Problems showering chronic fatigue syndrome are a significant hurdle for many individuals living with this debilitating condition. The simple act of bathing can become a major challenge due to the complex interplay of physical limitations, emotional distress, and environmental factors. This detailed exploration delves into the multifaceted nature of these difficulties, providing practical solutions, environmental considerations, and strategies for long-term management.
This article examines the specific physical limitations that affect showering, such as fatigue, pain, and mobility issues, along with the emotional and psychological toll these challenges take. We’ll also explore various practical solutions, adaptive equipment, and bathroom modifications to make showering more accessible and manageable. Finally, we’ll cover the importance of hygiene, safety, and creating a personalized showering plan to improve the overall experience.
Understanding the Challenge
Living with chronic fatigue syndrome (CFS) presents numerous daily challenges, and the seemingly simple act of showering can become a significant hurdle. The physical and emotional toll of this condition often impacts routine hygiene practices, highlighting the need for understanding and support. Many individuals with CFS find that even basic tasks, like showering, require significant effort and planning.
Physical Limitations in Showering
Individuals with CFS frequently experience a range of physical limitations that make showering difficult. Fatigue is a primary concern, often leading to a complete lack of energy to initiate or complete the task. Musculoskeletal pain, such as muscle aches and joint stiffness, can make movement challenging, and even the simple act of reaching for a soap or shampoo can become painful.
Mobility issues, including difficulty getting into and out of the shower, can also pose significant obstacles. These factors combine to make showering a demanding and often overwhelming experience.
Emotional and Psychological Impact
Beyond the physical limitations, the emotional and psychological toll of struggling with showering is substantial. The frustration of not being able to maintain personal hygiene can lead to feelings of isolation and inadequacy. The inability to participate in a routine activity that most people take for granted can contribute to feelings of powerlessness and a diminished sense of self-worth.
The constant effort and planning required for showering can also lead to increased stress and anxiety.
Impact on Daily Hygiene Routines
The difficulties associated with showering have a ripple effect on daily hygiene routines. Individuals with CFS may struggle to maintain adequate hygiene, potentially leading to further health complications and social isolation. Delayed or infrequent showering can also impact self-esteem and confidence. The need for adjustments and accommodations to showering routines can be a significant burden, requiring considerable planning and effort.
Furthermore, the emotional and mental strain of this difficulty can impact other aspects of their lives.
Symptom-Specific Impact on Showering
| Symptom Type | Description | Impact on Showering |
|---|---|---|
| Fatigue | Extreme tiredness, often overwhelming and persistent. | Inability to initiate or complete showering, feeling drained even after brief efforts. May require significant rest periods between steps. |
| Musculoskeletal Pain | Aches and stiffness in muscles and joints, varying in intensity. | Difficulty reaching for items, moving around in the shower, or supporting oneself. Pain can be exacerbated by the movement required. |
| Mobility Issues | Difficulties with movement, balance, or transferring between positions. | Challenges entering and exiting the shower, maintaining balance, and completing tasks while seated or standing. May require assistance or specialized equipment. |
| Cognitive Impairment | Difficulty with concentration, memory, or processing information. | Forgetting steps in the routine, feeling overwhelmed by the complexity of the task, or needing increased time to complete it. |
Practical Solutions and Adaptations
Navigating daily tasks, especially hygiene routines, can be incredibly challenging for individuals living with chronic fatigue syndrome (CFS). Showering, often a simple chore for many, can become a significant hurdle due to the fatigue, pain, and other symptoms associated with CFS. This section explores practical solutions and adaptations designed to make showering more manageable and less burdensome.
Implementing these strategies can significantly improve the overall well-being and quality of life for people with CFS. By understanding the specific challenges and utilizing appropriate aids and modifications, showering can be transformed from a source of stress into a more comfortable and accessible experience.
Showering Aids and Equipment
A wide array of showering aids and equipment can be incredibly beneficial in alleviating the physical demands and discomfort associated with showering for individuals with CFS. These aids can reduce the need for strenuous movements, minimizing fatigue and pain.
