Cool ways to stop hot flashes are crucial for managing discomfort during menopause. This guide explores various strategies, from lifestyle adjustments to alternative therapies and medical treatments, to help you navigate this common experience. We’ll delve into practical tips, like stress management techniques and dietary changes, alongside exploring alternative options like herbal remedies and acupuncture.
Understanding the interplay between lifestyle choices, environmental factors, and potential medical interventions is key. This comprehensive approach offers a range of solutions to help you find what works best for your individual needs and preferences.
Lifestyle Modifications: Cool Ways To Stop Hot Flashes
Managing hot flashes often involves more than just medication. Adopting healthy lifestyle changes can significantly reduce their frequency and intensity. These modifications work by addressing underlying factors contributing to the symptoms, like stress, poor sleep, and an unhealthy diet. A holistic approach that combines these elements can lead to a more comfortable and balanced life.Lifestyle modifications, such as stress management, improved sleep hygiene, and a balanced diet, can greatly impact the severity and frequency of hot flashes.
By addressing these lifestyle factors, individuals can often experience significant relief and improve their overall well-being.
Stress Management Techniques
Stress and anxiety can trigger hot flashes. Effective stress management strategies are crucial for minimizing their occurrence. Techniques like deep breathing exercises, meditation, and mindfulness practices can help regulate the body’s stress response, reducing the likelihood of a hot flash.
- Deep Breathing Exercises: Deep, slow breaths can calm the nervous system and lower heart rate. Incorporating these exercises into your daily routine can help reduce stress and its impact on hot flashes. For example, inhaling deeply through your nose for several seconds and exhaling slowly through your mouth for an equal duration can provide a calming effect.
- Mindfulness Meditation: Focusing on the present moment through meditation can help reduce anxiety and promote relaxation. Regular practice can lessen the frequency and intensity of hot flashes. Mindfulness techniques involve focusing on your breath, bodily sensations, or thoughts without judgment. This can help you become more aware of your body’s signals, allowing you to recognize and manage potential triggers.
- Progressive Muscle Relaxation: This technique involves tensing and releasing different muscle groups in the body. It helps reduce muscle tension and promote relaxation, potentially lessening the occurrence of hot flashes. This can be done by tensing a muscle group for a few seconds, holding it, and then releasing it, gradually working your way through the body.
Sleep Hygiene Strategies
Adequate sleep is essential for overall health and can significantly impact hot flashes. Poor sleep hygiene can increase their frequency and severity. Implementing good sleep habits can help regulate hormones and reduce the body’s stress response, thus reducing the occurrence of hot flashes.
Trying to beat those pesky hot flashes? It’s a common struggle, and thankfully, there are some surprisingly cool ways to combat them. Interestingly, just like the fascinating genetics of eye color, which you can explore further here: genetics of eye color , our bodies are complex systems. Staying hydrated and managing stress are key parts of a healthy approach to managing hot flashes.
- Consistent Sleep Schedule: Going to bed and waking up around the same time each day, even on weekends, helps regulate your body’s natural sleep-wake cycle. This regularity can lead to better sleep quality and fewer hot flashes.
- Creating a Relaxing Bedtime Routine: Establishing a calming bedtime routine, such as taking a warm bath, reading a book, or listening to calming music, can signal to your body that it’s time to wind down. This can improve sleep quality and potentially reduce the occurrence of hot flashes.
- Creating a Conducive Sleep Environment: Maintaining a cool, dark, and quiet bedroom environment can enhance sleep quality. Using blackout curtains, earplugs, or a white noise machine can create an ideal sleep environment.
Physical Activity and Hot Flashes
Regular physical activity can improve cardiovascular health and help regulate body temperature, potentially reducing the frequency and severity of hot flashes. Physical activity can also reduce stress, further contributing to the alleviation of hot flashes.
- Regular Exercise: Engaging in moderate-intensity exercise most days of the week can positively impact hot flashes. Activities like brisk walking, swimming, or cycling can contribute to better cardiovascular health and potentially lessen the intensity of hot flashes.
- Finding Activities You Enjoy: Choosing physical activities you find enjoyable makes it more likely that you will stick to a regular exercise routine. This consistency is crucial for reaping the benefits of exercise in reducing hot flashes.
Dietary Considerations
Diet plays a role in managing hot flashes. Certain foods and beverages can trigger or exacerbate them. A balanced diet, rich in fruits, vegetables, and whole grains, may help reduce the occurrence of hot flashes.
