Ways to lose weight with asthma is a multifaceted journey that delves into the intricate relationship between your breathing condition and your body’s composition. This exploration unveils practical strategies for managing weight while effectively controlling asthma symptoms. We’ll uncover dietary secrets, exercise routines tailored for asthma, and crucial lifestyle adjustments that can lead to a healthier, more balanced life.
Understanding the unique physiological effects of asthma on metabolism is key to crafting a successful weight management plan. This comprehensive guide will equip you with actionable advice and a deeper understanding of the factors influencing weight and asthma, such as medication side effects and stress management techniques.
Understanding Asthma and Weight Management
Managing weight effectively can be challenging for individuals with asthma. The interplay between the chronic respiratory condition and dietary habits, activity levels, and medication use often complicates the process. Understanding the specific physiological effects of asthma on metabolism and weight is crucial for developing personalized strategies that support both respiratory health and well-being.Asthma’s impact on metabolism extends beyond the immediate effects of breathing difficulties.
Chronic inflammation, a hallmark of asthma, can influence appetite, energy expenditure, and even hormonal balance. This inflammatory response can lead to changes in metabolism, making weight management more complex. Furthermore, the medications used to control asthma symptoms can also have unintended consequences on appetite and body composition.
Physiological Effects of Asthma on Metabolism
Asthma’s inflammatory nature affects the body’s metabolic processes. The persistent inflammation can trigger changes in hormones like cortisol, which can impact appetite and fat storage. Furthermore, the constant struggle to breathe can lead to reduced physical activity, further affecting energy expenditure and potentially contributing to weight gain. Patients may also experience fatigue and decreased motivation, making healthy lifestyle choices more challenging.
Common Misconceptions About Weight Gain and Asthma
There are several misconceptions about weight gain in individuals with asthma. One common misconception is that weight gain is solely a result of medication side effects. While medication can play a role, it’s important to understand that asthma itself can contribute to metabolic changes. Another misconception is that asthma sufferers are inherently predisposed to obesity. While some factors might increase risk, it’s not an automatic correlation.
The complexity of the relationship highlights the importance of personalized approaches to weight management.
Role of Inflammation in Asthma and Weight Issues
Inflammation is a central player in both asthma and weight management challenges. In asthma, inflammation in the airways restricts airflow and triggers symptoms. Similarly, chronic inflammation throughout the body can impact metabolism, affecting appetite regulation, fat storage, and energy expenditure. The inflammatory cascade in both conditions can contribute to a vicious cycle of reduced activity, altered appetite, and potentially, weight gain.
Importance of Individual Factors in Weight Management
Weight management strategies for individuals with asthma must consider individual factors like age, gender, and activity levels. For example, adolescents with asthma may have different metabolic needs than adults. Likewise, women may experience hormonal fluctuations that influence weight differently than men. Understanding these individual variations is critical for creating effective and sustainable weight management plans.
Comparison of Asthma Medications and Their Effects on Appetite and Metabolism
| Medication Type | Potential Effects on Appetite | Potential Effects on Metabolism | Considerations |
|---|---|---|---|
| Inhaled Corticosteroids | Generally, minimal or no significant changes in appetite. | May slightly impact metabolism by affecting cortisol levels; studies are inconclusive. | Individual responses may vary. Monitor for any changes in appetite or energy levels. |
| Leukotriene Modifiers | Generally, minimal or no significant changes in appetite. | May have minimal or no significant impact on metabolism. | Individual responses may vary. Monitor for any changes in appetite or energy levels. |
| Long-Acting Beta-2 Agonists | Potential for increased appetite, but the effect is usually mild. | May slightly increase energy expenditure, but the impact on metabolism is generally minimal. | Individual responses may vary. Monitor for any changes in appetite or energy levels. Combine with other lifestyle changes for optimal weight management. |
| Oral Corticosteroids | Significant increase in appetite and potential for increased food cravings. | Significant impact on metabolism, leading to potential weight gain due to increased cortisol levels and decreased energy expenditure. | Close monitoring of weight and dietary intake is essential. Consider strategies to mitigate appetite changes and increase physical activity. |
Dietary Strategies for Asthma Patients
Managing asthma effectively often involves a multifaceted approach, and diet plays a crucial role. Proper nutrition can help stabilize inflammation, improve lung function, and support a healthy weight, all of which are beneficial for individuals with asthma. A well-balanced diet, tailored to individual needs, can significantly impact asthma control.A personalized dietary strategy, combined with other asthma management techniques, can contribute to better overall health and quality of life.
