these warning signs, reduce the intensity or duration of your exercise. Consider taking a break or switching to a less demanding activity.
- Prioritize rest. Rest and recovery are just as important as exercise. Adequate rest allows your body to repair and rebuild muscle tissue.
Potential Role of Exercise in Improving Sleep Quality, Restless legs syndrome physical exercise
Regular exercise can significantly improve sleep quality for RLS patients. Exercise promotes better sleep by improving mood, reducing stress, and increasing energy levels.
- Improved sleep quality. Exercise can promote better sleep by reducing stress, improving mood, and regulating energy levels.
- Reduced stress and anxiety. Exercise is a natural stress reliever and can help reduce anxiety, which can often contribute to RLS.
- Increased energy levels. Regular exercise can improve energy levels, which can be particularly beneficial for individuals experiencing fatigue associated with RLS.
Sample Exercise Plan for RLS Management
This sample plan provides a structured approach to exercise, incorporating rest periods. Adjust the plan based on your individual needs and tolerance levels.
| Day | Activity | Duration (minutes) | Intensity | Rest (minutes) |
|---|---|---|---|---|
| Monday | Walking | 20 | Moderate | 5 |
| Tuesday | Swimming | 30 | Moderate | 10 |
| Wednesday | Rest | – | – | – |
| Thursday | Yoga | 30 | Light | 5 |
| Friday | Cycling | 25 | Moderate | 5 |
| Saturday | Light Hiking | 45 | Moderate | 10 |
| Sunday | Rest | – | – | – |
Strategies to Incorporate Exercise into a Daily Routine Effectively
Making exercise a regular part of your life requires strategic planning.
- Schedule exercise. Treat exercise appointments like any other important meeting.
- Find an exercise buddy. Having a workout partner can increase motivation and accountability.
- Make it enjoyable. Choose activities you genuinely enjoy to enhance adherence to your exercise routine.
Exercise Considerations for RLS Patients

Finding the right exercise routine can be challenging when living with restless legs syndrome (RLS). The unpredictable nature of RLS symptoms can make it difficult to maintain a consistent exercise program. However, regular physical activity can significantly improve RLS symptoms and overall well-being. Understanding the specific challenges and tailoring exercise strategies are key to successful management.Exercise can be a powerful tool for managing RLS, but it’s crucial to approach it with sensitivity and understanding of the condition’s impact.
Symptoms like the urge to move, discomfort, and pain can make it hard to stick to a routine. This section delves into practical considerations for RLS patients, emphasizing strategies for overcoming obstacles and building sustainable exercise habits.
Potential Challenges and Obstacles to Exercise
RLS symptoms can significantly interfere with exercise. The constant urge to move and the accompanying discomfort can make it difficult to focus on and complete a workout. Additionally, fatigue associated with RLS can make it hard to find the energy for physical activity. Sleep disturbances, another common symptom, can also hinder exercise adherence.
Finding the right physical exercise for restless legs syndrome can be tricky, and unfortunately, sometimes your health insurance might not cover the related treatments or therapies. Understanding why your health insurance won’t pay for these things is crucial, and that’s why I’ve included a helpful resource for you to learn more: why your health insurance wont pay for your health care.
Ultimately, though, consistent, gentle exercise, like walking or stretching, can be very effective in managing the symptoms of restless legs syndrome, and it’s definitely worth exploring those options.
Addressing Specific Concerns Related to Exercise and RLS Symptoms
Managing RLS symptoms during exercise requires a proactive approach. Understanding the triggers for RLS symptoms is crucial. Some individuals may find that certain times of day or specific activities exacerbate symptoms. For instance, exercising at night when RLS is most intense might not be ideal. Finding alternative times or modifying activities can be helpful.
