Hand pain causes treatment and when to see a doctor is a crucial guide for understanding and addressing discomfort in your hands. This comprehensive resource delves into the various causes, from everyday overuse to underlying medical conditions, offering a clear path to diagnosis and effective treatment. We’ll explore common causes, diagnostic methods, treatment options, and when immediate medical attention is necessary.
This guide will equip you with the knowledge to better understand your hand pain and take the appropriate steps toward relief and recovery. From recognizing the symptoms of different conditions to knowing when to seek professional help, we aim to empower you with the information needed to navigate this health concern effectively.
Understanding Hand Pain
Hand pain, a common ailment, can range from a mild annoyance to a debilitating condition. It’s crucial to understand the potential causes and characteristics of hand pain to seek appropriate medical attention and implement effective self-care strategies. This knowledge empowers individuals to better manage their pain and improve their overall well-being.Understanding the anatomy of the hand and the various structures susceptible to injury is vital for recognizing the potential sources of pain.
Different types of pain, like sharp, dull, or throbbing sensations, can offer clues about the underlying cause. This comprehensive overview will delve into common hand pain conditions, highlighting the anatomy, types, causes, and associated categories.
Common Hand Pain Conditions
Various conditions can lead to hand pain. Overuse, injuries, and underlying medical issues are frequent culprits. Recognizing the specific symptoms and contributing factors can facilitate proper diagnosis and treatment.
- Arthritis: Conditions like osteoarthritis and rheumatoid arthritis can cause inflammation and pain in the joints of the hand. Symptoms often include stiffness, swelling, and tenderness, particularly in the morning or after periods of inactivity. Osteoarthritis is characterized by the breakdown of cartilage, while rheumatoid arthritis involves the immune system attacking the joint lining.
- Carpal Tunnel Syndrome: This condition arises from compression of the median nerve in the carpal tunnel, a narrow passageway in the wrist. Symptoms typically include numbness, tingling, and pain in the thumb, index, middle, and ring fingers. The pain can radiate up the forearm. Activities like prolonged typing or repetitive hand motions can exacerbate the symptoms.
- Tendinitis: Inflammation of the tendons, the fibrous tissues connecting muscles to bones, often results from overuse or repetitive movements. Symptoms include pain, tenderness, and stiffness around the affected tendon. Pain often worsens with activity and can limit range of motion. Examples include De Quervain’s tenosynovitis, affecting tendons on the thumb side of the wrist.
- Fractures: Broken bones in the hand can cause severe pain, swelling, and bruising. Direct trauma, falls, or forceful impacts can lead to fractures. Symptoms include pain that increases with movement, visible deformity, and inability to use the hand.
- Ganglion Cysts: These are fluid-filled sacs that develop near joints or tendons in the hand. Symptoms can include a soft, painless lump, and pressure or discomfort when the cyst is pressed.
Anatomy of the Hand
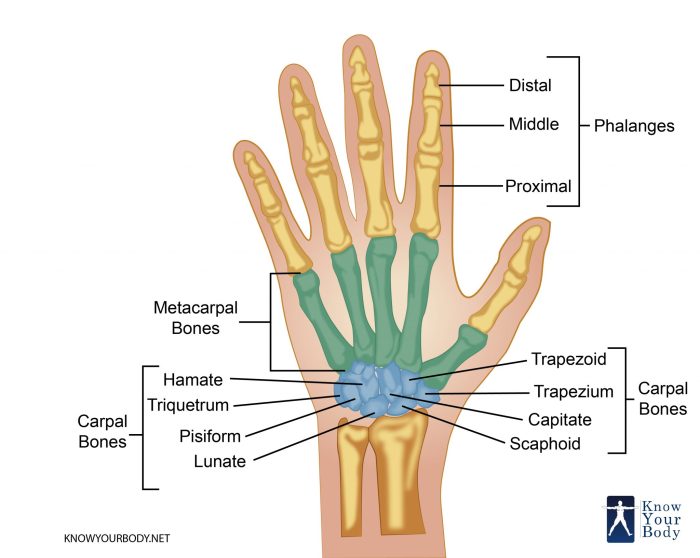
The hand is a complex structure composed of bones, joints, ligaments, tendons, and nerves. Understanding the intricate arrangement of these structures is key to comprehending the potential sources of hand pain.