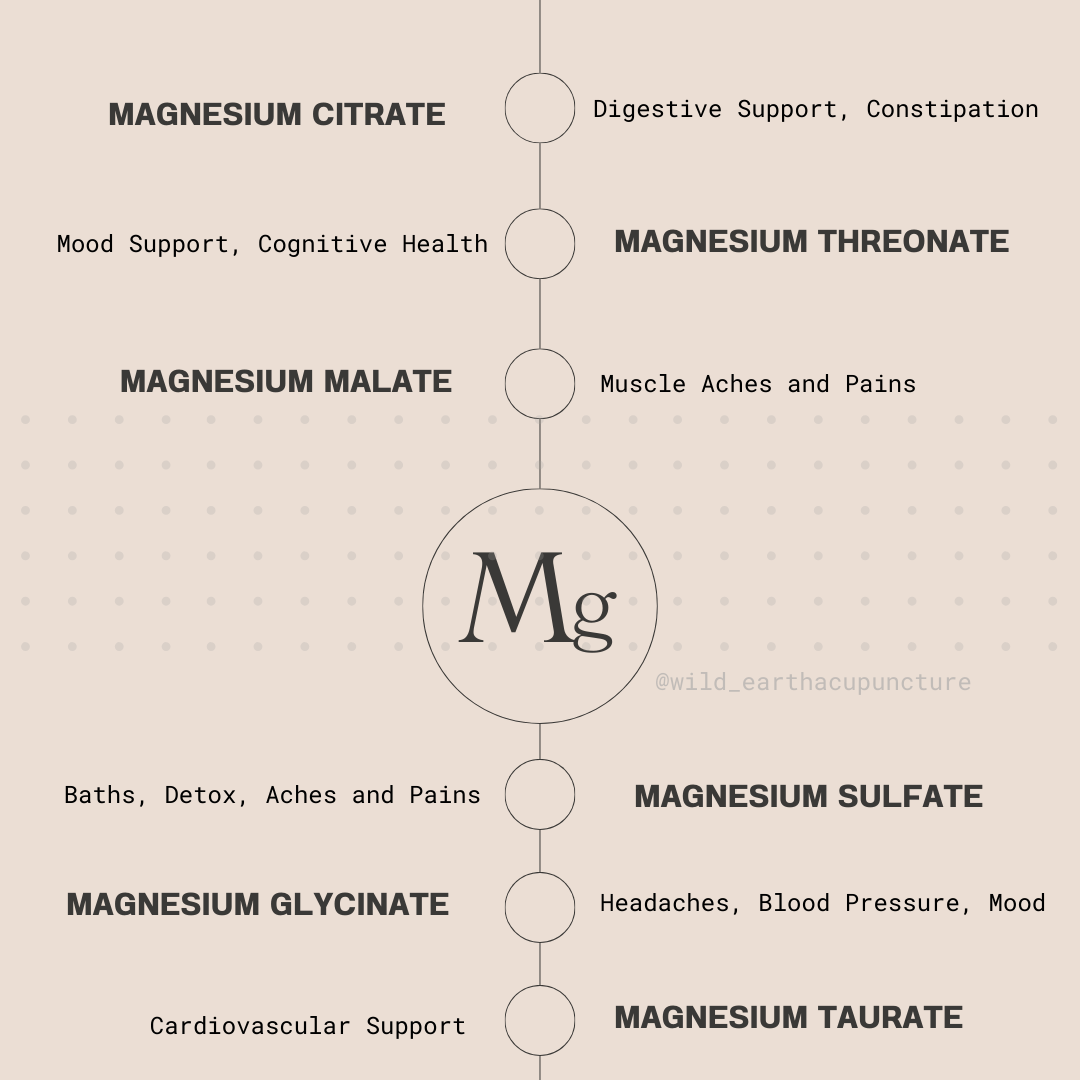
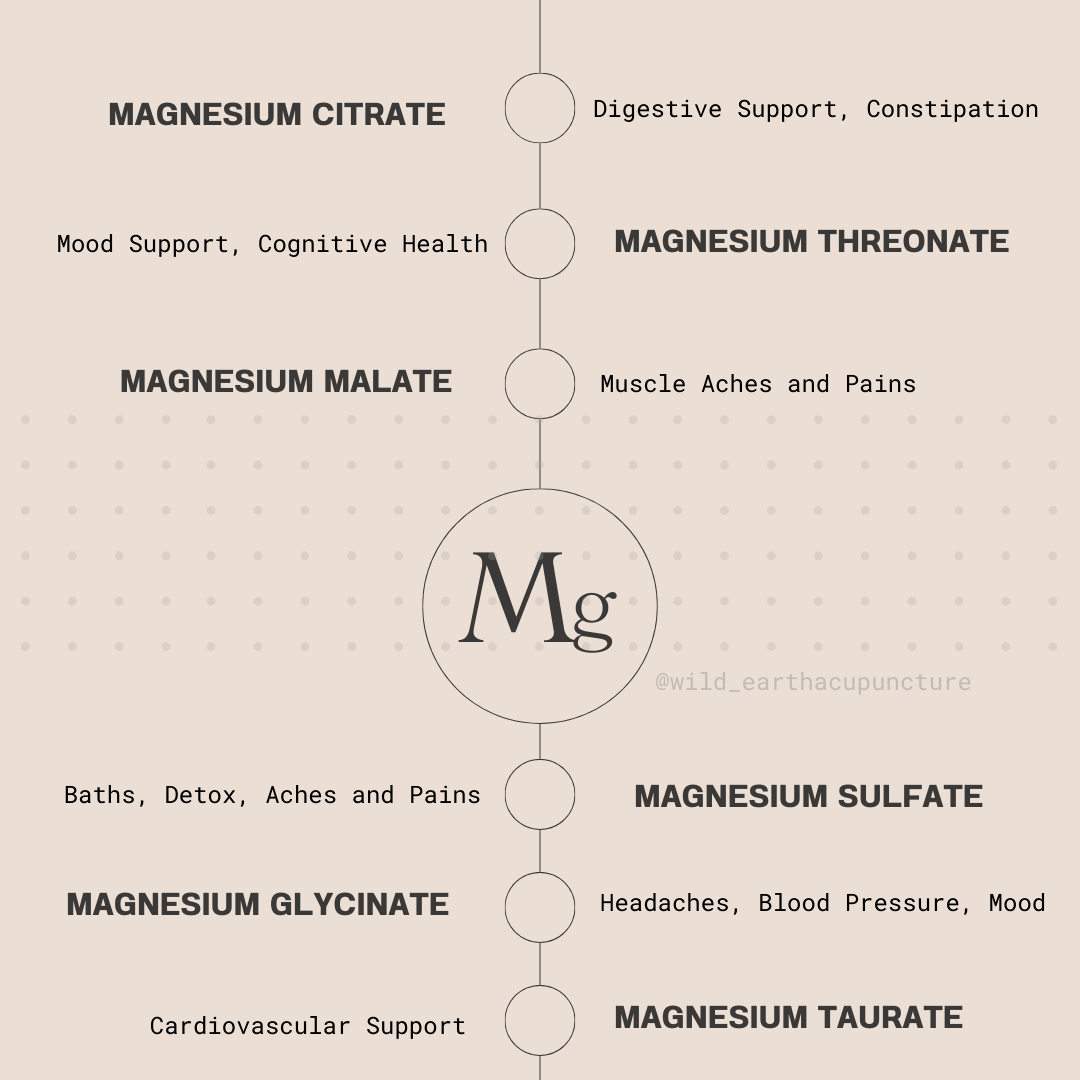
Showering can be a real struggle when you have chronic fatigue syndrome. The effort required often feels overwhelming, and sometimes the simple act of getting into the shower can trigger a whole host of symptoms. This can be directly related to issues with thyroid function and diet, including the impact of goitrogens. Understanding the impact of a thyroid disease goitrogens diet can be really helpful in managing these symptoms and finding ways to make showering more manageable.
Ultimately, it’s all about finding strategies that help you feel better and not worsen your fatigue.
- Adjustable showerheads and handheld shower nozzles: These tools allow for targeted water application, minimizing the need for extensive body movement. A person can easily adjust the angle and pressure to focus water on specific areas, reducing the overall physical effort required for showering.
- Shower benches or chairs: These provide a stable and comfortable seating position during showering, reducing the strain on the body and joints. This allows for extended periods of time in the shower without the need for constant movement or exertion.
