Is diet soda bad for you? This question is at the forefront of many conversations about health and wellness. While diet soda often presents itself as a healthier alternative to sugary drinks, the truth is more complex than a simple yes or no. This post explores the potential health impacts of diet soda, delving into the science behind artificial sweeteners and comparing it to regular soda.
We’ll examine the effects on different demographics and offer healthier alternatives for those seeking a refreshing and responsible beverage choice.
The potential negative health effects of diet soda consumption are multifaceted, ranging from metabolic issues to potential interactions with gut microbiota. We’ll explore the different mechanisms through which artificial sweeteners might impact metabolic health, and how these effects compare to the risks associated with regular soda. This includes a detailed analysis of the nutritional profiles of various diet sodas and the potential long-term consequences of regular consumption on different bodily systems.
We’ll also consider the role of artificial sweeteners, the different types used, and their potential metabolic effects. Furthermore, we’ll present a range of healthier alternatives, moderation strategies, and considerations for specific demographics.
Health Impacts of Diet Soda
Diet soda, marketed as a healthier alternative to sugary sodas, has become increasingly popular. However, its long-term effects on health are still a subject of ongoing research and debate. While proponents claim it helps manage calorie intake and reduce sugar consumption, potential negative consequences for metabolic health and other bodily systems are a significant concern. This discussion delves into the potential health impacts of diet soda, exploring the mechanisms of artificial sweeteners and comparing them to regular soda.The consumption of diet soda, despite its lower calorie content compared to regular soda, may not be as beneficial as initially perceived.
The artificial sweeteners present in diet soda can exert various effects on the body, and these effects are not fully understood. Potential negative impacts on metabolic health, gut microbiome, and even mental well-being require further investigation and awareness.
Potential Negative Health Effects
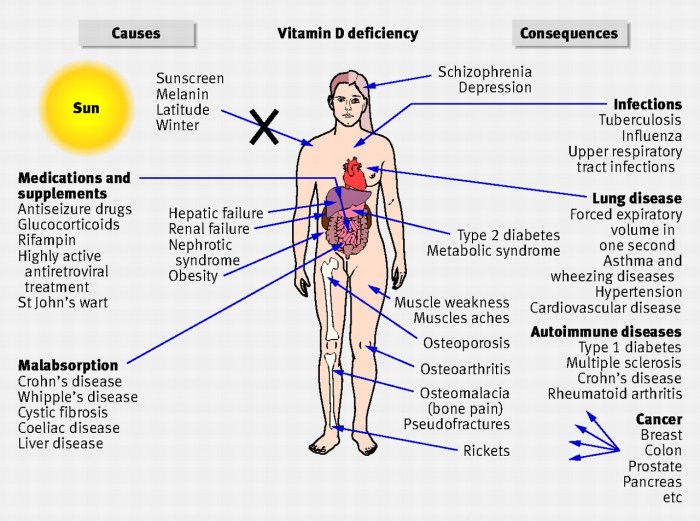
Artificial sweeteners, the primary components of diet soda, can have varied impacts on metabolic health. Some studies suggest a correlation between artificial sweetener consumption and an increased risk of metabolic syndrome, weight gain, and type 2 diabetes. The exact mechanisms behind these associations remain unclear, but potential disruptions in gut microbiome function, hormonal imbalances, and altered insulin sensitivity are possible contributing factors.
Mechanisms of Artificial Sweeteners on Metabolic Health
Artificial sweeteners, despite their low calorie count, may interfere with the body’s natural metabolic processes. One potential mechanism involves the disruption of the gut microbiome. Studies indicate that artificial sweeteners can alter the balance of beneficial and harmful bacteria in the gut, potentially impacting nutrient absorption and energy regulation. Furthermore, some artificial sweeteners might trigger cravings for sugary foods, ultimately counteracting the intended weight management benefits.
So, is diet soda bad for you? It’s a tricky question, and the answer might surprise you. While it’s often touted as a healthier alternative to regular soda, the potential long-term effects on your body are still being studied. Understanding how different types of pain, like somatic vs visceral pain, might be connected to your overall health is key here.