- Bones: The hand comprises 27 bones, forming the framework for movement and support. These bones are connected by joints, enabling various motions. The carpal bones in the wrist, metacarpals in the palm, and phalanges in the fingers are susceptible to fractures or dislocations.
- Joints: The hand’s numerous joints allow for a wide range of motion. These joints can be affected by arthritis, resulting in pain, stiffness, and limited mobility. Examples include the metacarpophalangeal (MCP) joints and the interphalangeal (IP) joints.
- Tendons and Ligaments: Tendons connect muscles to bones, enabling movement, while ligaments connect bones to bones, providing stability. Overuse or injury can lead to tendonitis or ligament sprains, causing pain and restricting function. The flexor tendons, crucial for finger flexion, are frequently affected by overuse injuries.
- Nerves: Nerves transmit signals to and from the brain, enabling sensation and control over hand movements. Compression of these nerves, as in carpal tunnel syndrome, can lead to pain, numbness, and tingling.
Types of Hand Pain
Different types of pain can indicate various underlying causes. Understanding these characteristics can aid in proper diagnosis and treatment.
- Sharp Pain: This type of pain is often associated with acute injuries like fractures or sudden tears in tissues. It can be intense and localized.
- Dull Pain: This type of pain is often more persistent and less intense, frequently indicative of chronic conditions like arthritis or overuse injuries.
- Throbbing Pain: This pain can be intermittent and associated with inflammation, such as in cases of tendonitis or arthritis.
Common Causes of Hand Pain
Hand pain can be a debilitating issue, impacting daily activities and quality of life. Understanding the various causes behind this discomfort is crucial for effective self-management and seeking appropriate medical intervention. Different factors, such as age, lifestyle, and pre-existing conditions, play a significant role in the types of hand pain experienced.
Frequent Causes Across Demographics
Numerous factors contribute to hand pain, varying based on age and lifestyle. For instance, repetitive strain injuries are more prevalent in working-age adults involved in tasks requiring repetitive hand motions. In older adults, conditions like osteoarthritis and carpal tunnel syndrome may be more common due to the cumulative effects of years of wear and tear on joints and nerves.
Children, on the other hand, might experience hand pain due to growth spurts or sports injuries.
Symptoms of Different Hand Pain Conditions
The symptoms of hand pain can vary considerably depending on the underlying cause. A sharp, sudden pain might indicate a fracture or a tendon rupture, while a gradual, aching pain could suggest arthritis or overuse. Numbness or tingling often accompanies nerve-related issues, such as carpal tunnel syndrome. It’s essential to pay attention to the specific characteristics of the pain, such as its location, intensity, duration, and any accompanying symptoms to accurately identify the potential cause.
For example, a burning pain in the palm, radiating up the wrist, often suggests carpal tunnel syndrome.
Dealing with hand pain? Understanding the causes, treatments, and when to see a doctor is key. Sometimes, simple remedies like rest and ice can help, but if the pain persists or worsens, seeking medical attention is crucial. It’s important to remember that while some people swear by old wives’ tales like “feed a cold, starve a fever” feed a cold starve a fever , these aren’t always the best approach.
Ultimately, a proper diagnosis and treatment plan from a healthcare professional are the most effective ways to address hand pain and get back to feeling your best.
Risk Factors Associated with Hand Pain Causes
Numerous risk factors can increase the likelihood of developing hand pain. Repetitive motions at work or during hobbies are significant risk factors for repetitive strain injuries. A family history of arthritis or a history of previous hand injuries can also elevate the risk of developing certain conditions. Certain occupations, like those involving heavy lifting or manual labor, can also contribute to hand pain.