Importance of Finding an Enjoyable and Sustainable Exercise Routine
Choosing activities that are both enjoyable and sustainable is paramount. Exercise should be a positive experience, not a chore. If a workout feels unpleasant or overly strenuous, it’s likely to be abandoned. Exploring various activities, such as swimming, walking, yoga, or tai chi, can help find one that aligns with preferences and helps manage RLS symptoms effectively.
Examples of Low-Impact Exercises Suitable for RLS Patients
Low-impact exercises are often well-tolerated by RLS patients. They put less stress on joints and muscles, reducing the risk of exacerbating symptoms. Here are a few examples:
- Walking: A simple and accessible exercise that can be easily adjusted to different fitness levels. Walking can be done outdoors, on a treadmill, or in a mall. Even short walks can be beneficial.
- Swimming: A low-impact exercise that works the entire body without putting significant stress on joints. The buoyancy of water can also provide support and reduce discomfort.
- Cycling: Indoor or outdoor cycling can be a great way to improve cardiovascular health without putting excessive strain on joints. Adjusting the resistance can tailor the workout to different fitness levels.
- Yoga and Tai Chi: These practices incorporate gentle stretching and movement, improving flexibility and balance while minimizing discomfort.
Importance of Staying Hydrated During Exercise for RLS Patients
Hydration is crucial for everyone, but especially for RLS patients during exercise. Dehydration can worsen RLS symptoms. Drinking plenty of water before, during, and after exercise can help manage symptoms and maintain overall well-being. Carry a water bottle and sip regularly during workouts.
Exercise Modifications to Manage RLS Symptoms
Modifying exercise routines can make them more manageable for RLS patients. Here are some strategies:
- Short, Frequent Workouts: Breaking down workouts into shorter sessions throughout the day can be more tolerable than longer, continuous sessions, especially if RLS symptoms are intense.
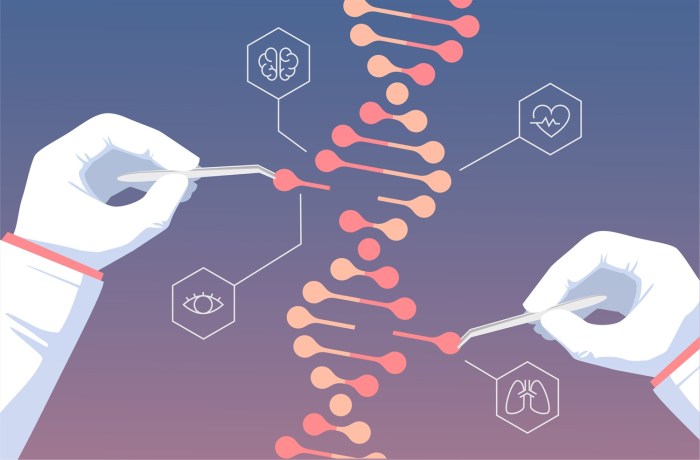
- Warm-up and Cool-down Periods: Incorporating a 5-10 minute warm-up before exercise and a similar cool-down period afterward can help prepare the body and gradually reduce symptoms.
- Listen to Your Body: If symptoms worsen during exercise, stop and rest. Don’t push through the pain. Adjusting the intensity or type of exercise can help manage discomfort and prevent exacerbating RLS symptoms.
- Avoid Overexertion: It’s important to avoid overexerting yourself. Start slowly and gradually increase the intensity and duration of workouts over time.
