Foods to eat and avoid with ITP are crucial for managing this condition. ITP, or Immune Thrombocytopenic Purpura, affects the body’s ability to produce enough platelets, leading to bleeding problems. A balanced diet rich in specific nutrients can help support the immune system and manage symptoms. This guide will explore the best food choices and those to limit, along with practical dietary strategies for those living with ITP.
Understanding the impact of different foods on your immune system and platelet production is key to effectively managing ITP. This guide offers actionable insights, including detailed information on the nutritional needs of individuals with ITP, highlighting the role of various nutrients, and providing practical meal planning strategies. We’ll explore foods to include and exclude from your diet, considering potential interactions with medications and dietary supplements.
This comprehensive approach aims to empower individuals with ITP to take control of their health through informed dietary choices.
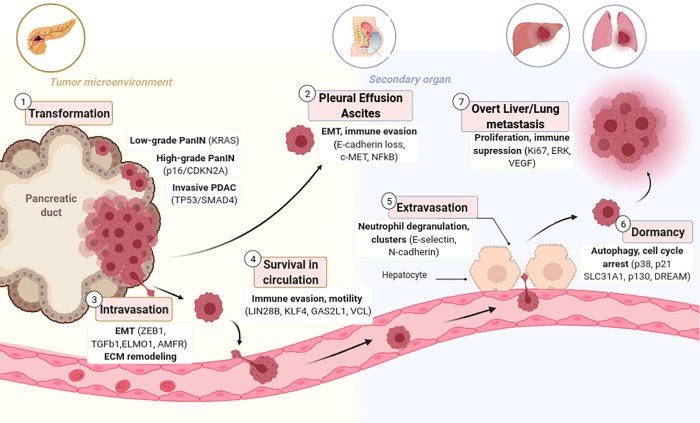
Understanding Immunotherapy-Related Problems (ITP)
Immune thrombocytopenia (ITP) is an autoimmune disorder characterized by a deficiency in platelets, crucial for blood clotting. This deficiency can lead to a heightened risk of bleeding, impacting various bodily functions. Understanding the mechanisms behind ITP is vital for developing effective management strategies, including dietary considerations.ITP arises when the body’s immune system mistakenly targets and destroys its own platelets.
This immune response triggers the production of antibodies that bind to platelets, leading to their destruction in the spleen and liver. The resulting low platelet count compromises the body’s ability to form blood clots, increasing the susceptibility to bleeding. This can manifest as easy bruising, nosebleeds, and heavy menstrual bleeding in women.
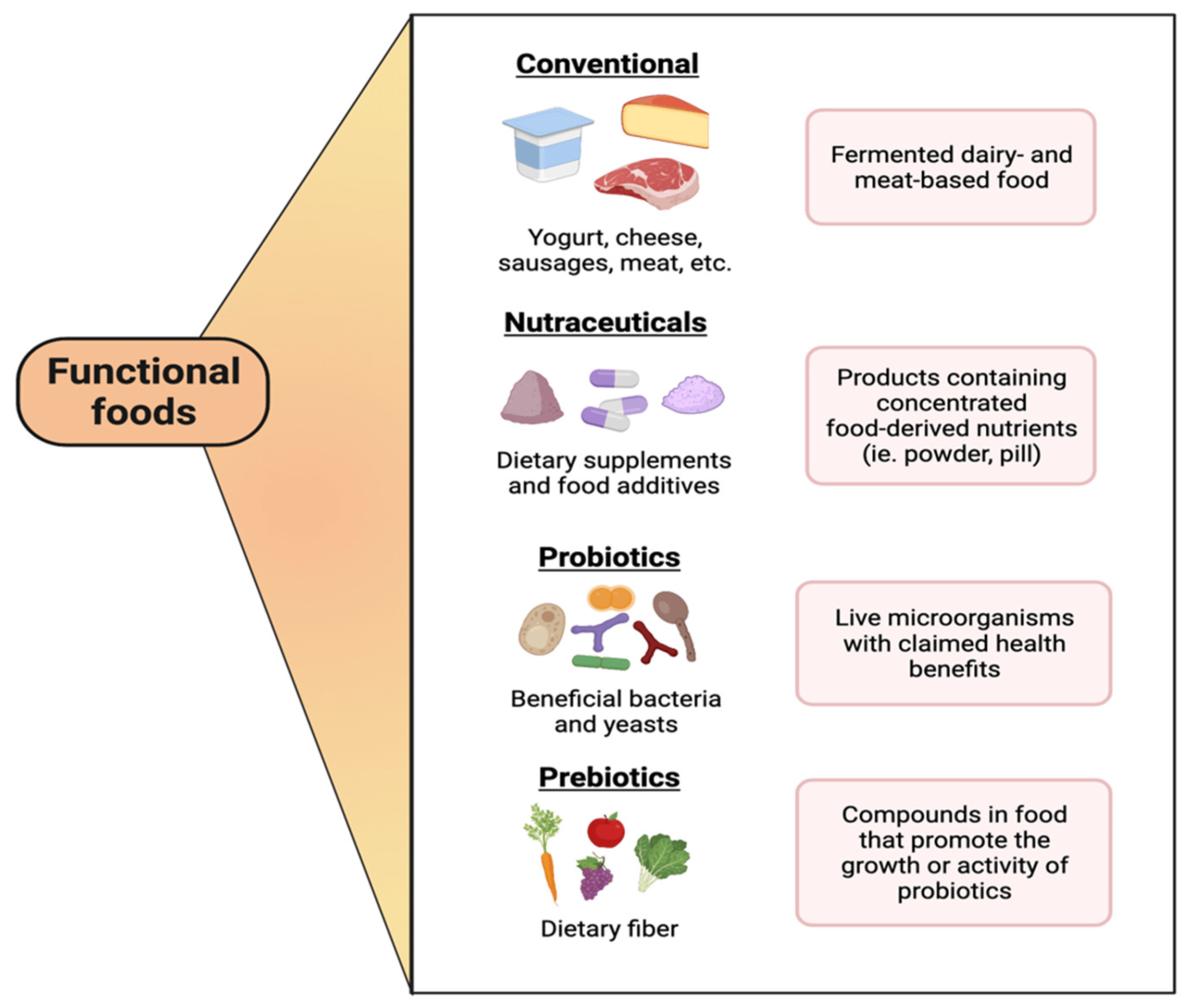