For example, differences in feeling somatic vs visceral pain can stem from various factors, and the impact of artificial sweeteners in diet soda is definitely worth exploring. Ultimately, it’s best to discuss any health concerns with a medical professional before making significant dietary changes.
Diet Soda vs. Regular Soda: Health Risks
Regular soda, laden with sugar, is associated with a higher risk of various health problems, including type 2 diabetes, heart disease, and obesity. Diet soda, while avoiding sugar, may still present its own set of risks, potentially impacting metabolic health in different ways. The key difference lies in the different mechanisms by which these drinks impact the body.
Regular soda’s sugar content directly affects blood sugar levels, whereas diet soda’s artificial sweeteners might indirectly affect metabolism and gut health.
Long-Term Consequences of Diet Soda Consumption, Is diet soda bad for you
Regular consumption of diet soda may lead to long-term health consequences across various bodily systems. Potential issues include disruptions in gut microbiome balance, potentially impacting nutrient absorption and immune function. Furthermore, consistent intake might be linked to an increased risk of metabolic disorders. The long-term impact of artificial sweeteners on the body is still a subject of research, but the possibility of adverse effects cannot be entirely ruled out.
Nutritional Profile Comparison of Diet Sodas
| Diet Soda Brand | Calories (per serving) | Sugar Content (grams) | Artificial Sweetener(s) | Sodium (mg) |
|---|---|---|---|---|
| Diet Coke | 0 | 0 | Aspartame | 40 |
| Diet Pepsi | 0 | 0 | Aspartame | 45 |
| Diet Dr. Pepper | 0 | 0 | Acesulfame potassium | 35 |
| Zero Sugar Coca-Cola | 0 | 0 | Sucralose | 42 |
Note: Nutritional information may vary depending on the specific product and serving size.
Potential Health Risks and Likelihood
| Level of Diet Soda Consumption | Potential Health Risks | Likelihood |
|---|---|---|
| Occasional Consumption | Minor metabolic shifts, minimal impact on gut health | Low |
| Regular Consumption (1-2 cans/day) | Potential for disrupted gut microbiome, minor weight gain concerns | Moderate |
| High Consumption (more than 2 cans/day) | Increased risk of metabolic disorders, possible link to mental health issues | High |
Note: This table is for illustrative purposes only and should not be considered medical advice. Individual responses to diet soda may vary.
Artificial Sweeteners and the Body
Artificial sweeteners, ubiquitous in diet soda and other processed foods, offer a tempting alternative to sugar. However, their impact on the body is complex and not entirely understood. While they provide a sugar-free option, the long-term effects on metabolic health, gut microbiome, and appetite regulation are subjects of ongoing research. This exploration delves into the different types of artificial sweeteners, their potential health impacts, and the scientific evidence surrounding them.Artificial sweeteners are synthetic compounds designed to provide a sweet taste without the calories of sugar.
So, is diet soda bad for you? While the lack of sugar might seem appealing, the artificial sweeteners in many diet sodas are still a bit of a mystery. Research is ongoing, and some studies suggest a potential link between excessive consumption and health issues, including a possible correlation with certain cancers, like triple negative breast cancer. Triple negative breast cancer is aggressive, and understanding the factors contributing to its development is critical.
Ultimately, moderation is key, and focusing on a balanced diet, rich in whole foods, is always the best approach when considering your overall well-being. So, while a diet soda might be a small part of your daily routine, it’s good to think about its place in a healthy lifestyle.
They are categorized into various chemical classes, each with unique properties and potential effects on the body. Understanding these different types and their mechanisms of action is crucial for assessing their potential risks and benefits.
Types of Artificial Sweeteners
Artificial sweeteners come in diverse chemical structures, each with a different mechanism for binding to taste receptors and triggering the sensation of sweetness. Some are intensely sweet, requiring only a small amount to achieve a comparable effect to sugar. This difference in sweetness levels can influence how they are used in food products and affect consumption patterns.