It’s essential to understand that while diet can influence asthma symptoms, it’s not a cure. Consult with a healthcare professional or registered dietitian to develop a plan that aligns with your specific asthma needs and overall health goals.
Healthy Eating Patterns
Different eating patterns can be beneficial for asthma management. Mediterranean diets, rich in fruits, vegetables, whole grains, and healthy fats, have shown promise in reducing inflammation and improving respiratory health. A plant-based diet, emphasizing fruits, vegetables, legumes, and whole grains, can also contribute to better asthma control. These dietary approaches focus on nutrient-rich foods and promote a balanced intake of essential vitamins, minerals, and antioxidants.
Sample Weekly Meal Plan
This sample meal plan provides a framework for a weekly diet rich in nutrients. It emphasizes portion control and a variety of foods, crucial for individuals with asthma. Adjust portions based on individual needs and activity levels. Remember to consult with a healthcare professional or registered dietitian for personalized recommendations.
- Monday: Breakfast: Oatmeal with berries and nuts; Lunch: Salad with grilled chicken or fish; Dinner: Lentil soup with whole-wheat bread.
- Tuesday: Breakfast: Greek yogurt with fruit and granola; Lunch: Leftover lentil soup; Dinner: Baked salmon with roasted vegetables.
- Wednesday: Breakfast: Whole-wheat toast with avocado and egg; Lunch: Quinoa salad with chickpeas and vegetables; Dinner: Chicken stir-fry with brown rice.
- Thursday: Breakfast: Smoothie with fruit, spinach, and protein powder; Lunch: Turkey and cheese sandwich on whole-wheat bread; Dinner: Vegetarian chili with cornbread.
- Friday: Breakfast: Scrambled eggs with spinach and whole-wheat toast; Lunch: Leftover vegetarian chili; Dinner: Pizza with whole-wheat crust and vegetables.
- Saturday: Breakfast: Pancakes made with whole-wheat flour and topped with fruit; Lunch: Leftover pizza; Dinner: Pasta with marinara sauce and vegetables.
- Sunday: Breakfast: Waffles made with whole-wheat flour and topped with berries and nuts; Lunch: Salad with grilled chicken or fish; Dinner: Roast chicken with roasted vegetables.
Foods to Avoid or Limit
Certain foods can trigger asthma symptoms in susceptible individuals. Identifying and avoiding or limiting these foods is crucial for managing asthma.
- Dairy products: Some individuals experience heightened sensitivity to dairy products, which can trigger inflammation in the airways.
- Processed foods: These often contain additives and preservatives that can exacerbate asthma symptoms in some individuals.
- Highly processed meats: Red meat, particularly processed meats, can increase inflammation in the body, potentially triggering asthma attacks.
- Sugary drinks and foods: Excessive sugar intake can lead to inflammation and blood sugar fluctuations, impacting asthma control.
- Certain fruits and vegetables: Some individuals might be allergic to or sensitive to specific fruits and vegetables.
Importance of Hydration
Adequate hydration is essential for overall health and especially for managing asthma. Water helps thin mucus, making it easier to clear the airways. Staying hydrated also aids in weight management by regulating metabolism and appetite.
Impact of Carbohydrates on Blood Sugar and Asthma
Different types of carbohydrates impact blood sugar levels differently. Complex carbohydrates, found in whole grains, fruits, and vegetables, release sugar slowly into the bloodstream, preventing significant spikes. Simple carbohydrates, found in sugary drinks and processed foods, release sugar quickly, potentially leading to blood sugar fluctuations and exacerbating asthma symptoms.
Healthy Snack Options
Healthy snacks can be an integral part of a balanced diet for individuals with asthma. These options provide sustained energy and essential nutrients.
| Snack | Description |
|---|---|
| Fruits (apple, banana, berries) | Provide vitamins, minerals, and antioxidants. |
| Vegetables (carrots, celery, cucumber) | Offer fiber and vitamins. |
| Plain yogurt | A source of protein and probiotics. |
| Hard-boiled eggs | Excellent source of protein. |
| Whole-grain crackers with hummus | Provide fiber and protein. |
Exercise and Activity Recommendations

Staying active is crucial for managing both asthma and weight. Regular physical activity strengthens lung function, improves cardiovascular health, and helps maintain a healthy weight, all of which can positively impact asthma control. Finding activities you enjoy and can consistently incorporate into your routine is key to long-term success.A well-structured exercise program, tailored to individual needs and asthma triggers, can significantly improve overall health and well-being for those with asthma.