- Grab bars and support rails: Installing grab bars or support rails in the shower area can significantly enhance stability and safety, preventing falls and injuries. This is crucial for individuals who experience balance issues or reduced strength due to CFS.
Bathroom Modifications
Modifying the bathroom environment can significantly improve the accessibility and comfort of showering for individuals with CFS. Simple changes can make a world of difference.
- Lowering the showerhead: Adjusting the height of the showerhead to a more comfortable position can reduce the need for stretching and bending, minimizing exertion.
- Installing a walk-in shower: This eliminates the need to step over thresholds, which can be a major source of pain and fatigue. A walk-in shower offers a seamless and more accessible showering experience.
- Creating a wider shower space: Increasing the width of the shower stall allows for easier maneuvering and positioning, minimizing the need for awkward movements and strain on the body.
Strategies for Managing Fatigue and Pain
Managing fatigue and pain during the showering process is crucial for a positive experience. Implementing these strategies can significantly improve the showering experience.
- Scheduling: Scheduling shower time around periods of higher energy levels can help maximize comfort and minimize exertion.
- Taking shorter showers: Breaking down the showering process into shorter, more manageable sessions can reduce the overall physical and mental demand.
- Utilizing pain relief medications or techniques: Employing pain relief strategies like over-the-counter medications or relaxation techniques, like deep breathing, can help manage discomfort during the showering process.
- Taking breaks: If needed, taking breaks during the shower can allow the body to rest and recover from exertion, preventing fatigue and discomfort.
Showering Aids Table
| Aid Type | Description | Benefits | Considerations |
|---|---|---|---|
| Adjustable Showerhead | Allows for targeted water application. | Reduces strain on the body, minimizes movement. | May require some adjustment to find the optimal setting. |
| Shower Bench/Chair | Provides a stable seating position during showering. | Reduces strain on joints, allows for extended showering. | May require space in the shower area. |
| Grab Bars/Support Rails | Enhance stability and safety. | Reduces risk of falls, improves confidence. | Installation may be required. |
Environmental Considerations
Navigating daily life with chronic fatigue syndrome (CFS) often requires significant adaptations. The bathroom, a space frequently associated with self-care, can present unique challenges. Understanding and modifying the environment to promote comfort and safety is crucial for managing symptoms and maintaining independence. This section will explore how to create a supportive and accessible bathroom environment, particularly focusing on temperature, water pressure, lighting, and design.The bathroom should be viewed as a space that enhances well-being, not a source of stress.
Careful consideration of environmental factors can make a profound difference in the ease and comfort of daily routines, especially for those with CFS. The goal is to minimize exertion and maximize comfort, ensuring the bathroom becomes a refuge rather than a hurdle.
Supportive and Accessible Bathroom Environment
Creating an accessible bathroom is about reducing physical and mental strain. This involves removing barriers to movement, ensuring clear pathways, and utilizing assistive devices if necessary. Grab bars, non-slip flooring, and wider doorways are examples of features that enhance safety and reduce the risk of falls. The design should also prioritize ease of access to all essential items, including toiletries and towels, minimizing unnecessary movements.
Temperature Control and Water Pressure
Temperature and water pressure play a significant role in the showering experience. Extremes in either can exacerbate fatigue and discomfort. A moderate water temperature, adjustable to individual preferences, is essential. A gradual temperature change can also be important. Similarly, manageable water pressure prevents overwhelming sensations.
Adjusting water pressure to a comfortable level avoids unnecessary strain.
Lighting and Sound
Lighting and sound in the bathroom can significantly impact mood and energy levels. Bright, natural light is ideal, but supplementary lighting options should be readily available. Soft, ambient lighting can create a calming atmosphere. Sound levels should be considered. Quiet or soothing sounds can promote relaxation.
Conversely, excessive noise can be overwhelming. Consider the use of sound-dampening materials or white noise machines to minimize disruptions.
Showering can be a real struggle with chronic fatigue syndrome. The effort required can often exacerbate symptoms, making it a chore. Luckily, my recent visit to the dermatologist for my atopic dermatitis your visit atopic dermatitis helped me discover some great tips for managing the discomfort and keeping my skin healthy. These tips are now helping me manage the difficulties I experience showering with chronic fatigue syndrome.