Individuals with diabetes may also experience hand pain due to nerve damage.
Specific Hand Pain Conditions
Several specific conditions can cause hand pain, each with its own characteristics. Trigger finger, a common condition, involves a tendon in the finger that gets stuck, causing a painful catching or snapping sensation. Ganglion cysts are fluid-filled sacs that can develop on the wrist or hand, typically causing swelling and mild pain. Carpal tunnel syndrome, a common condition, occurs when the median nerve in the wrist is compressed, leading to numbness, tingling, and pain in the hand and fingers.
Osteoarthritis is a degenerative joint disease that can affect the small joints in the hand, causing pain, stiffness, and limited movement. Rheumatoid arthritis is an autoimmune disease that can cause inflammation and pain in the joints throughout the body, including the hands.
Summary Table of Hand Pain Causes
| Cause | Symptoms | Risk Factors |
|---|---|---|
| Repetitive Strain Injuries | Pain, stiffness, tenderness, swelling, numbness, tingling, sometimes clicking or snapping sounds | Repetitive hand motions, improper posture, poor ergonomics, lack of rest, forceful exertion |
| Carpal Tunnel Syndrome | Numbness, tingling, and pain in the thumb, index, middle, and ring fingers, often worse at night | Repetitive hand motions, wrist strain, pregnancy, obesity, diabetes, rheumatoid arthritis |
| Trigger Finger | Catching or snapping sensation in the affected finger, stiffness, pain | Repetitive hand motions, diabetes, rheumatoid arthritis |
| Ganglion Cysts | Swelling, tenderness, sometimes pain or a feeling of fullness or pressure in the affected area | Repetitive hand motions, trauma, previous hand injuries |
| Osteoarthritis | Pain, stiffness, swelling, decreased range of motion, creaking or grating sounds in the joint | Age, genetics, obesity, previous joint injuries |
| Rheumatoid Arthritis | Inflammation, pain, stiffness, swelling in the affected joints, including the hands, fatigue, fever | Genetics, environmental factors, smoking, obesity |
Diagnosis and Evaluation
Understanding the cause of your hand pain is crucial for effective treatment. A proper diagnosis helps pinpoint the underlying issue, guiding the most appropriate course of action. This involves a thorough evaluation by a healthcare professional, combining your medical history with physical examination findings and potentially, diagnostic tests. Without a precise diagnosis, treatment might be ineffective or even harmful.A comprehensive diagnostic approach involves a multifaceted process.
It’s not just about identifying symptoms, but also understanding the context surrounding them. This includes factors like the duration, frequency, and intensity of the pain, as well as any associated symptoms like numbness, tingling, or swelling. The healthcare provider will use this information to formulate a hypothesis about the potential causes of your hand pain.
Physical Examination
A physical examination is an essential initial step in diagnosing hand pain. The doctor will carefully examine the affected area, assessing the range of motion, strength, and sensation in your hand and wrist. They will also look for any visible signs of inflammation, swelling, or deformities. This visual inspection can provide valuable clues about the possible source of your pain.
Palpation, or feeling the affected areas, will also help identify any tenderness or nodules, which can be indicative of certain conditions.
Imaging Tests
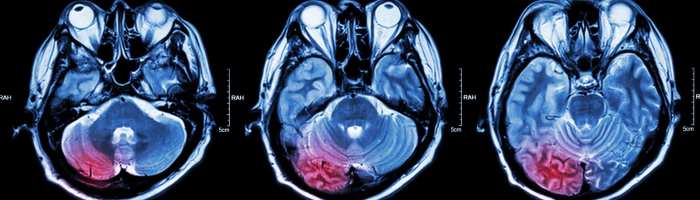
Imaging tests are often used to visualize the structures within the hand and wrist, providing crucial information for diagnosis. X-rays, for example, are excellent at revealing fractures, dislocations, or bone abnormalities. Other imaging techniques, such as MRIs (magnetic resonance imaging) or CT scans (computed tomography scans), can provide more detailed information about soft tissues, ligaments, tendons, and nerves.