It’s essential to remember that consistency is paramount. Even short bursts of activity can contribute to positive outcomes when integrated into a regular schedule. Proper warm-up and cool-down procedures are essential to prevent asthma symptoms and promote optimal recovery.
Importance of Regular Physical Activity
Regular physical activity is vital for asthma patients because it strengthens the respiratory muscles, improves lung capacity, and enhances overall cardiovascular health. These benefits translate to improved asthma control and reduced symptom frequency. Furthermore, regular exercise contributes to weight management by burning calories and boosting metabolism. This dual impact on health significantly improves the quality of life for individuals with asthma.
Exercise Routines Suitable for Asthma Patients
Exercise routines for asthma patients should prioritize gradual progression and symptom monitoring. Begin with short, low-intensity activities and gradually increase the duration and intensity over time. It’s crucial to listen to your body and adjust the intensity based on your individual needs and asthma symptoms. Regular monitoring of breathing patterns and exertion levels will help you identify your personal limits and prevent overexertion.
Relationship Between Exercise and Lung Function
Exercise plays a significant role in improving lung function for individuals with asthma. Physical activity strengthens respiratory muscles, leading to increased lung capacity and improved breathing efficiency. Regular exercise can help reduce the frequency and severity of asthma attacks, especially when incorporated into a comprehensive asthma management plan.
Structured Exercise Plan
A structured exercise plan should include a variety of activities to maintain interest and prevent boredom. Begin with a 5-10 minute warm-up, followed by 20-30 minutes of moderate-intensity exercise, and conclude with a 5-10 minute cool-down. Examples of activities include brisk walking, swimming, cycling, or yoga. Remember to listen to your body and adjust the intensity based on your individual response.
Warm-up and Cool-down Periods
Warm-up and cool-down periods are essential for asthma patients engaging in exercise. Warm-up periods prepare the body for increased exertion, reducing the risk of muscle strain and asthma symptoms. Cool-down periods allow the body to gradually return to a resting state, promoting recovery and preventing complications. These periods should be incorporated into every exercise session.
Low-Impact Exercises for Asthma Patients
Low-impact exercises are particularly beneficial for asthma patients due to their reduced stress on the respiratory system. These activities are suitable for individuals with varying fitness levels and can be easily incorporated into a daily routine.
| Exercise Type | Description | Benefits |
|---|---|---|
| Walking | A simple and accessible exercise, suitable for all fitness levels. | Excellent for cardiovascular health and burning calories. |
| Swimming | A low-impact exercise that involves minimal stress on joints. | Excellent for cardiovascular health and respiratory muscle strengthening. |
| Cycling | A low-impact exercise that involves rhythmic movement. | Excellent for cardiovascular health and burning calories. |
| Yoga | A series of postures and breathing exercises. | Improves flexibility, strength, and relaxation. Can help manage stress, which can trigger asthma. |
| Tai Chi | A series of slow, flowing movements. | Improves balance, coordination, and relaxation. |
Lifestyle Modifications and Weight Management
Managing weight effectively is crucial for anyone with asthma, and lifestyle modifications play a pivotal role in this process. By incorporating strategies for stress management, prioritizing sleep hygiene, and creating a supportive environment, individuals can significantly improve their asthma control and overall well-being. Understanding the interplay between environmental factors, sleep, and mental health is key to developing a comprehensive weight management plan tailored to the unique needs of asthma patients.Lifestyle choices significantly impact both asthma symptoms and weight.
Stress, poor sleep, and environmental factors can all exacerbate asthma and contribute to weight gain or loss. By actively managing these factors, individuals can improve their health outcomes and maintain a healthy weight. These strategies, when implemented consistently, can lead to a healthier and more balanced life for those living with asthma.