Bathroom Design Options
Various bathroom designs cater to different needs and preferences. Walk-in showers, with their easy access and reduced physical demands, can be highly beneficial for individuals with CFS. Roll-in showers provide an even greater level of accessibility for those with mobility challenges. Consider incorporating features like adjustable showerheads and handheld sprays for greater control over water pressure and temperature.
Comparison of Bathroom Design Features
| Feature | Description | Impact on Showering Experience for People with CFS | Cost Considerations |
|---|---|---|---|
| Walk-in Shower | A shower with wider doorways and a low threshold, making entry and exit easier. | Reduces physical exertion and improves safety. | Moderate to high, depending on the complexity of the design. |
| Roll-in Shower | A shower designed with a flat, smooth entry for easier access using a wheelchair. | Provides maximum accessibility for individuals with significant mobility limitations. | High, due to specialized features and construction. |
| Adjustable Showerhead | A showerhead that allows for adjustments in height, angle, and water pressure. | Provides personalized control over the shower experience, reducing strain. | Moderate, depending on the specific features. |
| Handheld Spray | A separate spray nozzle for washing specific body parts. | Allows for targeted cleaning and reduced exertion. | Moderate. |
| Non-slip Flooring | Flooring that prevents slips and falls. | Improves safety and reduces risk of injury. | Moderate. |
Hygiene and Safety

Maintaining proper hygiene is crucial for overall well-being, but for individuals living with chronic fatigue syndrome (CFS), it can present unique challenges. Finding safe and effective ways to manage personal care, especially showering, is essential to preserving both physical and emotional comfort. This section will explore the importance of hygiene practices tailored for CFS, address potential safety concerns, and offer practical strategies for a safe and comfortable showering experience.Proper hygiene practices are not just about cleanliness; they play a vital role in preventing infections and maintaining a sense of well-being.
For those with CFS, the potential for fatigue exacerbation and pain from typical hygiene routines necessitates careful consideration and adaptation. This is especially true for showering, a potentially strenuous activity for someone with CFS.
Importance of Proper Hygiene Practices
Maintaining hygiene is vital for individuals with CFS. Regular personal care routines help prevent skin infections, promote a sense of normalcy, and contribute to overall comfort and self-esteem. Compromised immune systems and increased fatigue levels make individuals with CFS more susceptible to infections, so proper hygiene practices are even more important in this population. However, it’s essential to recognize the limits of energy and physical capacity, and adapt routines accordingly.
Potential Safety Concerns During Showering
Showering can be a challenging activity for those with CFS. Potential safety concerns include the risk of falls due to dizziness or weakness, muscle strain from exertion, and injuries related to hot water or slippery surfaces. The exertion involved in showering can trigger or exacerbate fatigue, potentially leading to accidents. Careful planning and adaptation are key to minimizing these risks.
Strategies for Safe and Comfortable Showering
Implementing safe showering strategies involves minimizing exertion and maximizing comfort. A gradual approach to showering is recommended, starting with short, less-intense sessions. Adjusting water temperature to a comfortable level, avoiding extremes, is essential to prevent discomfort or shock. Using supportive surfaces like non-slip mats or grab bars can greatly enhance safety during the showering process. Consider pre-shower planning, setting out all necessary items beforehand, to avoid unnecessary movements and exertion.
Alternative Hygiene Methods
While showering is a common practice, alternative hygiene methods can be used in place of or alongside showering, offering a more manageable approach for those with CFS. These methods can be used for various body parts and include:
- Wiping: Using a damp cloth or sponge for quick cleaning of specific areas can be an effective and less strenuous alternative to full showering.
- Spot Cleaning: Concentrating on areas needing attention, such as hands and face, can be a more manageable approach than a full-body wash.
- Sponge Baths: Using a sponge and gentle water pressure can provide a sufficient level of cleanliness without the exertion of a full shower.
- Sitz Baths: A sitz bath is a shallow basin of warm water used for cleaning the perineal area. It can be a gentler and more comfortable alternative to showering for this specific region.