MRIs are particularly helpful in identifying problems with cartilage, tendons, and ligaments. CT scans are useful in visualizing bony structures and potentially identifying foreign objects.
Diagnostic Tests Table
| Test | Purpose |
|---|---|
| X-ray | Detects fractures, dislocations, bone abnormalities, and joint space narrowing. |
| MRI | Provides detailed images of soft tissues, ligaments, tendons, nerves, and cartilage. |
| CT scan | Visualizes bony structures in detail and can identify foreign objects. |
| Blood tests | Assess for inflammation or infection; helps in ruling out conditions like rheumatoid arthritis. |
| Nerve conduction studies | Evaluate the function of nerves, identifying potential nerve entrapment or damage. |
Medical History
A thorough medical history is a critical part of the diagnostic process. The doctor will need to know about your past medical conditions, any surgeries you’ve had, medications you’re taking, and any recent injuries or traumas to your hand or wrist. For example, a history of repetitive strain injuries, like those common in certain professions, can suggest a likely cause of carpal tunnel syndrome.
Understanding your lifestyle and daily activities can also provide valuable insight into potential contributing factors.
Dealing with hand pain? Understanding the causes and treatments is key. From arthritis to repetitive strain injuries, various factors can contribute. Knowing when to seek medical attention is crucial for prompt diagnosis and effective management. While researching hand pain, it’s interesting to consider how environmental factors like humidity might influence other health concerns.
For instance, do humidifiers help with allergies? Learning more about the impact of humidity on allergies could be beneficial for overall well-being. Ultimately, if your hand pain persists or worsens, consulting a doctor is always the best course of action. do humidifiers help with allergies Remember, proper diagnosis and treatment are essential for effective relief.
Typical Doctor Questions
Doctors will ask a variety of questions during the evaluation. These questions are designed to gain a comprehensive understanding of your hand pain. Examples include: “When did the pain start?”, “What makes the pain worse or better?”, “Are there any other symptoms?”, and “Have you experienced any previous hand injuries or conditions?”. These questions help build a detailed picture of your condition and allow the doctor to narrow down the potential causes of your pain.
Treatment Options for Hand Pain
Hand pain can significantly impact daily activities, from simple tasks like gripping to more complex movements. Effective treatment hinges on accurately diagnosing the underlying cause. This section explores various treatment options, categorized for clarity, to help you understand the potential approaches for managing your hand pain.
Conservative Treatments
Conservative treatments are typically the first line of defense for hand pain. They focus on managing symptoms and promoting healing without surgery. These methods often involve lifestyle adjustments and various therapies.
Dealing with hand pain? Knowing the causes, treatments, and when to see a doctor is crucial. Sometimes, pain isn’t just in your hands, but can also stem from other areas like the big toe joint. For example, understanding the causes of pain at the big toe joint can provide clues to similar issues in your hands.
Ultimately, proper diagnosis and treatment of hand pain require a thorough evaluation, so don’t hesitate to seek professional help if the pain persists.
- Rest and Ice: Initial treatment often involves resting the affected hand and applying ice packs to reduce inflammation and pain. This is particularly important in the acute phase of injury or inflammation. Applying ice for 15-20 minutes at a time, several times a day, can significantly reduce swelling and discomfort.
- Pain Medications: Over-the-counter pain relievers like ibuprofen or naproxen can help manage mild to moderate pain. However, consult with a healthcare professional before using these medications, especially if you have underlying health conditions. Stronger pain medications may be prescribed by a doctor for more severe cases.
- Physical Therapy: Physical therapy exercises and stretches can improve hand strength, flexibility, and range of motion. A physical therapist can develop a personalized program to address the specific needs of your hand condition. This is crucial for conditions like carpal tunnel syndrome, where exercises can help alleviate symptoms.