- Foods to Include: Focus on a diet rich in fruits, vegetables, and whole grains. These foods are packed with essential nutrients and can help regulate hormone levels. Include foods high in fiber, such as beans, lentils, and whole grains, for improved digestion and overall health.
- Foods to Avoid: Some foods, like spicy foods, caffeine, and alcohol, are often associated with triggering hot flashes. Reducing intake of these items can help minimize hot flash frequency and intensity.
Caffeine and Alcohol
Caffeine and alcohol can trigger or worsen hot flashes. Moderation is key. Reducing or eliminating these substances can often lessen the occurrence and severity of hot flashes.
- Caffeine Consumption: Limit or eliminate caffeine intake, especially in the later part of the day. Caffeine can interfere with sleep, increasing the risk of hot flashes.
- Alcohol Consumption: Limit or avoid alcohol, particularly in the evenings. Alcohol can disrupt sleep patterns and exacerbate hot flashes.
Relaxation Techniques
Different relaxation techniques can help manage hot flashes. The effectiveness of each method may vary based on individual experiences.
| Technique | Description | Effectiveness |
|---|---|---|
| Deep Breathing | Slow, deep breaths to calm the nervous system. | Generally effective for reducing immediate anxiety and stress-related hot flashes. |
| Meditation | Focusing on the present moment to reduce stress and anxiety. | Potentially effective for long-term management of hot flashes, especially those linked to anxiety. |
| Progressive Muscle Relaxation | Tensing and releasing muscle groups to reduce tension. | May reduce muscle tension and anxiety, indirectly affecting hot flash frequency. |
Alternative Therapies
Exploring alternative therapies for hot flashes can offer a holistic approach beyond traditional treatments. While these methods are not a replacement for medical advice, they can be complementary and potentially beneficial for managing symptoms. Many individuals find these practices helpful in managing the emotional and physical discomfort associated with hot flashes.Alternative therapies often focus on restoring balance within the body and mind, which may contribute to a reduction in hot flash frequency and severity.
This approach acknowledges the interconnectedness of physical and emotional well-being and aims to address the root causes of discomfort rather than just the symptoms themselves. However, it’s important to remember that these therapies are not scientifically proven to cure or eliminate hot flashes, and their effectiveness can vary greatly from person to person.
Herbal Remedies for Hot Flashes
Herbal remedies have been used for centuries to treat various ailments, and some herbs show promise in alleviating hot flashes. These remedies often work by influencing hormone levels or reducing inflammation.Examples include black cohosh, a plant traditionally used to regulate hormonal balance, and red clover, which may help reduce estrogen-related symptoms. However, the scientific evidence for their effectiveness in treating hot flashes is mixed.
Some studies show potential benefits, while others do not demonstrate a significant effect. It’s crucial to consult with a healthcare professional before using herbal remedies, as they can interact with other medications and may have potential side effects.
Acupuncture for Hot Flashes
Acupuncture, an ancient Chinese practice, involves inserting thin needles into specific points on the body. Proponents believe that acupuncture can restore the flow of “Qi” (vital energy) and balance the body’s energy meridians. Studies on acupuncture’s effectiveness in reducing hot flashes have produced varied results. While some studies show a potential reduction in hot flash frequency and severity, more robust research is needed to confirm these findings.
Acupuncture’s potential benefits may include stress reduction and improved overall well-being, which could indirectly contribute to symptom relief.
Mindfulness and Yoga for Hot Flash Management
Mindfulness practices, which involve focusing on the present moment, and yoga, with its emphasis on physical postures and breathing techniques, can significantly impact hot flash experiences. These practices help manage stress and anxiety, which can trigger or exacerbate hot flashes. Through regular practice, individuals may develop coping mechanisms to manage emotional responses to these sensations.By cultivating awareness and relaxation techniques, mindfulness and yoga can potentially reduce the frequency and intensity of hot flashes.
The stress-reducing effects of these practices may play a significant role in achieving symptom relief.
Aromatherapy and Essential Oils for Hot Flashes
Aromatherapy utilizes essential oils to promote well-being and address various health concerns. Specific essential oils are believed to have a calming effect on the body and mind, potentially reducing hot flash symptoms.Lavender oil, known for its calming properties, is frequently used in aromatherapy for hot flashes. Other potential options include chamomile, which has a soothing effect, and sandalwood, with its grounding aroma.