Hygiene Tips and Safety Measures for Showering with CFS
Implementing strategies for safe and effective hygiene practices is crucial for individuals with CFS. A tailored approach that considers individual limitations and needs is paramount.
| Tip | Description | Importance | Implementation |
|---|---|---|---|
| Gradual Approach | Start with short, less-intense sessions and gradually increase duration as tolerated. | Prevents fatigue exacerbation and potential injuries. | Begin with 5-10 minutes, increasing by 2-5 minutes per session as tolerance improves. |
| Comfortable Temperature | Adjust water temperature to a comfortable level, avoiding extremes. | Prevents discomfort and shock. | Use a thermometer or a test with your hand to check the water temperature. |
| Non-Slip Surfaces | Use non-slip mats or grab bars to enhance safety and prevent falls. | Reduces risk of slips and falls. | Place mats in the shower area and use grab bars for support. |
| Pre-Planning | Set out all necessary items beforehand to avoid unnecessary movements and exertion. | Reduces fatigue and potential injuries during showering. | Gather all items like soap, washcloths, and towels before entering the shower. |
| Rest Periods | Take breaks between showering sessions if necessary. | Allows for rest and recovery, preventing further fatigue exacerbation. | Plan for short breaks between different tasks or parts of the showering process. |
Long-Term Management and Support: Problems Showering Chronic Fatigue Syndrome

Navigating chronic fatigue syndrome (CFS) can be a lifelong journey, and showering, though seemingly simple, can become a significant challenge. Long-term management involves understanding the ebb and flow of your energy levels, adapting your routines, and seeking the right support systems. This requires a proactive approach, emphasizing strategies that allow for consistency and prevent frustration.Effective long-term management of showering difficulties necessitates a multi-faceted approach that encompasses individualized plans, professional guidance, and supportive relationships.
This requires a careful balance between self-advocacy and the support of healthcare professionals, caregivers, and peers. The goal is to create a sustainable showering routine that minimizes stress and maximizes well-being.
Individualized Showering Plans
Creating a personalized showering plan is crucial for managing showering challenges effectively. This involves considering individual energy levels, pain thresholds, and personal preferences. The plan should be flexible and adaptable, allowing for adjustments as needed. It’s not about a rigid schedule, but a structured approach that accounts for the variability of CFS symptoms.
Role of Healthcare Professionals
Healthcare professionals play a vital role in long-term management. They can provide guidance on pain management techniques, assistive devices, and strategies for conserving energy. Physicians can also assess the impact of showering on overall health and recommend modifications as needed. Regular communication with healthcare providers is essential for adjusting the plan as symptoms change.
Caregiver and Support Group Involvement, Problems showering chronic fatigue syndrome
Caregivers and support groups offer crucial emotional and practical support. Caregivers can assist with tasks, such as fetching supplies or adjusting water temperature. Support groups provide a sense of community and shared understanding, offering valuable insights and encouragement. These groups offer a space to share experiences, find solutions, and receive emotional support.
Communication and Collaboration
Open communication and collaboration with healthcare providers are essential for effective long-term management. Sharing personal experiences, including showering difficulties, allows providers to tailor recommendations and treatments. Providing detailed feedback on the effectiveness of different strategies is equally important. This collaborative approach allows for a dynamic and responsive management plan.
Showering can be a real struggle with chronic fatigue syndrome. The effort required can sometimes trigger debilitating cold sweats, making the experience even more challenging. Understanding the causes and treatment of these episodes is key to managing this symptom, which can be found in resources like causes and treatment of cold sweats. Thankfully, there are strategies to help you better navigate these physical and emotional hurdles, allowing you to shower with less stress and more comfort.
Resources and Support Systems
Numerous resources and support systems are available for individuals with CFS and showering difficulties. These include:
- Support Groups: Online and in-person support groups provide a safe space to connect with others facing similar challenges. These groups can offer practical advice, emotional support, and a sense of belonging.
- Assistive Devices: Adaptive equipment, such as handheld showerheads or grab bars, can significantly ease the showering process. These tools can minimize physical strain and improve safety.
- Occupational Therapists: Occupational therapists can assess daily routines and suggest adjustments to improve efficiency and safety. They can help create customized strategies to manage showering and other daily tasks.
- Home Modifications: Adapting the bathroom environment can make showering more accessible and safe. For example, installing grab bars or a lower showerhead can reduce the physical strain of the activity.