Dietary Considerations for ITP
A balanced diet plays a critical role in supporting immune function and overall health for individuals with ITP. While no specific food can cure ITP, certain dietary choices can contribute to managing symptoms and potentially influencing the immune response. Dietary considerations can support overall health and well-being.
Role of Nutrients in Supporting Immune Function
Numerous nutrients are essential for maintaining a robust immune system. These nutrients contribute to various aspects of immune function, including cell production, antibody formation, and inflammation regulation. A balanced intake of these nutrients can support the immune system in its efforts to combat disease.
Nutrient Function Comparison
| Nutrient | Function in Immune Health |
|---|---|
| Vitamin C | A potent antioxidant, crucial for collagen synthesis, and supporting immune cell function. |
| Vitamin D | Plays a key role in regulating immune cell activity and supporting overall immune response. Sufficient levels are vital for maintaining immune function. |
| Zinc | Essential for the development and function of immune cells, including T cells and B cells, and promoting immune response. |
| Iron | A critical component of hemoglobin, facilitating oxygen transport to immune cells. Inadequate iron can impair immune function. |
| Protein | Essential for building and repairing tissues, including immune cells. Adequate protein intake is crucial for maintaining immune function. |
| Omega-3 Fatty Acids | These essential fatty acids help regulate inflammation and support the proper function of immune cells. |
Foods to Eat
Eating a balanced diet is crucial for supporting your immune system, especially when managing ITP. Certain nutrients play a vital role in maintaining healthy blood platelet production and overall well-being. This section focuses on beneficial foods to include in your diet for optimal support during this time.