However, it’s important to note that the scientific evidence supporting the use of aromatherapy for hot flashes is limited. Consult a healthcare professional to determine the appropriate use of essential oils and potential risks.
Comparison of Alternative Therapies
| Therapy | Potential Benefits | Potential Drawbacks |
|---|---|---|
| Herbal Remedies | Potential to regulate hormones, reduce inflammation, and alleviate symptoms. | Potential interactions with medications, side effects, and inconsistent scientific evidence. |
| Acupuncture | Potential to improve energy flow and reduce stress, potentially leading to symptom relief. | Limited scientific evidence of effectiveness, potential for discomfort at insertion points. |
| Mindfulness/Yoga | Stress reduction, improved emotional regulation, and potential to modify physiological responses to hot flashes. | Requires consistent practice, may not be effective for all individuals. |
| Aromatherapy | Calming effect, potentially reducing anxiety and stress, which may alleviate symptoms. | Limited scientific evidence, potential allergic reactions to essential oils. |
Finding Qualified Practitioners
Finding qualified practitioners for alternative therapies is crucial to ensure safety and effectiveness.Consult your primary care physician for recommendations or explore online directories that list certified practitioners in your area. Look for practitioners with relevant experience and qualifications in the specific alternative therapy you are considering. It’s important to prioritize safety and efficacy when selecting practitioners for alternative treatments.
Medical Treatments

Medical treatments for hot flashes offer a range of options for managing symptoms. While lifestyle modifications and alternative therapies can provide relief, some individuals may benefit from medication to address the underlying hormonal imbalances or neurological pathways involved in hot flashes. Consulting with a healthcare professional is crucial to determine the most appropriate and effective treatment plan.Hormone replacement therapy (HRT) is a common approach, and various non-hormonal medications can also be considered.
Understanding the potential benefits and risks associated with each option is essential for informed decision-making.
Commonly Prescribed Medications
Various medications are used to treat hot flashes, and their effectiveness and side effects can vary significantly. Some commonly prescribed medications include certain types of hormone replacement therapy (HRT), selective serotonin reuptake inhibitors (SSRIs), and other options.
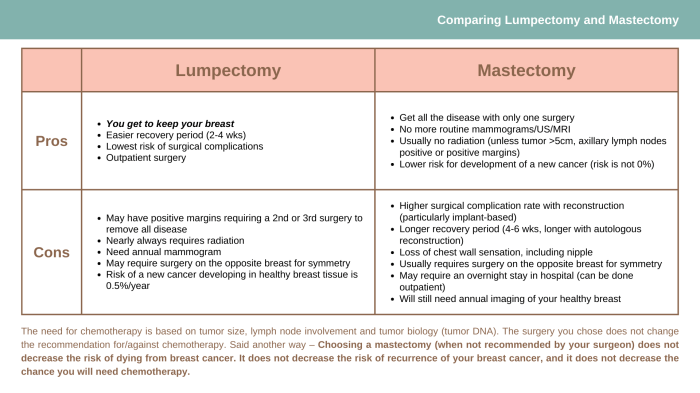
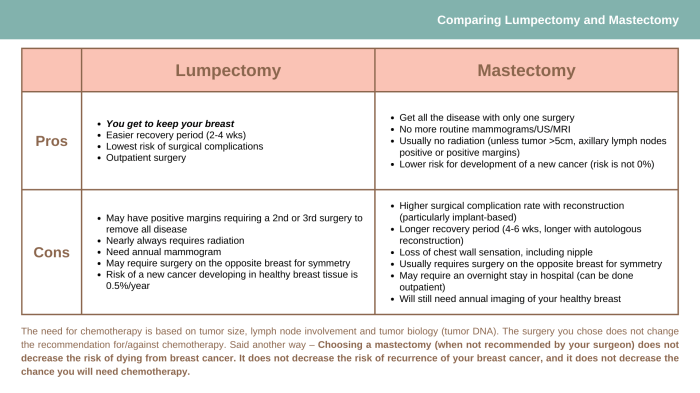
Finding cool ways to manage hot flashes can be a real lifesaver, especially when you’re navigating the complexities of health. Considering the various stages of care, like in planning for care in phases of metastatic breast cancer , is crucial. Staying proactive and exploring options like cool compresses or herbal remedies can help alleviate discomfort and improve overall well-being during this journey.
Ultimately, focusing on practical solutions for hot flashes remains important, regardless of the health situation.