Creating a Personalized Showering Plan
A personalized showering plan should consider individual needs and preferences. This plan should include:
- Energy Levels: The plan should be structured around available energy levels, avoiding overexertion.
- Pain Management: Strategies to minimize pain during and after showering should be included.
- Timing: The ideal time for showering should be considered, taking into account energy levels and personal preferences.
- Duration: Short, manageable showering sessions are preferable.
- Environment: The bathroom environment should be adjusted to ensure comfort and safety, such as adjusting the water temperature or ensuring proper lighting.
Visual Representation
Chronic Fatigue Syndrome (CFS) presents unique challenges, and adapting daily routines, especially personal hygiene tasks like showering, is crucial. Visualizing an accessible bathroom tailored to the needs of someone with CFS provides a tangible understanding of the practical solutions that enhance independence and dignity. This section delves into the design of such a space, assistive technologies, and the importance of emotional support in the context of showering.The design of an accessible bathroom for someone with CFS prioritizes safety, ease of movement, and minimizing exertion.
This goes beyond simply adding grab bars; it’s about creating a space where the individual can manage the task with the least amount of physical and mental effort.
Accessible Bathroom Design
This design focuses on reducing physical demands during the showering process. The bathroom layout is optimized for ease of entry and exit. A wide doorway (at least 36 inches) allows for safe and unhindered movement. The shower stall is designed with a low threshold for easy entry and exit.
- Shower Head Placement: A hand-held shower head mounted on a long hose is essential. This allows the individual to control the water’s position and intensity, reducing strain on the upper body. The height of the shower head is adjustable to suit the individual’s needs.
- Seating Options: A comfortable, supportive shower bench or chair is positioned within easy reach of the shower head and the water controls. This allows the individual to sit down during the showering process, minimizing exertion.
- Grab Bars: Multiple grab bars are strategically placed throughout the bathroom, including near the shower, toilet, and sink, for support and stability.
- Lighting: Bright, even lighting throughout the bathroom improves visibility and reduces potential falls. A motion-activated light fixture can be beneficial.
- Water Temperature Control: Easy-to-reach temperature controls are positioned within easy grasp of the shower bench or chair.
- Non-Slip Flooring: The entire bathroom floor is covered with slip-resistant flooring to prevent accidents. This is especially crucial in the shower area.
Assistive Technology in Showering
Assistive technologies play a vital role in making showering accessible and less strenuous for individuals with CFS.
- Adjustable Shower Seats: These seats provide stability and comfort while showering, reducing the need for excessive exertion. Features like adjustable heights and built-in grab bars are key considerations.
- Lever-Style Faucets: Lever faucets require less force to operate compared to traditional knobs, minimizing the physical effort required to control water flow and temperature.
- Electric/Power-Assisted Shower Chairs: These chairs offer additional support and assistance, making showering easier for those with more significant mobility limitations.
Emotional Support
The emotional toll of showering with CFS should not be underestimated. Managing the physical demands, along with the accompanying fatigue and pain, can be emotionally challenging. Open communication with caregivers, therapists, and support groups is essential.
Visualization of Showering Aids
Imagine a person seated comfortably on a supportive, adjustable shower bench. A long hose with a hand-held shower head allows them to direct the water precisely. The individual’s hands rest lightly on grab bars for added stability. The lighting is bright and even, eliminating shadows and improving visibility. The person’s face is relaxed and their posture suggests a sense of comfort and control.
Community Support Groups
Community support groups provide a valuable resource for sharing experiences and finding practical solutions. These groups offer a network of individuals who understand the unique challenges of showering with CFS. Members can share tips, strategies, and advice, fostering a sense of community and shared understanding.
Final Summary
In conclusion, navigating the challenges of showering with chronic fatigue syndrome requires a multifaceted approach. Understanding the specific impacts of CFS symptoms, implementing practical solutions, and creating a supportive environment are crucial steps. By incorporating adaptive equipment, modifying the bathroom, and prioritizing safety and hygiene, individuals with CFS can maintain their well-being and dignity. Remember, personalized plans and ongoing support from healthcare professionals and caregivers are essential for long-term management.
Ultimately, the goal is to empower individuals to maintain their daily hygiene routines with dignity and comfort.