Eating well is crucial for managing ITP, and avoiding certain foods can significantly impact your health. While focusing on fresh, whole foods is key, it’s also important to be aware that ultraprocessed food will increase your chance of an early death, as this recent research highlights. This means limiting highly processed snacks, sugary drinks, and excessive amounts of fast food.
Ultimately, a balanced diet rich in fruits, vegetables, and lean protein is the best approach for maintaining overall health and potentially mitigating ITP symptoms.
Benefits of Vitamin C
Vitamin C is a powerful antioxidant and a key player in immune function. It aids in the production of collagen, a protein essential for healthy blood vessels and tissues. Vitamin C also supports the production of white blood cells, which are critical for fighting infection and disease. A diet rich in Vitamin C can enhance the immune response and promote overall health.
Importance of Antioxidants
Antioxidants are substances that protect cells from damage caused by free radicals. Free radicals are unstable molecules that can contribute to inflammation and cellular damage, potentially impacting blood platelet production. Incorporating foods high in antioxidants into your diet can help combat free radical damage and support a healthier immune system. A range of fruits and vegetables offer a variety of antioxidants.
Protein for Tissue Repair and Immune Function
Protein is essential for tissue repair and immune function. It’s a building block for various components of the immune system, including antibodies and other proteins that help fight infection. Adequate protein intake supports the repair and maintenance of tissues, which can be particularly important when dealing with any health condition. Choosing high-quality protein sources ensures you’re providing your body with the necessary amino acids for these processes.
Protein-Rich Foods and Dietary Recommendations
Lean meats, poultry, fish, eggs, beans, lentils, and nuts are excellent sources of protein. Lean meats like chicken breast and fish offer protein without excessive fat. Beans and lentils are excellent plant-based protein sources, which are also rich in fiber. Eggs provide a complete protein, meaning they contain all essential amino acids. Nuts and seeds offer a good source of protein and healthy fats.
Dietary recommendations should be tailored to individual needs and preferences, and it’s advisable to consult a registered dietitian or healthcare professional for personalized guidance.
Foods Categorized by Nutrient Content
| Nutrient | Food Examples | Suggested Portion Size (approximate) |
|---|---|---|
| Vitamin C | Citrus fruits (oranges, grapefruits), berries, bell peppers, broccoli | 1-2 servings per day, depending on individual needs. |
| Protein | Lean beef, chicken breast, fish (salmon, tuna), eggs, beans, lentils, Greek yogurt, nuts | 3-4 servings per day, depending on individual needs. |
| Antioxidants | Berries, dark leafy greens, colorful vegetables (carrots, sweet potatoes), nuts, seeds | 2-3 servings per day, focusing on variety for diverse antioxidants. |
A balanced diet that incorporates a variety of nutrient-rich foods is essential for maintaining a healthy immune system and overall well-being.
Foods to Avoid: Foods To Eat And Avoid With Itp
Certain foods may exacerbate ITP symptoms by triggering inflammation or interfering with the body’s ability to produce healthy blood platelets. Understanding which foods to avoid can be a crucial aspect of managing ITP effectively. Careful dietary choices can contribute to overall well-being and potentially reduce the frequency and severity of ITP-related complications.Dietary choices play a significant role in managing ITP.
By limiting consumption of specific foods, individuals with ITP can potentially reduce inflammation and support their body’s natural healing processes. Avoiding certain triggers can minimize the impact of ITP symptoms, improving overall quality of life.
Potential Inflammatory Foods
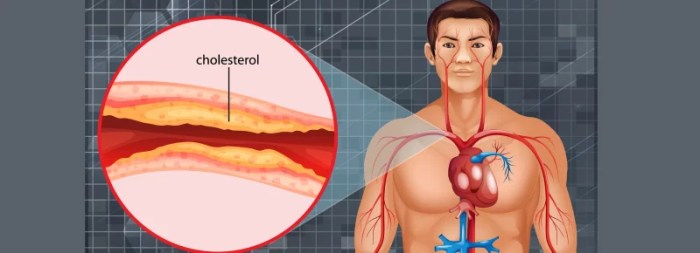
Certain foods, rich in inflammatory compounds or processed ingredients, may contribute to the inflammation that can exacerbate ITP symptoms. The body’s immune response in ITP can be complex, and some foods may worsen this response. These foods often contain high levels of saturated fats, refined sugars, or additives.