Hormone Replacement Therapy (HRT)
Hormone replacement therapy (HRT) is a treatment option that aims to restore hormonal balance in the body. It can be particularly helpful in managing hot flashes associated with menopause. Different types of HRT use varying combinations of estrogen and progestin, and the choice depends on individual factors such as age, overall health, and medical history. Different formulations of HRT, such as oral, transdermal, or topical, can impact the effectiveness and side effect profiles.
Some examples of HRT include conjugated equine estrogens (CEE), estradiol, and various progestins.
Comparison of HRT Effectiveness
The effectiveness of different HRT formulations for managing hot flashes varies. For example, oral HRT may have a faster onset of action compared to transdermal HRT. However, transdermal HRT may be associated with fewer side effects, such as blood clots or increased risk of stroke, compared to oral HRT. The optimal choice depends on individual factors and should be discussed with a healthcare professional.
Non-Hormonal Medications
Non-hormonal medications, such as selective serotonin reuptake inhibitors (SSRIs), can also be used to manage hot flashes. SSRIs work by affecting neurotransmitters in the brain, potentially reducing the frequency and severity of hot flashes. However, these medications can have potential side effects, including nausea, headaches, and insomnia. Other non-hormonal medications include gabapentin and clonidine, which can also offer relief from hot flashes.
Potential Benefits and Risks of Medications
Each medication carries potential benefits and risks. For example, HRT can effectively reduce hot flashes but may increase the risk of certain health problems, such as blood clots and breast cancer. SSRIs can help manage hot flashes but may cause side effects like nausea or sleep disturbances. It’s crucial to weigh the potential benefits against the potential risks when considering any medication for hot flash management.
Summary Table of Medical Treatments
| Treatment | Potential Benefits | Potential Side Effects |
|---|---|---|
| Hormone Replacement Therapy (HRT) | Effective in reducing hot flashes, restoring hormonal balance | Increased risk of blood clots, stroke, breast cancer, other cardiovascular issues, and possible mood changes. |
| Selective Serotonin Reuptake Inhibitors (SSRIs) | May reduce hot flash frequency and severity | Nausea, headaches, insomnia, and other possible side effects. |
| Gabapentin | May reduce hot flashes, often used for nerve pain conditions | Drowsiness, dizziness, and other potential side effects. |
| Clonidine | Can reduce hot flashes, sometimes used for blood pressure issues | Drowsiness, dizziness, and other potential side effects. |
When to Consult a Doctor
If hot flashes significantly impact your daily life, disrupt sleep, or cause noticeable discomfort, consulting a healthcare professional is essential. Factors like the severity, frequency, and duration of hot flashes, as well as your overall health history, should be considered when seeking medical advice. A doctor can help assess the underlying cause of the hot flashes and recommend appropriate treatment options.
Environmental Strategies
Controlling your environment plays a crucial role in managing hot flashes. Understanding how temperature affects your body and making smart choices about your surroundings can significantly reduce the frequency and intensity of these episodes. By strategically adjusting your home and work environments, you can create a more comfortable and supportive atmosphere for yourself.Environmental factors significantly influence the likelihood and severity of hot flashes.
Exposure to heat, both externally and internally, can trigger these episodes. Conversely, cooler temperatures and environments can help mitigate the discomfort. By addressing these environmental elements, you can take proactive steps towards minimizing the impact of hot flashes on your daily life.
Impact of Temperature on Hot Flashes
Temperature fluctuations, both internal and external, can trigger or exacerbate hot flashes. Your body’s internal temperature regulation system can be thrown off balance by external heat, leading to discomfort. Maintaining a consistent and comfortable temperature, particularly in your home and workplace, is vital for managing hot flashes.
Adjusting Home and Work Environments
Maintaining a cool environment is key. Utilize air conditioning or fans strategically, ensuring adequate circulation. Consider using fans strategically in areas where you spend extended periods, such as your bedroom or office. Also, keeping windows closed during peak heat hours can maintain a cooler temperature inside. Regularly cleaning and maintaining your air conditioning system is essential for optimal efficiency and cooling.
Dressing Appropriately for Different Climates and Situations
Appropriate clothing choices can significantly influence your comfort level. During warmer months, opt for loose-fitting, light-colored, and breathable fabrics like cotton or linen. In cooler climates, layers of clothing allow you to adjust your temperature easily. Pay attention to the humidity levels in your environment; higher humidity can intensify hot flashes.