Exercise and Sleep Quality in RLS: Restless Legs Syndrome Physical Exercise
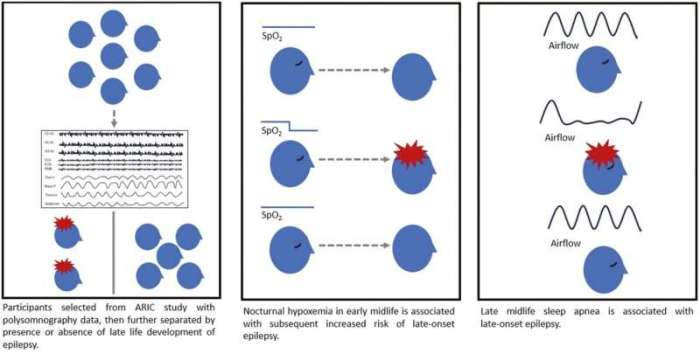
Restless legs syndrome (RLS) can significantly impact sleep quality, making it challenging for individuals to achieve restful sleep. This often leads to daytime fatigue and decreased overall well-being. Conversely, a good night’s sleep can significantly improve RLS symptoms and enhance the effectiveness of exercise routines. Understanding the interplay between exercise, sleep, and RLS is crucial for developing a comprehensive management strategy.Exercise can positively influence sleep quality by promoting relaxation and reducing stress, both of which are important for sleep.
However, the timing and type of exercise play a critical role in optimizing sleep for RLS sufferers. A well-structured exercise routine, combined with appropriate sleep hygiene practices, can lead to improved sleep quality and symptom management.
Impact of Exercise on Sleep-Wake Cycle in RLS
Exercise can affect the sleep-wake cycle in individuals with RLS by regulating the body’s natural circadian rhythm. Regular physical activity can help synchronize the body’s internal clock, improving the consistency of sleep-wake cycles. This improved consistency can translate to more predictable sleep onset and duration. For instance, a consistent evening walk can help regulate the body’s internal clock, promoting better sleep.
Incorporating Exercise into a Bedtime Routine for RLS Management
To effectively incorporate exercise into a bedtime routine, it’s crucial to avoid strenuous workouts too close to bedtime. Light to moderate-intensity exercise, such as a gentle walk or stretching, can be beneficial. The goal is to promote relaxation and reduce the stimulation that could hinder sleep. For instance, a 30-minute brisk walk an hour before bed can promote relaxation and improve sleep quality.
Avoid high-intensity activities immediately prior to sleep.
Sleep Hygiene Practices for Individuals with RLS
Effective sleep hygiene practices can significantly influence sleep quality for individuals with RLS. Consistent sleep schedules, a calming bedtime routine, and a sleep-conducive environment are essential. Avoid caffeine and alcohol before bed, and ensure your bedroom is dark, quiet, and cool. For instance, creating a relaxing bedtime routine, like reading or listening to calming music, can significantly improve sleep quality.
Comparison of Sleep Hygiene Practices and Their Effect on Exercise
Different sleep hygiene practices can influence the effectiveness of exercise for RLS management. For example, a consistent sleep schedule helps regulate the body’s natural sleep-wake cycle, improving both sleep quality and the effectiveness of exercise. Maintaining a consistent sleep schedule and incorporating relaxing pre-sleep activities can help improve sleep quality and the impact of exercise on RLS symptoms.
Relationship Between Exercise Frequency, Duration, and Sleep Quality for RLS Patients
The following table illustrates the potential relationship between exercise frequency, duration, and sleep quality for RLS patients. This is not a definitive study, but provides a hypothetical framework.
| Exercise Frequency | Exercise Duration (minutes) | Sleep Quality (estimated rating on a scale of 1-5, 5 being excellent) |
|---|---|---|
| 3 times per week | 20-30 | 3 |
| 4 times per week | 30-45 | 4 |
| 5 times per week | 45-60 | 4-5 |
Significance of Maintaining a Regular Sleep Schedule for Exercise Routines
Maintaining a regular sleep schedule is crucial for optimizing exercise routines in RLS. A consistent sleep-wake cycle regulates the body’s hormones and other functions, which can positively impact exercise performance and recovery. For instance, if you regularly sleep 7-8 hours and wake up at 7 am, your body will adapt to this routine, making it easier to maintain an exercise schedule and improving sleep quality.
This regularity will make exercise routines more sustainable.