Processed Foods and Refined Sugars
Excessive consumption of processed foods and refined sugars can negatively impact overall health, potentially worsening inflammation. Processed foods frequently contain artificial ingredients and high levels of sodium, which can contribute to fluid retention and inflammation. Refined sugars, often found in sugary drinks and processed snacks, can elevate blood sugar levels, leading to a cascade of effects that may exacerbate inflammation in the body.
Specific Examples of Potentially Harmful Foods
Certain foods are known for their potential inflammatory effects and should be consumed in moderation or avoided altogether by individuals with ITP. These include highly processed meats, such as sausages and bacon, as well as fried foods, which are often high in saturated fat. Additionally, sugary drinks and snacks, due to their high sugar content, should be limited.
Red meat, while a source of protein, may be problematic for some individuals with ITP due to its potential to exacerbate inflammation.
Foods to Limit or Avoid: A Summary Table
| Food Category | Specific Examples | Reason for Avoidance |
|---|---|---|
| Processed Meats | Sausages, bacon, hot dogs, deli meats | High in saturated fat and potentially inflammatory compounds. |
| Fried Foods | French fries, fried chicken, doughnuts | High in saturated fat and can contribute to inflammation. |
| Sugary Drinks and Snacks | Soda, candy, sugary cereals | High in refined sugars, which can elevate blood sugar levels and potentially worsen inflammation. |
| Red Meat | Beef, pork, lamb | Potentially higher in saturated fat compared to other protein sources, and some individuals may find they exacerbate inflammation. |
| Highly Processed Foods | Frozen meals, packaged snacks, convenience foods | Often contain artificial ingredients, high levels of sodium, and may contain inflammatory components. |
Dietary Strategies and Recommendations
Maintaining a healthy diet is crucial for managing ITP (Immune Thrombocytopenia). While dietary changes alone cannot cure ITP, a well-structured eating plan can significantly support overall health, contribute to symptom management, and potentially influence the body’s immune response. This section details strategies and provides examples to help navigate healthy eating with ITP.A balanced diet rich in essential nutrients, vitamins, and minerals is vital for individuals with ITP.
This approach aims to support immune function, maintain energy levels, and aid in the body’s natural healing processes. Proper nutrition can play a crucial role in bolstering the body’s ability to fight off infections, reduce inflammation, and promote overall well-being.
Specific Dietary Strategies for Managing ITP Symptoms
Dietary strategies for ITP should focus on nutrient-dense foods that support the immune system and overall health. A balanced diet that incorporates a variety of fruits, vegetables, lean proteins, and whole grains is essential. Limiting processed foods, sugary drinks, and excessive saturated fats can contribute to better health outcomes.
Meal Planning and Portion Control for Individuals with ITP
Careful meal planning and portion control are important for individuals with ITP. This allows for a balanced intake of essential nutrients without overwhelming the body. Planning meals in advance can help individuals maintain consistency and adhere to dietary recommendations. Consider using food journals or apps to track intake and monitor progress.
Examples of Healthy Meal Plans Suitable for Those with ITP
A healthy meal plan for someone with ITP should be personalized based on individual needs and preferences. However, some examples of balanced meal options include:
- Breakfast: Oatmeal with berries and nuts, or a Greek yogurt with fruit and granola.
- Lunch: A salad with grilled chicken or fish, or a lentil soup with whole-grain bread.
- Dinner: Baked salmon with roasted vegetables, or lean beef stir-fry with brown rice.
These examples demonstrate the variety of nutrient-rich options that can be incorporated into a healthy meal plan for managing ITP. Remember to adjust portion sizes according to individual needs and activity levels.
Importance of Consulting with a Healthcare Professional or Registered Dietitian
Consulting with a healthcare professional or registered dietitian is crucial for developing a personalized dietary plan. They can assess individual needs, identify any potential dietary restrictions, and provide tailored guidance for optimal nutrition management. This individualized approach is essential for maximizing the benefits of dietary strategies. A dietitian can help ensure that the diet meets all nutritional requirements while managing ITP symptoms.