Utilizing Cooling Techniques
Implementing cooling techniques during hot flashes can provide immediate relief. A cool cloth placed on your neck or wrists can quickly reduce discomfort. Using a handheld fan directed at your body can also offer immediate relief. These methods can be effective in managing a hot flash episode in real-time.
Modifying Daily Routines to Avoid Triggers
Recognizing and avoiding potential triggers for hot flashes can help minimize their occurrence. For example, avoid strenuous activities during the hottest parts of the day. Taking regular breaks in a cool environment can also prevent overheating. Scheduling physical activities during cooler times can minimize discomfort.
Trying to beat those pesky hot flashes? It’s tough, but some simple tricks can help. Staying cool, like using a fan or a cool compress, can make a big difference. And, did you know what you eat can impact your symptoms? For example, understanding what to eat when you have mixed connective tissue disease what to eat when you have mixed connective tissue disease can be crucial.
Focus on a balanced diet and foods that are easy to digest to help keep your body comfortable. Ultimately, finding what works best for you in managing hot flashes is key. Experiment with different techniques to find your perfect cooling strategy.
Creating a Relaxing and Cool Environment During Hot Flashes
During a hot flash, creating a calming and cool environment can be crucial. Dimming lights and using soft music can promote relaxation. Taking a cool shower or bath can provide instant relief. If possible, lie down in a cool room, with light clothing on, and use fans to circulate air.
Cooling Techniques Effectiveness
| Cooling Technique | Effectiveness | Details |
|---|---|---|
| Cool cloth on neck/wrists | High | Quick relief, readily available |
| Handheld fan | Moderate | Helps with circulation, portable |
| Air conditioning | High | Maintains a consistent cool environment |
| Loose, light clothing | Moderate | Promotes breathability, reduces heat buildup |
| Cool shower/bath | Very High | Provides significant and rapid cooling |
Dietary Recommendations
Managing hot flashes often involves a multifaceted approach, and dietary choices play a significant role. Understanding which foods might exacerbate symptoms and which may offer support can be incredibly helpful in managing this common menopausal experience. This section delves into specific dietary strategies that can potentially help alleviate the frequency and intensity of hot flashes.
Foods That May Exacerbate Hot Flashes
Certain foods and beverages can trigger or worsen hot flashes in some individuals. These triggers can vary greatly from person to person. Common culprits often include caffeine-rich beverages, alcohol, spicy foods, and processed foods high in sugar and unhealthy fats.
- Caffeine: Coffee, tea, and chocolate can stimulate the nervous system, potentially increasing the likelihood of hot flashes. For individuals sensitive to caffeine, even small amounts can trigger a response.
- Alcohol: While some individuals may not experience a direct correlation, alcohol can disrupt hormonal balance and contribute to vasodilation, a key factor in hot flashes.
- Spicy Foods: Certain spices, such as chili peppers, can trigger a temporary increase in body temperature, which may manifest as a hot flash in susceptible individuals.
- Processed Foods: Processed foods often contain high levels of refined sugars and unhealthy fats. These can lead to blood sugar fluctuations and increased inflammation, which may contribute to hot flashes.
Foods That May Help Manage Hot Flashes
Certain foods are rich in nutrients that may help balance hormones and reduce inflammation. Incorporating these foods into your diet can be beneficial for managing hot flashes. These include foods rich in phytoestrogens, antioxidants, and healthy fats.
- Phytoestrogens: Soy products, flaxseeds, and lentils are excellent sources of phytoestrogens. These compounds mimic the effects of estrogen in the body, potentially mitigating some of the hormonal fluctuations that can trigger hot flashes.
- Antioxidants: Berries, leafy greens, and colorful fruits and vegetables are packed with antioxidants, which can help combat oxidative stress, a factor believed to be linked to hot flashes.
- Healthy Fats: Avocados, nuts, and seeds provide healthy fats that support hormone production and reduce inflammation, which can lessen the severity and frequency of hot flashes.
Hydration and Hot Flashes
Adequate hydration is crucial for overall health, and it plays a significant role in regulating body temperature. Staying well-hydrated can help prevent and manage hot flashes.
- Water Intake: Maintaining a consistent daily intake of water is essential for regulating body temperature and reducing the risk of dehydration, which can worsen hot flashes. Aim for at least 8 glasses of water daily. Adjust based on activity levels and climate.
Vitamins and Minerals
Certain vitamins and minerals may play a supportive role in reducing hot flash frequency. These include Vitamin D, magnesium, and B vitamins.