Stress Management Strategies
Stress can trigger asthma attacks and affect appetite regulation, potentially leading to weight fluctuations. Effective stress management techniques can help reduce both stress and its impact on asthma and weight. Practicing mindfulness, yoga, or deep breathing exercises can calm the nervous system, reducing the frequency and severity of asthma attacks. Regular physical activity, even moderate exercise, is also an effective stress reliever.
Maintaining a supportive social network can provide emotional comfort and reduce feelings of isolation. Finding healthy outlets for stress, like spending time in nature or pursuing hobbies, can be very beneficial.
Sleep Hygiene and its Impact
Adequate sleep is essential for both physical and mental health, and it plays a critical role in managing asthma. Sleep deprivation can weaken the immune system, making individuals more susceptible to asthma attacks. Poor sleep can also affect hormone regulation, which can influence appetite and metabolism, potentially contributing to weight gain. Establishing a consistent sleep schedule, creating a relaxing bedtime routine, and ensuring a dark, quiet, and cool sleep environment can improve sleep quality.
Avoiding caffeine and alcohol before bed, and ensuring regular exercise, are also helpful strategies.
Losing weight with asthma can be tricky, as certain exercise regimens might trigger symptoms. One crucial factor to consider is potential allergies, which can significantly impact your health journey. Understanding the differences between allergy blood tests and skin tests can help pinpoint any sensitivities affecting your overall well-being. Knowing if you have allergies can inform a personalized weight loss plan, which is tailored to your specific needs.
For a comprehensive comparison of allergy blood tests and skin tests, check out this resource: allergy blood test vs skin test. Ultimately, a balanced approach that incorporates exercise and a healthy diet, while managing asthma and any potential allergies, is key to successful weight loss.
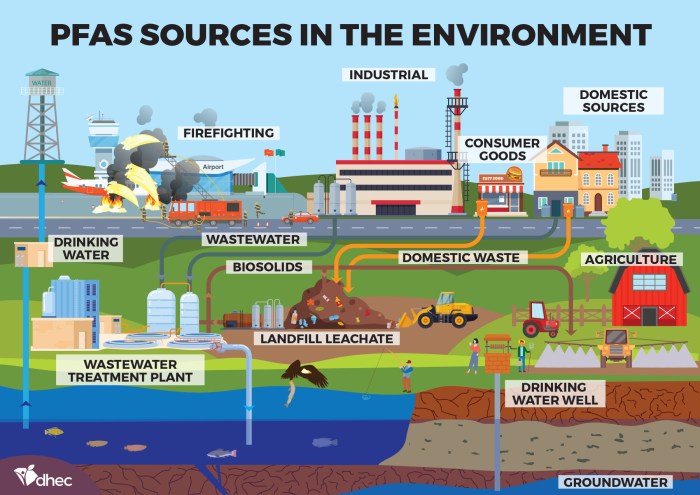
Environmental Factors and Asthma
Environmental factors like allergens, pollutants, and extreme temperatures can significantly impact asthma symptoms. Identifying and mitigating these triggers can improve asthma control. Regular cleaning to reduce dust mites, controlling pet dander, and using air purifiers can help manage indoor allergens. Minimizing exposure to outdoor pollutants, such as smog and smoke, and taking precautions during extreme weather conditions are also crucial.
Knowing your personal triggers and developing strategies to avoid or manage them is essential.
Losing weight with asthma can be tricky, but it’s definitely achievable! Finding the right balance of exercise and diet is key. Understanding potential digestive issues like IBS, which can sometimes mimic symptoms of colon cancer, is also important. You might want to check out this article on IBS vs colon cancer to get a better understanding of these conditions.
Ultimately, consulting with a doctor is crucial to develop a safe and effective weight loss plan that considers your specific asthma and overall health needs.
Creating a Supportive Environment
Building a supportive environment is key to successful weight management and asthma control. Encouraging a positive and healthy relationship with food and exercise is important. Encouraging open communication with healthcare providers, family members, and friends is essential for sharing concerns and creating a support system. Setting realistic goals and celebrating small victories can maintain motivation and encourage adherence to lifestyle changes.
Finding an exercise buddy or joining a support group can foster accountability and motivation.