- Aspartame is a dipeptide ester composed of two amino acids, aspartic acid, and phenylalanine, joined with a methyl ester group. Its chemical formula is C 14H 18N 2O 5. Aspartame is one of the most commonly used artificial sweeteners, known for its high sweetness relative to sugar.
- Sucralose is a chlorinated sugar molecule. Its chemical formula is C 12H 19Cl 3O 8. Sucralose is derived from sucrose and is approximately 600 times sweeter than sugar.
- Saccharin is a sulfonamide derivative. Its chemical formula is C 7H 5NO 3S. Saccharin’s sweetness is relatively strong, and it is often used in various food products.
- Acesulfame potassium (Ace-K) is a sulfonylurea derivative. Its chemical formula is C 4H 4KNO 4S. Ace-K is also intensely sweet and has a wide range of applications in food products.
Scientific Evidence on Safety and Effectiveness
Extensive research has been conducted on the safety of artificial sweeteners, and numerous studies have examined their effectiveness in reducing calorie intake. While some studies suggest potential associations with negative health outcomes, the scientific consensus remains that artificial sweeteners, when used in moderation, are generally safe for consumption. The FDA has set Acceptable Daily Intake (ADI) levels for each sweetener, representing the maximum amount considered safe for daily consumption.
Metabolic Effects of Artificial Sweeteners
The metabolic effects of artificial sweeteners are a key area of ongoing investigation. Some studies suggest potential associations between artificial sweetener consumption and altered glucose metabolism, insulin sensitivity, and the risk of metabolic disorders. However, the evidence is not conclusive, and the underlying mechanisms are still under investigation.
Interactions with Gut Microbiota
The gut microbiome plays a crucial role in overall health. Some research indicates that artificial sweeteners might alter the composition and function of the gut microbiota, potentially leading to shifts in microbial diversity and impacting metabolic processes. However, more research is needed to definitively understand these interactions.
Influence on Appetite Regulation
Studies exploring the effect of artificial sweeteners on appetite regulation have yielded mixed results. Some research suggests that artificial sweeteners may impact satiety signals, leading to changes in food intake. However, the magnitude and consistency of these effects are not always clear.
Influence on Insulin Sensitivity and Blood Sugar Levels
Some studies have reported potential associations between artificial sweetener consumption and insulin resistance, potentially contributing to impaired glucose tolerance. The exact mechanisms and the extent of these effects remain a subject of ongoing debate.
Potential Health Impacts Table
| Artificial Sweetener | Potential Health Impacts (Note: Research is ongoing and findings are varied) |
|---|---|
| Aspartame | Potential effects on neurotransmitter function, though generally considered safe in moderation. |
| Sucralose | Some studies suggest possible associations with gut microbiome alterations, but more research is needed. |
| Saccharin | Possible links to bladder cancer, although evidence remains controversial. |
| Acesulfame Potassium | Limited research on long-term health effects, but generally considered safe. |
Alternatives and Moderation
Switching from diet soda to healthier options is a gradual process, not a sudden overhaul. This transition involves understanding the available alternatives, developing strategies for reducing consumption, and appreciating the nutritional differences between beverages. A balanced approach that prioritizes hydration and mindful choices is key to long-term well-being.A significant step towards a healthier lifestyle involves replacing diet soda with more nutritious alternatives.
This shift not only reduces potential health risks associated with artificial sweeteners but also allows for the enjoyment of beverages that contribute positively to overall well-being. Embracing moderation and understanding the nutritional value of different drinks are crucial elements in this transition.
Healthier Alternatives to Diet Soda
Replacing diet soda with healthier alternatives is a vital aspect of a balanced lifestyle. These options provide hydration and flavor without the artificial ingredients often found in diet soda.