- Splinting: Splinting can immobilize the hand, reduce stress on injured tissues, and promote healing. Splints can support joints and prevent further injury, particularly for conditions such as arthritis or fractures.
- Corticosteroid Injections: In some cases, corticosteroid injections into the affected area can help reduce inflammation and pain. These injections are often used for conditions like tendonitis or bursitis. However, they may not be suitable for everyone and may have potential side effects.
Surgical Treatments
Surgical interventions are often reserved for cases where conservative treatments are ineffective or when the underlying cause requires direct correction.
- Carpal Tunnel Release: This surgery involves cutting the transverse carpal ligament to relieve pressure on the median nerve, alleviating symptoms of carpal tunnel syndrome. Recovery time varies, but patients often experience significant improvement after surgery. The success rate of this procedure is high, often leading to a marked reduction in symptoms.
- Tendon Repair: For injuries to tendons, surgical repair may be necessary to restore proper function. This procedure involves repairing the damaged tendon, potentially using grafts to replace the damaged section. Post-operative rehabilitation is crucial for restoring full function and strength.
- Joint Replacement: In cases of severe arthritis or joint damage, joint replacement surgery can restore joint function and reduce pain. The recovery time for joint replacement surgery is longer than other procedures, but the benefits can be substantial for improved mobility and reduced pain.
Comparing Treatment Options
| Treatment Option | Effectiveness | Cost | Recovery Time | Potential Side Effects |
|---|---|---|---|---|
| Rest and Ice | Low to Moderate | Low | Variable, depends on severity | None, or minimal |
| Pain Medications | Moderate | Low | Variable | Possible stomach upset, allergic reactions |
| Physical Therapy | Moderate to High | Moderate | Variable, depends on severity and adherence | Possible muscle soreness |
| Splinting | Moderate | Low to Moderate | Variable | Possible discomfort, skin irritation |
| Corticosteroid Injections | High (short-term) | Moderate | Short | Infection, bruising, nerve damage, tendon rupture |
| Carpal Tunnel Release | High | High | Several weeks | Infection, nerve damage, swelling, pain |
| Tendon Repair | High | High | Several weeks to months | Infection, nerve damage, stiffness, pain |
| Joint Replacement | High | High | Several months | Infection, blood clots, nerve damage, pain |
When to Seek Medical Attention: Hand Pain Causes Treatment And When To See A Doctor
Hand pain, while often manageable, can sometimes signal a more serious underlying issue. Ignoring certain symptoms can lead to complications and hinder your ability to perform daily tasks. Understanding when to seek medical attention is crucial for prompt diagnosis and effective treatment.
Symptoms Warranting Immediate Medical Attention, Hand pain causes treatment and when to see a doctor
Early intervention is vital for conditions that could cause permanent damage or hinder recovery. Recognizing these symptoms is key to ensuring timely medical care.
- Severe, persistent pain that doesn’t respond to over-the-counter pain relievers.
- Swelling, redness, or warmth around the affected area that intensifies over time.
- Numbness or tingling in the hand or fingers, especially if accompanied by weakness or loss of sensation.
- Sudden, significant weakness or loss of function in the hand or fingers.
- Deformity or misalignment of the hand or fingers, like a broken bone or dislocation.
- Signs of infection, such as pus, fever, or chills.
- Pain that is accompanied by a noticeable change in skin color, such as pale, blue, or purple discoloration.
- Hand pain that is severe enough to disrupt your daily activities and limit your mobility.
- Recent injury, such as a fall or accident, that causes significant hand pain.
Situations Requiring Prompt Medical Attention
Delaying treatment for certain conditions can lead to long-term complications, impacting your overall well-being. Recognizing these situations is paramount.
- A hand injury from a workplace accident, sports activity, or any forceful trauma requiring immediate attention.
- Symptoms of a potential fracture or dislocation, such as a popping sound, inability to move the hand, or severe pain.