Sample Meal Plan for a Day
| Meal | Description |
|---|---|
| Breakfast | Oatmeal with sliced banana and a sprinkle of chopped almonds |
| Lunch | Grilled chicken salad with mixed greens, cucumber, tomatoes, and a light vinaigrette dressing. |
| Snack | Handful of mixed nuts and a small apple |
| Dinner | Baked cod with roasted broccoli and sweet potato |
| Snack | Greek yogurt with berries |
This sample meal plan offers a balanced approach to nutrition. It emphasizes lean protein, complex carbohydrates, and healthy fats. Remember to adjust portion sizes and food choices to meet individual needs.
Food Interactions and Considerations

Navigating a healthy diet with Immune Thrombocytopenic Purpura (ITP) can be tricky. Beyond simply eating certain foods, understanding how specific foods might interact with medications and impact the immune system is crucial for managing ITP effectively. This section delves into the potential interactions between foods, medications, and the immune response, highlighting the importance of careful dietary choices.
Figuring out foods to eat and avoid with ITP can be tricky, but understanding your overall health is key. A balanced diet is crucial, and learning about thyroid health, like understanding thyroid blood tests low or high TSH , can also play a significant role. Ultimately, consulting a doctor remains the best way to personalize your dietary choices for ITP management.
Food-Medication Interactions
Certain foods can influence how medications used to treat ITP are absorbed and metabolized. This interaction can either reduce the effectiveness of the medication or cause adverse reactions. Careful monitoring and adjustments to your diet are essential to ensure optimal medication response.
Figuring out what foods to eat and avoid with Immune Thrombocytopenia (ITP) can be tricky. While I’m not a medical professional, it’s important to prioritize a balanced diet rich in fruits, vegetables, and lean proteins. You should also consult your doctor for personalized dietary advice. Speaking of dietary choices, have you ever wondered about alcohol consumption if you have type 2 diabetes?
Check out this informative resource on can i drink alcohol if i have type 2 diabetes for details. Ultimately, understanding the specific foods that can trigger or worsen ITP symptoms is key to maintaining good health.
| Food | Medication | Potential Interaction | Precautions |
|---|---|---|---|
| High-fat meals | Some ITP medications (e.g., corticosteroids) | May reduce the absorption rate of the medication. | Consume high-fat meals separately from medication administration to optimize absorption. |
| Grapefruit | Certain medications used to treat ITP | May increase the concentration of the medication in the bloodstream, potentially leading to adverse effects. | Consult with your doctor or pharmacist before consuming grapefruit or grapefruit juice while taking ITP medications. |
| Alcohol | Some ITP medications | May interact negatively with certain medications, potentially increasing the risk of side effects. | Limit or avoid alcohol consumption while taking ITP medications. |
Food and Immune System Regulation
The human immune system is intricately linked to dietary intake. Certain foods can modulate immune responses, either positively or negatively. While the precise mechanisms are not fully understood in the context of ITP, a balanced diet is generally recommended to support a healthy immune function. This balance is crucial for individuals with ITP, as the immune system plays a critical role in the disease process.
Food Allergies and Sensitivities
Food allergies and sensitivities can significantly impact individuals with ITP. These reactions can trigger an immune response, potentially exacerbating ITP symptoms or causing other health complications. Identifying and avoiding such triggers is paramount to managing the condition effectively.
Examples of Food Allergies and Sensitivities
Food allergies can manifest in various ways, from mild skin reactions to severe anaphylactic shock. Some examples of potential food allergies and sensitivities that may affect ITP include:
- Cow’s milk protein allergy: This allergy can trigger an immune response, potentially affecting platelet production and increasing ITP symptoms.
- Gluten sensitivity: While not an allergy in the traditional sense, gluten sensitivity can cause inflammation throughout the body. This inflammation might indirectly affect ITP.