- Infused Water: Water infused with fruits and herbs provides a refreshing and flavorful alternative to soda. Lemon, cucumber, berries, mint, and ginger are popular choices. These infusions enhance the taste of water while offering vitamins and antioxidants naturally present in the chosen fruits or herbs. Furthermore, these natural flavors are appealing and can help curb the desire for sugary drinks.
- Sparkling Water: Sparkling water, available in various flavors, provides a bubbly alternative to soda without added sugar. This option is a great choice for those craving the carbonation of soda. It’s crucial to opt for varieties without artificial sweeteners or added sugar.
- Unsweetened Tea: Unsweetened herbal or black tea can satisfy the craving for a warm or cold beverage. Black tea offers antioxidants, while herbal teas offer diverse flavor profiles without added sugar or artificial ingredients. Choose varieties without added sugars or artificial sweeteners.
- Freshly Squeezed Fruit Juices (in moderation): Freshly squeezed fruit juices, in moderation, can offer a burst of flavor and vitamins. However, be mindful of their sugar content, as natural sugars can still contribute to a significant intake. Consider diluting them with water or choosing low-sugar options.
Strategies for Reducing Diet Soda Consumption
Gradually reducing diet soda consumption is a more effective approach than abrupt cessation. This process involves replacing soda with healthier alternatives and establishing a routine.
- Gradual Reduction: Instead of eliminating diet soda entirely, reduce consumption gradually. Replace one or two servings per week with a healthier alternative. This approach makes the transition less challenging and more sustainable.
- Mindful Consumption: Pay attention to when and why you drink diet soda. Identifying triggers can help you develop strategies to avoid reaching for it. This awareness allows for a more informed approach to beverage choices.
- Hydration First: Prioritize drinking water throughout the day. Keeping yourself hydrated can help reduce cravings for sugary drinks.
- Keep Healthy Alternatives Handy: Having healthier options readily available can make it easier to choose them over diet soda when cravings arise. This proactive approach is beneficial for making informed choices.
Nutritional Value and Health Impacts of Different Beverages
Understanding the nutritional value and health impacts of various beverages is crucial for making informed choices. This knowledge helps in creating a balanced diet that incorporates beverages responsibly.
| Beverage | Nutritional Information (approximate) | Health Benefits |
|---|---|---|
| Water | Zero calories, no sugar, essential for hydration | Supports bodily functions, aids digestion, regulates body temperature |
| Infused Water | Zero to minimal calories, vitamins/minerals from fruits/herbs | Hydration, antioxidants, enhanced flavor, potential vitamins/minerals |
| Sparkling Water | Zero calories, no sugar, carbonation | Hydration, alternative to carbonated drinks |
| Unsweetened Tea | Low in calories, antioxidants | Antioxidant properties, potential health benefits associated with specific types (e.g., green tea) |
| Freshly Squeezed Fruit Juice (in moderation) | Natural sugars, vitamins, minerals | Vitamins, minerals, but watch portion sizes |
| Diet Soda | Zero to very low calories, artificial sweeteners | Potential health risks associated with artificial sweeteners, lack of essential nutrients |
Moderation is key in beverage consumption, regardless of the type.
Designing a Balanced Diet with Beverages
A balanced diet that incorporates beverages responsibly focuses on hydration, flavor, and overall health. This approach emphasizes the importance of making informed choices about beverage intake.
While diet soda might seem like a healthier alternative, it’s definitely a tricky one. There are some concerns about its impact on your overall health. But, if you’re looking for a naturally sweet and refreshing beverage option, exploring the health benefits of traditional Indonesian drinks like health benefits jamu drink might be a good idea.
Ultimately, a balanced diet and mindful choices are key to a healthy lifestyle, even when considering seemingly innocuous beverages like diet soda.
- Prioritize Water: Water should form the cornerstone of your daily beverage intake. It’s essential for bodily functions and plays a vital role in a healthy diet.
- Variety is Key: Incorporate a variety of healthier beverages to maintain flavor and ensure a diverse intake of nutrients. This approach provides essential nutrients and avoids monotony.