- Signs of a serious infection, like cellulitis, which can rapidly spread and require prompt antibiotic treatment.
- Pain associated with arthritis, particularly if it’s accompanied by swelling or stiffness, as it can accelerate the progression of the disease.
- Symptoms related to conditions like carpal tunnel syndrome, which can become more severe if not addressed promptly.
Signs of Potential Serious Medical Conditions
Certain symptoms could indicate a more serious medical condition that requires prompt medical intervention.
- Persistent hand pain that’s accompanied by fever, chills, or unexplained weight loss.
- Pain that radiates to the arm, shoulder, or neck.
- Numbness or tingling in the hand that extends beyond the fingers and into the forearm.
- Sudden onset of hand pain that’s accompanied by a change in vision or difficulty speaking.
- Persistent hand pain that worsens over time, especially if it’s associated with a recent illness or medication change.
Importance of Seeking Professional Help
Hand pain can significantly impact your daily life. Ignoring pain that interferes with essential activities can lead to further problems.
- Pain that limits your ability to perform daily tasks, such as gripping objects, writing, or working.
- Pain that disrupts sleep or other essential daily routines.
- Inability to work or participate in activities due to hand pain.
- Inability to perform tasks necessary for self-care.
Flowchart for When to Seek Medical Attention
The following flowchart provides a visual guide for determining when to seek medical attention for hand pain. It’s designed to help you make informed decisions based on the severity and nature of your symptoms.
| Step | Situation | Action |
|---|---|---|
| 1 | Mild pain, responds to over-the-counter remedies | Monitor symptoms, consider rest and ice. Contact doctor if symptoms worsen. |
| 2 | Severe, persistent pain, swelling, numbness, or infection signs | Seek immediate medical attention. |
| 3 | Recent injury, deformity, or significant loss of function | Seek immediate medical attention. |
| 4 | Symptoms of potential serious condition (fever, radiating pain, vision changes) | Seek immediate medical attention. |
Self-Care and Home Remedies
Taking care of mild hand pain at home can often be very effective. Simple steps like rest, gentle exercises, and over-the-counter medications can significantly reduce discomfort and speed up recovery. Understanding the causes of your pain and implementing appropriate self-care strategies can prevent further complications and promote overall hand health.Proper self-care is crucial for managing mild hand pain effectively.
It’s important to remember that home remedies are often suitable for short-term relief and should not replace professional medical advice. Consult a doctor if pain persists or worsens, or if you suspect an underlying medical condition.
Safe and Effective Self-Care Measures
Many mild hand pain issues can be managed effectively with self-care measures at home. These strategies, when used appropriately, can often alleviate discomfort and promote healing. The following steps are designed to provide temporary relief and should not replace professional medical advice.
- Rest: Allowing the affected hand to rest is essential for reducing inflammation and allowing tissues to heal. Avoid activities that aggravate your pain. This includes repetitive motions, heavy lifting, or any activity that puts stress on the hand.
- Ice Application: Applying ice packs to the affected area can help reduce swelling and inflammation. Wrap the ice pack in a thin towel to avoid direct skin contact and apply for 15-20 minutes at a time, several times a day.
- Compression: Using a compression bandage can help reduce swelling and support the hand. Ensure the bandage is not too tight, as this could impede blood flow.
- Elevation: Keeping the affected hand elevated above the heart can help reduce swelling. This can be done by resting the hand on pillows or cushions.
Specific Exercises and Stretches
Gentle exercises and stretches can help improve hand flexibility and strength, which can be beneficial in preventing and relieving hand pain. These exercises should be performed gently, avoiding any pain or discomfort. If pain persists or worsens, stop the exercise and consult a doctor.
- Finger Stretches: Gently bend and straighten each finger individually, then make a fist and hold for a few seconds. Repeat this 10-15 times.
- Wrist Circles: Gently rotate your wrist in both clockwise and counterclockwise directions. Repeat 10-15 times in each direction.