Sleep Disorders and their Impact
| Sleep Disorder | Potential Impact on Asthma | Potential Impact on Weight |
|---|---|---|
| Sleep Apnea | Increased risk of asthma attacks, reduced lung function | Increased risk of weight gain due to hormonal imbalances and reduced metabolism |
| Insomnia | Increased risk of asthma attacks, decreased immune function | Increased risk of weight gain due to stress and hormonal imbalances |
| Restless Legs Syndrome | Disrupted sleep, potential for increased anxiety and stress, increasing the risk of asthma attacks | Potential for increased stress leading to weight gain or loss depending on coping mechanisms. |
| Narcolepsy | Increased risk of asthma attacks due to disrupted sleep patterns | Potential for both weight gain and loss due to unpredictable sleep patterns and energy levels |
Sleep disorders can significantly affect both asthma and weight management. Recognizing the potential impact of these disorders is critical in developing personalized strategies for better health.
Mental Health and Weight Management
Mental health plays a vital role in weight management and asthma control. Stress, anxiety, and depression can negatively affect both weight and asthma symptoms. Seeking professional help, such as therapy or counseling, is essential for managing mental health concerns. Developing coping mechanisms for stress, such as relaxation techniques, mindfulness, and spending time in nature, can be very effective.
Building a strong support system, connecting with others, and practicing self-care can also contribute to improved mental well-being. This can, in turn, help in maintaining a healthy weight and better managing asthma.
Medical Professional Involvement
Managing weight with asthma requires careful consideration of your individual needs. Consulting with healthcare professionals is crucial for developing a safe and effective plan that addresses both your asthma and weight goals. This approach ensures that any changes to your diet or exercise routine are tailored to your specific health conditions and that potential risks are minimized.A holistic approach to weight management for asthma patients necessitates a collaborative effort between the patient and their healthcare team.
This involves open communication, shared decision-making, and a commitment to ongoing monitoring and adjustments as needed. This ensures that your treatment plan evolves with your individual needs and responds to any changes in your health.
Finding healthy ways to lose weight with asthma can be tricky, but it’s definitely possible! One important supplement to consider is turmeric, and knowing the best time to take it can significantly impact its effectiveness. For example, research suggests that taking turmeric alongside your meals might maximize its absorption, just like other nutrients. Check out this helpful guide on best time to take turmeric to learn more.
Ultimately, a balanced diet and regular exercise, tailored to your asthma management plan, are key to sustainable weight loss for people with asthma.
Importance of Professional Consultation
Seeking guidance from healthcare professionals before altering your diet or exercise regimen is essential. This proactive step helps prevent unintended complications, ensures that any modifications are safe and beneficial for your overall health, and allows for personalized recommendations that consider your specific asthma triggers and sensitivities. By consulting with healthcare professionals, you gain a comprehensive understanding of how your chosen lifestyle changes will interact with your existing medical conditions.
Role of a Registered Dietitian
A registered dietitian (RD) plays a vital role in assisting individuals with asthma and weight management. They are trained to provide personalized dietary recommendations that consider the individual’s unique needs, including potential food sensitivities or allergies. RDs can also help patients identify and manage potential asthma triggers that may be hidden in certain foods or dietary patterns. They can tailor a meal plan that is not only supportive of weight loss or maintenance but also mindful of the individual’s specific asthma considerations.
Working with a Pulmonologist
Collaboration with a pulmonologist is essential for effective asthma management. Pulmonologists specialize in respiratory conditions and can provide expert guidance on managing asthma symptoms, including the impact of weight on respiratory function. They can assess the potential effects of weight loss or gain on asthma triggers, and recommend modifications to your treatment plan, if needed. Working with a pulmonologist ensures a coordinated approach that integrates your asthma management with your weight loss goals.
Questions to Ask a Doctor
| Category | Example Questions |
|---|---|
| Dietary Considerations | “Are there any specific foods or dietary patterns I should avoid due to my asthma?” “Can you recommend a registered dietitian who specializes in asthma and weight management?” |
| Exercise Recommendations | “What types of exercise are best for managing my asthma and weight?” “How can I safely increase my activity levels without exacerbating my asthma symptoms?” |
| Asthma Management | “How might my weight affect my asthma control?” “Are there any medications or therapies that might interact with my weight loss goals?” |
| Overall Health | “What are the potential health risks of rapid weight loss for someone with asthma?” “What is the recommended rate of weight loss to support my overall health and asthma control?” |
Effective Communication Strategies
Clear and open communication with healthcare professionals is vital for a successful partnership. Be prepared to provide detailed information about your asthma symptoms, medications, and any relevant medical history. Clearly articulate your weight management goals and concerns. Actively listen to the advice and recommendations provided, and ask clarifying questions to ensure you understand the plan. Regular follow-up appointments and proactive communication are essential for addressing any emerging issues or concerns.