- Portion Control: Be mindful of portion sizes, especially with beverages that contain natural sugars, to manage calorie intake.
- Listen to Your Body: Pay attention to your body’s signals and adjust your beverage choices accordingly. This awareness allows for a personalized approach to hydration and nourishment.
Specific Populations and Considerations
Diet soda, despite its zero-calorie promise, can have varying effects on different population groups. Understanding these nuances is crucial for making informed choices about consumption. Factors like age, health conditions, and lifestyle significantly impact how diet soda affects individuals. This section will delve into the potential impacts on pregnant women, children, individuals with pre-existing conditions, athletes, and different age groups.
Impact on Pregnant Women
Pregnant women need to be particularly cautious about their diet soda intake. The artificial sweeteners used in diet sodas can potentially disrupt the delicate hormonal balance during pregnancy. Limited research exists, but some studies suggest a possible link between artificial sweetener consumption and adverse pregnancy outcomes, such as gestational diabetes. However, more robust research is needed to fully understand the connection.
Consult with a healthcare professional for personalized advice on diet soda consumption during pregnancy.
Impact on Children
Children are another vulnerable population regarding diet soda consumption. Their developing bodies and metabolic systems are particularly sensitive to the effects of artificial sweeteners and the potential negative impact on dental health. Frequent consumption can contribute to the development of cavities and erode tooth enamel. Furthermore, excessive consumption might disrupt healthy eating habits, potentially impacting their overall nutritional intake.
Encouraging healthy hydration through water and other nutritious beverages is recommended.
Impact on Individuals with Pre-existing Conditions
Individuals with pre-existing conditions like diabetes or obesity need to be extremely mindful of diet soda consumption. While diet soda offers a lower calorie option, it might still affect blood sugar levels in individuals with diabetes. The artificial sweeteners, though not providing calories, can still impact insulin sensitivity and blood sugar control. Additionally, for those with obesity, substituting regular soda with diet soda might not necessarily lead to weight loss.
This is because the potential impact on metabolism and appetite regulation is still an area of ongoing research. Consult with a healthcare professional or registered dietitian for personalized guidance.
Impact on Athletes and Individuals Engaging in Intense Physical Activity
Athletes and individuals engaged in intense physical activity might experience different effects from diet soda consumption. The artificial sweeteners may not impact hydration, but some studies suggest that they can potentially interfere with the body’s ability to use carbohydrates during exercise. This could potentially impact performance. Moreover, the overall impact on fluid balance and electrolyte regulation needs further investigation.
Water and electrolyte-rich beverages may be more suitable for optimal hydration and performance.
Considerations for Different Age Groups and Stages of Life
The influence of diet soda on different age groups and life stages varies. Teenagers and young adults may be more susceptible to developing unhealthy eating habits due to the perceived convenience and taste of diet soda. Older adults, with potential health conditions or dietary restrictions, should also be mindful of the potential impacts. Consult with a healthcare professional for personalized recommendations.
Approaching Diet Soda Consumption with Consideration for Specific Demographics
Instead of outright banning diet soda, a more nuanced approach should be taken. For example, limiting consumption for pregnant women and children is crucial. For individuals with pre-existing conditions, moderation and careful monitoring of blood sugar levels is recommended. Athletes might benefit from opting for water or electrolyte-rich beverages during intense physical activity. A personalized approach, taking into account individual health needs and lifestyle, is essential.