- Hand and Finger Flexion/Extension: Extend your fingers fully and flex them back towards your palm. Repeat 10-15 times. Extend your hand fully upwards and downwards. Repeat 10-15 times.
Importance of Proper Hand Posture and Ergonomics
Maintaining proper hand posture and using ergonomic tools can prevent hand pain and discomfort. A proper posture reduces strain on the hand, wrist, and forearm, thereby decreasing the risk of injury.
- Neutral Hand Position: Avoid holding your hand in awkward positions for extended periods. Keep your hand and wrist in a neutral position, avoiding excessive flexion or extension.
- Proper Lifting Techniques: Use your entire body to lift heavy objects, not just your hands. Avoid twisting your wrist while lifting.
- Ergonomic Tools: Use ergonomic tools, such as specialized keyboards or mouse pads, when performing repetitive tasks.
Over-the-Counter Medications
Several over-the-counter medications can help reduce inflammation and pain associated with mild hand pain. These medications are intended for temporary relief and should not be used for extended periods. Consult a doctor if pain persists or worsens.
- Nonsteroidal Anti-inflammatory Drugs (NSAIDs): NSAIDs, such as ibuprofen or naproxen, can help reduce inflammation and pain. Follow the dosage instructions carefully.
Home Remedies and Potential Benefits
The following table Artikels some home remedies and their potential benefits for managing mild hand pain. Note that these remedies are for informational purposes only and should not replace professional medical advice.
| Home Remedy | Potential Benefits |
|---|---|
| Cold Compress | Reduces inflammation and swelling. |
| Rest | Allows tissues to heal and reduces strain on the hand. |
| Gentle Exercises | Improves flexibility and strength. |
| Over-the-Counter Pain Relievers (NSAIDs) | Reduces inflammation and pain. |
Preventing Hand Pain
Hand pain, a common ailment, can significantly impact daily life. Preventive measures play a crucial role in reducing the risk of developing hand pain conditions. Proactive strategies, encompassing proper hand hygiene, mindful movement patterns, and ergonomic considerations, are essential components in safeguarding hand health. Understanding these preventive measures empowers individuals to take control of their hand well-being.
Importance of Hand Hygiene
Maintaining meticulous hand hygiene is paramount in preventing hand pain, particularly infections that can lead to inflammation and discomfort. Regular and thorough handwashing with soap and water, especially after contact with potentially contaminated surfaces, is a cornerstone of hand hygiene. This practice helps to eliminate pathogens that can trigger infections and subsequent hand pain. Alcohol-based hand sanitizers can be effective alternatives in situations where immediate access to soap and water is unavailable.
Avoiding Repetitive Movements
Repetitive movements, a common occupational hazard, can lead to cumulative trauma disorders (CTDs) and hand pain. Sustained or repeated motions strain the tendons, muscles, and nerves in the hands and wrists. Activities like typing, using a mouse, or performing assembly-line work can increase the risk of developing carpal tunnel syndrome or other CTDs. To mitigate this risk, it is crucial to incorporate short breaks into work routines to allow the hands and wrists to rest and recover.
Adjusting work posture and utilizing ergonomic tools can also help reduce the strain on the hands and wrists.
Workplace Ergonomics
Workplace ergonomics plays a critical role in preventing hand pain. Ergonomic principles focus on designing the workplace to fit the worker, not the other way around. Appropriate workstation setup, including the height of the desk, chair, and monitor, is crucial in maintaining a comfortable posture and minimizing strain on the hands and wrists. Using ergonomic tools and equipment, such as adjustable keyboards and mice, can also help reduce the risk of repetitive strain injuries.
Proper workstation design can significantly minimize the risk of developing hand pain and related conditions.
Protective Equipment
Protective equipment is essential in safeguarding the hands from potential injuries. Using gloves when handling potentially hazardous materials or performing tasks that could expose the hands to injury is paramount. Examples of such protective equipment include work gloves, safety glasses, and other protective gear. Appropriate use of protective equipment reduces the risk of cuts, abrasions, and other hand injuries, ultimately preventing hand pain.