Finding Support
Finding support groups or online communities for individuals with asthma and weight concerns can be incredibly beneficial. These platforms provide a supportive environment where individuals can share experiences, learn from others, and receive encouragement. Support groups offer valuable insights, coping strategies, and a sense of belonging for individuals navigating these challenges. Online forums can connect you with a broader network of individuals facing similar situations, and provide practical advice and shared experiences.
Potential Challenges and Solutions
Managing weight with asthma can be tricky. The medications, the need for careful activity levels, and the potential for underlying conditions all influence how we approach weight loss. Understanding the specific challenges and implementing effective solutions is key to achieving sustainable results.Weight management for individuals with asthma often faces unique obstacles. These challenges are not insurmountable, however, and with a comprehensive understanding and proactive strategies, progress is possible.
Identifying Potential Challenges
Asthma and weight management often clash. Medications for asthma can sometimes affect appetite or metabolism. The need to avoid strenuous activity due to exacerbations or lung function limitations can hinder the development of healthy habits. Underlying conditions like allergies or sensitivities can also complicate dietary choices. Recognizing these potential obstacles is the first step toward developing a tailored strategy.
Addressing Food Cravings and Emotional Eating, Ways to lose weight with asthma
Food cravings and emotional eating can derail weight loss efforts. These patterns are often deeply rooted in emotional or physiological needs. Understanding the triggers for these cravings and developing healthy coping mechanisms is essential. Techniques like mindful eating, stress management, and keeping a food journal can help identify patterns and create a more balanced approach. For example, recognizing a link between stress and sugary snacks can empower an individual to explore healthier stress-reducing alternatives.
Overcoming Barriers to Physical Activity
Physical activity is crucial for weight management, but individuals with asthma might face barriers due to exacerbations, fear of triggering symptoms, or limited lung capacity. A gradual approach to exercise, tailored to individual needs, is essential. Consulting with a doctor or respiratory therapist to establish a safe and effective exercise regimen is important. This personalized approach helps individuals safely incorporate physical activity into their routines.
For example, walking in short bursts, followed by rest periods, can be a suitable starting point.
Table of Common Barriers and Potential Solutions
| Barrier | Potential Solution |
|---|---|
| Medication side effects (e.g., increased appetite) | Communicate with a doctor to adjust medication or explore alternative options. |
| Fear of triggering asthma symptoms during exercise | Start with low-intensity activities, gradually increasing duration and intensity. Consult a healthcare professional for a personalized exercise plan. |
| Limited lung capacity | Prioritize activities that are less strenuous on the lungs. Focus on activities like walking, swimming, or cycling. Ensure proper breathing techniques are used during exercise. |
| Lack of time | Break down exercise into shorter, more manageable sessions throughout the day. Incorporate physical activity into daily routines, such as taking the stairs instead of the elevator. |
| Social factors (lack of support, lack of accessible facilities) | Seek out support groups or online communities for people with asthma and weight management goals. Find local parks or gyms that cater to individuals with respiratory conditions. |
Seeking Professional Support
Professional guidance is crucial for individuals with asthma who are seeking weight management. A registered dietitian specializing in respiratory conditions can provide tailored dietary advice. A physical therapist can help create a safe and effective exercise program. A doctor can monitor lung function and adjust medication as needed. This multidisciplinary approach ensures a holistic and supportive weight management plan.
Accountability Partners and Support Groups
Accountability partners or support groups can significantly boost motivation and provide encouragement. Sharing experiences, strategies, and successes with others facing similar challenges can foster a sense of community and support. Online forums or local support groups can provide valuable connections. This collective effort can help maintain consistency and motivation. For instance, sharing meals or working out together can make weight management goals more achievable.
Summary: Ways To Lose Weight With Asthma

In conclusion, managing weight with asthma requires a holistic approach that encompasses dietary choices, tailored exercise routines, and mindful lifestyle modifications. Remember that consistency and seeking professional guidance are essential for achieving sustainable results. By understanding the nuances of your condition and embracing these strategies, you can take control of your weight and asthma management, ultimately leading to a better quality of life.