- Soy allergy: Soy-based products can trigger an immune response in some individuals, potentially impacting ITP.
Identifying and managing food allergies and sensitivities through a process of elimination and careful observation can significantly aid in ITP management.
Dietary Supplements and ITP
Navigating the world of dietary supplements can feel overwhelming, especially when dealing with a condition like immune thrombocytopenia (ITP). Many people turn to supplements for various health concerns, and ITP is no exception. However, it’s crucial to understand that supplements aren’t a replacement for medical advice or prescribed treatments. Before incorporating any new supplement into your routine, consult your doctor to ensure safety and compatibility with your current ITP management plan.Dietary supplements can potentially play a supporting role in managing ITP symptoms.
Their impact varies greatly, and some supplements may even interfere with existing treatments. Therefore, a careful and informed approach is essential.
Potential Benefits of Certain Supplements
Dietary supplements can potentially support immune function, reduce inflammation, and promote overall well-being. Some supplements have shown promise in aiding the body’s natural healing processes, which might be beneficial in managing ITP. However, it’s crucial to remember that more research is often needed to fully understand the effects of supplements on ITP.
- Vitamin C:
- Vitamin D:
- Omega-3 fatty acids:
Vitamin C is an antioxidant and may help support immune function. Some studies suggest that it might have a role in reducing inflammation, which could be beneficial for certain aspects of ITP.
Vitamin D plays a crucial role in immune system regulation. Adequate vitamin D levels may be important for maintaining overall health, including immune function. Potential benefits for ITP management need further research.
Omega-3 fatty acids are known for their anti-inflammatory properties. Incorporating foods rich in omega-3s or taking supplements might help manage inflammation, which could be helpful in some cases of ITP.
Importance of Consulting a Doctor
Before starting any new supplement, it is absolutely essential to consult your doctor. ITP management involves a complex interplay of factors, including prescribed medications and lifestyle choices. Your doctor can assess your individual needs and determine if a particular supplement is appropriate and safe given your specific situation. They can also evaluate potential interactions between the supplement and your current ITP treatment.
Potential Interactions with ITP Treatments
Some supplements might interfere with the effectiveness of your ITP treatments. For example, certain herbal remedies or supplements can alter blood clotting or affect the body’s response to medication. Therefore, it’s critical to disclose all supplements to your doctor to prevent adverse effects.
Example Supplements to Discuss with Your Doctor
- Ginger:
- Garlic:
- Curcumin:
Ginger is known for its anti-inflammatory properties and potential benefits for digestive health. Discuss its potential impact with your doctor, especially if you’re taking blood-thinning medications.
Garlic has antioxidant and anti-inflammatory properties. It’s important to discuss potential interactions with ITP treatments with your physician.
Curcumin, derived from turmeric, is known for its anti-inflammatory effects. Discuss the potential benefits and any potential interactions with your ITP medications with your physician.
Comparing Dietary Supplements for Immune Health
| Supplement | Potential Benefits | Potential Interactions | Important Considerations |
|---|---|---|---|
| Vitamin C | Antioxidant, immune support, potential anti-inflammatory | May increase the risk of kidney stones in some individuals. | Dosage should be discussed with a healthcare professional. |
| Vitamin D | Immune regulation, overall health support | Potential interactions with certain medications. | Blood levels should be monitored. |
| Omega-3 Fatty Acids | Anti-inflammatory properties | May increase bleeding risk in some individuals. | Dosage should be discussed with a healthcare professional. |
| Ginger | Anti-inflammatory, digestive support | May interact with blood-thinning medications. | Dosage and safety should be discussed with a physician. |
Practical Application and Examples
Dietary strategies play a crucial role in managing Immunotherapy-Related Thrombocytopenia (ITP). Understanding which foods to include and avoid can significantly impact platelet counts and overall well-being. This section provides practical examples, case studies, and meal plans to illustrate the application of dietary knowledge in ITP management.