- Vitamin D: Studies suggest a link between vitamin D levels and hot flash frequency. A sufficient intake of Vitamin D might help alleviate hot flashes. Consult your doctor for recommendations.
- Magnesium: Magnesium plays a vital role in nerve and muscle function, and studies indicate that a magnesium deficiency might be linked to hot flashes. Include magnesium-rich foods in your diet, such as leafy greens, nuts, and seeds.
- B Vitamins: B vitamins are involved in numerous bodily functions, including hormone regulation. A balanced intake of B vitamins may contribute to better hormonal balance, which may help with hot flashes. Consume a varied diet including whole grains, legumes, and lean meats.
Sample Meal Plan
This sample meal plan provides a framework for incorporating foods that may help manage hot flashes. Adjust portion sizes and specific foods based on your individual needs and preferences.
| Meal | Description |
|---|---|
| Breakfast | Oatmeal with berries, nuts, and a drizzle of honey. |
| Lunch | Mixed green salad with grilled chicken or fish, avocado, and a light vinaigrette dressing. |
| Dinner | Lentil soup with whole-grain bread and a side salad. |
| Snacks | Fruits, vegetables, nuts, seeds, or a small handful of yogurt. |
Resources for Nutritionists
Locating a nutritionist specializing in menopause management can be beneficial for developing a personalized dietary plan. Online databases and healthcare providers can provide referrals. Be sure to verify credentials and experience before choosing a nutritionist.
Support Systems
Navigating the challenges of hot flashes can be emotionally taxing. Beyond the physical discomfort, many women experience feelings of isolation, frustration, and even embarrassment. Recognizing the emotional toll and actively seeking support can make a significant difference in managing these symptoms and overall well-being. A strong support network can provide a vital buffer against the negative impacts of hot flashes.Emotional support is crucial for women experiencing hot flashes.
These episodes can disrupt daily routines, affect relationships, and impact self-esteem. Having people who understand and empathize with the experience can significantly lessen the emotional burden. This support network can be comprised of family, friends, or even strangers who share similar experiences.
Importance of Emotional Support, Cool ways to stop hot flashes
The emotional toll of hot flashes extends beyond the immediate discomfort. The unpredictability and frequency of these episodes can lead to feelings of anxiety, frustration, and even depression. Emotional support helps manage these feelings by providing a safe space to express concerns and validate experiences.
Benefits of Support Groups and Online Communities
Connecting with others who understand the experience of hot flashes offers significant advantages. Support groups and online communities provide a safe and supportive environment to share experiences, strategies, and coping mechanisms. These groups offer a sense of community and belonging, fostering understanding and reducing feelings of isolation.
Strategies for Communicating with Loved Ones
Open communication with loved ones about hot flashes is essential. Explaining the symptoms, the impact they have on daily life, and the need for support is key. Using clear and direct language, focusing on the impact rather than the inconvenience, and seeking understanding rather than judgment can be helpful. Emphasizing the need for empathy and practical support can foster a stronger understanding.
Seeking Professional Help
If emotional or mental health challenges related to hot flashes arise, seeking professional help is a crucial step. A therapist or counselor can provide support, coping strategies, and guidance to address underlying anxieties or emotional distress. Addressing these concerns can be vital in managing the overall experience and improving quality of life.
Resources for Support Groups and Online Communities
- National Institutes of Health (NIH): The NIH website often provides links to relevant support groups and resources for various health conditions, including menopause.
- Mayo Clinic: This renowned medical institution may have information on support groups or resources related to menopause and hot flashes.
- Local community centers: Check with local community centers or senior centers for support groups or workshops related to women’s health.
- Online forums and social media groups: Search for online forums and social media groups focused on menopause, women’s health, or hot flashes.
Building a Strong Support Network
Building a strong support network involves proactive steps. Reach out to friends, family, and trusted individuals to share your experiences. Participate in support groups or online communities to connect with others facing similar challenges. Actively listen to and validate the experiences of others, and reciprocate the support you receive. This process strengthens relationships and builds a network of understanding and empathy.
Ultimate Conclusion
In conclusion, managing hot flashes involves a multifaceted approach. By combining lifestyle modifications, exploring alternative therapies, considering medical treatments, and implementing smart environmental strategies, you can significantly reduce the frequency and severity of these episodes. Remember that a personalized approach tailored to your specific needs and preferences is essential for optimal results. This guide provides a wealth of information, but remember that consulting a healthcare professional is always recommended.