Potential Risks and Benefits for Various Population Groups
| Population Group | Potential Risks | Potential Benefits |
|---|---|---|
| Pregnant Women | Possible disruption of hormonal balance; potential adverse pregnancy outcomes (limited research). | Lower calorie option compared to regular soda. |
| Children | Potential for cavities and tooth enamel erosion; disruption of healthy eating habits. | Lower calorie option compared to regular soda. |
| Individuals with Pre-existing Conditions (Diabetes, Obesity) | Potential impact on blood sugar levels and insulin sensitivity; not necessarily leading to weight loss. | Lower calorie option compared to regular soda. |
| Athletes/Intense Physical Activity | Potential interference with carbohydrate use during exercise; impact on fluid balance and electrolyte regulation (limited research). | Lower calorie option compared to regular soda. |
| Different Age Groups/Life Stages | Potential for developing unhealthy eating habits. | Lower calorie option compared to regular soda. |
Research and Evidence

Unraveling the truth behind diet soda’s health impacts requires a deep dive into the scientific literature. The effects aren’t always straightforward, and the research often reveals nuanced relationships. This section delves into the methodologies, findings, and conclusions of key studies on diet soda consumption and its association with various health outcomes.The scientific community employs diverse methodologies to investigate the complex relationship between diet soda and health.
Observational studies, which track large populations over time, can identify correlations but cannot definitively prove causation. Intervention studies, on the other hand, can manipulate variables and assess the direct impact of diet soda consumption, but these are often limited by ethical considerations and practical constraints. Understanding these methodologies is crucial for interpreting the research findings accurately.
Recent Research on Diet Soda Consumption
A variety of studies have examined the link between diet soda consumption and health markers. Some studies suggest a correlation between regular diet soda intake and increased risk of certain health problems, while others find no significant association. The variability in results highlights the complexity of the issue. This disparity is further compounded by the diversity of methodologies employed in different studies.
Peer-Reviewed Studies Investigating Diet Soda and Health
Numerous peer-reviewed studies have investigated the relationship between diet soda consumption and various health outcomes. These studies employ different methodologies, resulting in diverse findings.
Methodologies Used in Relevant Studies
Observational studies often track large cohorts of individuals, documenting their diet soda consumption and monitoring health outcomes over extended periods. These studies can identify correlations but cannot establish causality. Intervention studies, on the other hand, might randomly assign participants to either a diet soda group or a control group. This allows researchers to observe the direct impact of diet soda consumption.
Meta-analyses combine data from multiple studies to provide a broader perspective on the overall evidence.
Comparison and Contrast of Research Approaches
Observational studies are useful for identifying potential associations but are prone to confounding variables. For example, individuals who consume diet soda might also have other lifestyle factors that influence their health outcomes. Intervention studies, while capable of establishing causality, often involve smaller sample sizes and may not fully reflect real-world conditions. Meta-analyses offer a more comprehensive view by aggregating data from multiple studies, but their interpretation can still be influenced by the quality and consistency of the included studies.
Key Findings and Conclusions of These Studies
Studies have produced varied results regarding the relationship between diet soda and health. Some studies suggest a correlation with increased risk of metabolic syndrome, type 2 diabetes, and cardiovascular disease. Other studies have found no significant association or even suggest potential protective effects in certain contexts. These differing conclusions highlight the need for more comprehensive research and further investigation into the underlying mechanisms.
Key Studies and Findings Table
| Study | Methodology | Key Findings | Conclusions |
|---|---|---|---|
| Study 1 (Example) | Observational, cohort study | Positive correlation between high diet soda consumption and increased risk of type 2 diabetes. | Suggests a potential link, but further research is needed to confirm causality. |
| Study 2 (Example) | Intervention, randomized controlled trial | No significant difference in weight gain between diet soda and water groups. | Diet soda consumption, in this study, did not show a direct link to weight gain. |
| Study 3 (Example) | Meta-analysis | Mixed results; some studies showed a correlation with adverse health outcomes, others did not. | The evidence is inconclusive and more research is required to draw a definitive conclusion. |
Conclusive Thoughts: Is Diet Soda Bad For You

In conclusion, the question of whether diet soda is bad for you doesn’t have a simple answer. While it may seem like a healthier option, the potential downsides, particularly regarding metabolic health and potential interactions with the body’s systems, are significant. This exploration highlights the importance of moderation and a balanced approach to beverage consumption. Considering healthier alternatives, and being mindful of the specific needs of different demographics, is crucial.
Ultimately, making informed choices about our beverage intake is key to maintaining overall well-being.