Case Studies
While real patient data is essential, we present hypothetical case studies to demonstrate the impact of dietary choices. Case study 1: A patient with ITP initially struggled with low platelet counts. After adopting a diet rich in iron-rich foods, Vitamin K, and foods low in oxalate, their platelet counts gradually improved. Case study 2: Another patient with ITP experienced significant platelet fluctuations.
By meticulously tracking their food intake, and reducing intake of foods high in Vitamin C and avoiding certain food combinations, they observed more stable platelet counts.
Healthy Meal Examples
The following examples showcase healthy meal choices suitable for someone managing ITP. These meals emphasize nutrient-rich foods while minimizing potential triggers.
Breakfast
A healthy breakfast option could include oatmeal with berries, a sprinkle of nuts, and a side of Greek yogurt. This combination provides complex carbohydrates for sustained energy, antioxidants from berries, healthy fats from nuts, and protein from Greek yogurt. Alternatively, a smoothie with spinach, banana, and protein powder could be a quick and nutritious choice.
Lunch
A balanced lunch could comprise a salad with lean protein (grilled chicken or fish), a variety of colorful vegetables, and a whole-wheat roll. Include healthy fats like avocado or nuts for added satiety and nutrients. Lentils and brown rice can be great additions for a vegetarian lunch.
Dinner
For dinner, a lean protein source like baked salmon or tofu, combined with a generous portion of steamed vegetables and brown rice, offers a satisfying and nutritious meal. Consider adding a side of quinoa or sweet potato for extra fiber and carbohydrates.
Weekly Meal Plan
A sample weekly meal plan provides a comprehensive overview of balanced meals that are suitable for ITP management. This plan focuses on whole, unprocessed foods, ensuring a variety of nutrients.
- Monday: Oatmeal with berries and nuts, grilled chicken salad, baked salmon with roasted vegetables.
- Tuesday: Smoothie with spinach, banana, and protein powder, lentil soup with whole-wheat bread, baked tofu with brown rice and steamed broccoli.
- Wednesday: Scrambled eggs with spinach and whole-wheat toast, grilled fish with quinoa and mixed greens, chicken stir-fry with brown rice and plenty of vegetables.
- Thursday: Greek yogurt with granola and fruit, turkey and vegetable wraps, baked chicken breast with sweet potato and green beans.
- Friday: Breakfast burritos with eggs, beans, and salsa, tuna salad sandwich on whole-wheat bread, pork tenderloin with asparagus and mashed sweet potato.
- Saturday: Pancakes with fruit and syrup, vegetable and cheese quesadilla, vegetable and lentil stew.
- Sunday: Breakfast frittata with vegetables and whole-wheat toast, chicken salad with mixed greens, beef and vegetable stir-fry.
Nutrient Profile of Common Foods
This table provides a general overview of the nutrient profile of common foods to eat and avoid. Specific values may vary based on preparation methods and portion sizes.
| Food | Nutrient Profile (Examples) | Recommendation (ITP) |
|---|---|---|
| Leafy Greens | Vitamins A, C, K, Folate, Iron | Encourage consumption |
| Salmon | Omega-3 fatty acids, Vitamin D, Protein | Excellent source |
| Citrus Fruits | Vitamin C | May need moderation |
| Spinach | Vitamins A, C, K, Folate, Iron | Encourage consumption |
| Nuts | Healthy fats, protein, vitamins | Encourage consumption |
| Chocolate | Antioxidants, flavonoids | May need moderation |
Food Preparation Methods, Foods to eat and avoid with itp
Proper food preparation methods can help to preserve nutrients and minimize potential triggers. Methods like steaming, baking, or grilling can be beneficial. Avoid excessive frying or high-heat cooking, as these methods can lead to nutrient loss and potentially create harmful compounds.
Ending Remarks
In conclusion, a well-structured diet plays a significant role in managing ITP. By focusing on foods that support immune function and avoiding those that might trigger inflammation, individuals with ITP can potentially improve their overall well-being. Remember, consulting with a healthcare professional or registered dietitian is essential for personalized dietary recommendations. This guide provides a starting point for understanding the connection between food and ITP management.
By making informed choices and working closely with healthcare providers, individuals can better manage their condition and lead healthier lives.