Exercise and RLS: Illustrative Examples
Finding the right exercise routine for restless legs syndrome (RLS) can feel like searching for a needle in a haystack. However, with careful consideration and adaptation, exercise can be a powerful tool in managing RLS symptoms. This section will provide practical examples and strategies for incorporating exercise into your RLS management plan.Understanding that RLS often manifests with an urge to move, finding exercises that provide soothing movement without exacerbating the discomfort is crucial.
This involves careful selection and modification of routines to suit individual needs and tolerances. This section will highlight specific exercises and routines that can be adapted for individuals with RLS.
Specific Exercises and Routines Adaptable for RLS
Many forms of exercise can be beneficial for RLS, but it’s crucial to choose activities that promote relaxation and controlled movement. Low-impact exercises are often a good starting point. Examples include walking, swimming, cycling, and water aerobics. These activities put less stress on joints while providing cardiovascular benefits.
Modifying Common Exercises for RLS Patients
Modifying existing exercise routines is often necessary to accommodate RLS symptoms. For instance, a brisk walk might be adjusted by incorporating short periods of rest or slower paces when the urge to move intensifies. Gentle stretching, focusing on areas that provide comfort and relaxation, is also beneficial. If high-impact exercises are difficult, consider substituting with low-impact alternatives.
For example, instead of running, opt for walking or swimming.
Importance of Proper Warm-up and Cool-down Procedures
A comprehensive warm-up and cool-down routine are essential for RLS patients. A gradual warm-up helps prepare the body for exercise and can prevent sudden movements that might trigger the urge to move. A cool-down routine allows the body to gradually return to a resting state, reducing the risk of discomfort. This is particularly important for RLS patients, as abrupt changes in activity can exacerbate symptoms.
Warm-up Example:
Start with 5 minutes of gentle stretching, focusing on major muscle groups like the legs, arms, and back. Include gentle arm circles, leg swings, and torso twists. Gradually increase the intensity of the movements, incorporating walking or light cardio.
Cool-down Example:
Begin with 5 minutes of light walking or slow cycling. Then, gradually transition to static stretching, holding each stretch for 15-30 seconds. Focus on the muscles that were worked during the exercise.
Resources for Further Information on Exercise and RLS
- The National Institutes of Health (NIH) website: A wealth of information on RLS, including research findings and treatment options.
- The Restless Legs Syndrome Foundation: Provides support groups, educational materials, and up-to-date research on RLS.
- Books on exercise and health: Many books provide practical guidance on incorporating exercise into daily routines.
These resources can provide valuable insights into managing RLS through exercise and offer support networks for individuals affected by this condition.
Benefits of Combining Exercises for RLS
Combining different forms of exercise can offer a holistic approach to managing RLS symptoms. For example, incorporating yoga or tai chi with low-impact cardio can provide both physical benefits and mental relaxation. This can lead to better symptom control and improved overall well-being.
Impact of Various Forms of Exercise on RLS Symptoms
Yoga and tai chi, with their focus on mindful movement and controlled breathing, can be particularly beneficial for RLS. These practices promote relaxation and reduce stress, which can contribute to decreased RLS symptoms. Water-based exercises, like swimming or water aerobics, offer low-impact movement and support, which can be particularly accommodating for individuals with RLS. Swimming, for example, can help to alleviate muscle tension and promote relaxation.
Consult with a healthcare professional to determine the most suitable form of exercise for your specific needs.
Final Thoughts
In conclusion, incorporating physical exercise into a RLS management plan can significantly improve overall well-being. By exploring different exercise types, adjusting intensity and duration, and prioritizing individual needs, individuals with RLS can find effective strategies for symptom relief and enhanced sleep quality. Remember to always consult with a healthcare professional before starting any new exercise program. This guide provides a starting point, but personalization is key to achieving optimal results.


![🔥 [48+] Night HD Wallpapers | WallpaperSafari Night sweats during period](https://lyricapills.com/wp-content/uploads/2025/06/night-walk-park-hd-wallpaper-1.jpg)