Maintaining a Healthy Weight and Lifestyle
Maintaining a healthy weight and a balanced lifestyle can contribute to reducing the risk of hand pain. Obesity can put extra stress on the joints and tissues in the hands and wrists, increasing the risk of developing conditions like arthritis. A balanced diet, regular exercise, and adequate sleep contribute to overall well-being, which in turn can reduce the risk of hand pain.
Maintaining a healthy weight and lifestyle is crucial for preventing a range of health problems, including hand pain.
Illustrative Cases and Scenarios
Understanding hand pain requires considering the specific circumstances surrounding each individual case. Factors like the type of activity, the duration of the pain, and the presence of accompanying symptoms significantly influence diagnosis and treatment. This section presents illustrative cases to highlight the diverse range of hand pain experiences.
Acute Pain After a Fall
A 65-year-old woman, Sarah, fell while ice-skating. She experienced immediate, sharp pain in her right wrist and hand. Initial assessment revealed swelling and tenderness along the radial side of her wrist. X-rays confirmed a distal radius fracture. Treatment involved a cast and physiotherapy exercises to regain wrist and hand mobility.
Sarah’s case exemplifies the importance of prompt medical evaluation for injuries sustained during falls, especially when significant pain, swelling, and tenderness are present.
Chronic Pain Associated with Repetitive Strain
A 38-year-old graphic designer, David, experienced persistent pain in his right wrist and thumb. The pain intensified during periods of prolonged computer use, and he reported a tingling sensation in his thumb and index finger. He described a “numbness” that progressively worsened throughout the day. His case points to the potential of repetitive strain injuries, particularly in occupations demanding frequent hand movements.
Diagnosis of carpal tunnel syndrome was made. Treatment included wrist splints, ergonomic adjustments at work, and possible corticosteroid injections.
Hand Pain from a Gardening Accident
A 70-year-old retired gardener, Mr. Johnson, suffered a laceration on his left hand while trimming a hedge. The wound was deep and bled profusely. Immediate first aid included applying direct pressure to the wound. He was taken to the emergency room, where the laceration was cleaned, and sutures were placed.
Mr. Johnson’s case highlights the need for prompt medical attention for deep or bleeding hand wounds. The need for professional wound care is critical to prevent infection and ensure proper healing.
Signs of a Serious Condition: Severe and Persistent Pain
A 22-year-old student, Emily, experienced intense, throbbing pain in her left hand that progressively worsened over several days. She also noted fever and chills, along with redness and swelling around the affected area. Her symptoms raised concern about potential infection. A blood test revealed elevated inflammatory markers, suggesting a bacterial infection. Treatment involved intravenous antibiotics and close monitoring.
This case illustrates the significance of seeking immediate medical attention when hand pain is accompanied by systemic symptoms like fever, chills, or redness.
Case Study: Ulnar Nerve Entrapment
A 45-year-old carpenter, Michael, complained of numbness and tingling in his ring and little fingers. The symptoms were worse at night and aggravated by gripping tools. His symptoms were exacerbated by prolonged work. He had noticed weakness in his grip strength. A nerve conduction study confirmed ulnar nerve entrapment at the elbow.
Treatment involved a night splint, and ergonomic adjustments at work. Surgical decompression of the ulnar nerve was considered and scheduled for a later date. This case study demonstrates the importance of a comprehensive evaluation when hand pain is accompanied by specific sensory and motor deficits.
Ending Remarks

In conclusion, understanding hand pain requires a multifaceted approach. This guide has provided a comprehensive overview of causes, treatments, and when to seek medical attention. Remember that early diagnosis and appropriate treatment are crucial for managing hand pain effectively and preventing potential complications. By combining self-care strategies with professional guidance, you can significantly improve your hand health and quality of life.