Making the decision to stop dialysis is a deeply personal and often difficult choice. This guide delves into the multifaceted aspects of this decision, from understanding the factors influencing the choice to exploring practical implications and available support systems. It’s a journey through the emotional, physical, and medical realities of this critical decision.
This comprehensive guide aims to provide a supportive framework for individuals and their families navigating this complex process. It examines the decision-making process, assessing patient well-being, medical considerations, practical implications, support systems, and ethical considerations. Ultimately, the goal is to empower those facing this choice with knowledge and resources.
Understanding the Decision-Making Process: Making The Decision To Stop Dialysis
The decision to discontinue dialysis is a profoundly personal one, fraught with complex emotions and difficult choices. It’s a journey marked by introspection, careful consideration, and the need to balance the benefits and burdens of treatment. This decision isn’t made lightly, but rather after a thorough evaluation of various factors impacting quality of life. This exploration delves into the multifaceted process involved, from the initial considerations to the emotional and psychological implications.The decision to discontinue dialysis is not a simple ‘yes’ or ‘no’ choice; rather, it’s a complex evaluation of personal values, medical realities, and emotional well-being.
Individuals facing this decision need a comprehensive understanding of the factors influencing their choice, the emotional landscape, and the stages involved in the decision-making process.
Factors Influencing the Decision
Understanding the various factors influencing the decision to discontinue dialysis is crucial for navigating this complex process. These factors range from physical limitations and medical prognosis to emotional and psychological considerations.
| Category | Factor | Description | Impact |
|---|---|---|---|
| Physical | Progressive decline in health | As kidney disease progresses, symptoms and limitations may worsen, leading to a reduced quality of life. This includes increasing fatigue, pain, and difficulty performing daily tasks. | Decreased ability to endure treatment and potential for significant discomfort, impacting the decision to continue treatment. |
| Physical | Treatment side effects and burdens | Dialysis itself can be physically taxing, requiring significant time commitment and potentially leading to complications like anemia, malnutrition, or infections. | The physical burden of dialysis can outweigh the benefits, leading to the desire for an alternative. |
| Physical | Inability to maintain treatment adherence | Chronic illness and its associated complications may make it difficult to adhere to the rigorous treatment schedule required for dialysis. | Difficulty adhering to the dialysis regimen may lead to decreased treatment efficacy and potentially decreased quality of life. |
| Emotional | Depression and anxiety | The emotional toll of a chronic illness like kidney failure and the associated treatment can lead to depression and anxiety. | These emotional burdens may make the decision to discontinue dialysis more appealing, potentially as a means of coping with emotional distress. |
| Emotional | Loss of independence and autonomy | Chronic illness and treatment can significantly limit an individual’s ability to participate in activities they once enjoyed and maintain their independence. | A desire to regain control and autonomy may influence the decision to discontinue dialysis. |
| Emotional | Fear of future suffering | Patients may fear further deterioration in health and the prospect of prolonged suffering. | Fear of future suffering may motivate the decision to discontinue dialysis to prevent further deterioration in health. |
| Social | Support system | The availability and support of family, friends, and healthcare professionals can significantly influence the decision-making process. | Adequate support can provide comfort and assistance, potentially encouraging the continuation of treatment. Lack of support may contribute to the decision to discontinue dialysis. |
| Social | Financial constraints | The cost of dialysis can be substantial, and this financial burden may create significant stress. | Financial burdens may lead to the decision to discontinue dialysis, as the cost can be prohibitive. |
| Medical | Limited treatment options | In certain cases, the effectiveness of dialysis may be limited or the patient’s overall health may not be conducive to ongoing treatment. | Limited treatment options may be a significant factor in the decision to discontinue dialysis. |
| Medical | Overall prognosis | A physician’s assessment of the patient’s overall prognosis can inform the decision-making process. | An unfavorable prognosis may influence the decision to discontinue dialysis, especially if the potential benefits are deemed minimal. |
Stages of Decision-Making
The decision to discontinue dialysis is rarely instantaneous. It’s a process that often involves several stages:
- Initial Awareness and Reflection:
- Information Gathering and Evaluation:
- Emotional Processing and Acceptance:
- Decision Making and Implementation:
This initial stage involves recognizing the limitations of dialysis and considering alternative options. This phase is characterized by introspection and reflection on the individual’s values and priorities.
This stage involves researching different treatment options and understanding the potential benefits and drawbacks of each. This process often involves consulting with healthcare professionals, family members, and support groups.
This stage is crucial for acknowledging the emotional impact of the decision. It involves processing feelings of grief, loss, and uncertainty.
Making the tough decision to stop dialysis is incredibly personal, and often involves weighing many factors. While physical therapy and exploring non surgical treatments for rotator cuff tears, like those discussed in this helpful guide, non surgical treatments for rotator cuff tears , can sometimes be part of the equation, the ultimate choice rests on individual circumstances and quality of life.
Ultimately, the decision to stop dialysis is a deeply personal one, with each person’s needs and goals needing careful consideration.
This final stage involves making a conscious choice and implementing the decision. This involves communicating with healthcare providers to ensure a smooth transition.
Common Considerations, Making the decision to stop dialysis
Individuals facing this decision often grapple with various considerations:
- Quality of Life:
- Financial Burden:
- Emotional Well-being:
A critical factor is the assessment of the current quality of life and how dialysis impacts it. This involves weighing the benefits of treatment against the burdens and limitations it imposes.
The financial implications of dialysis, including the costs of treatment, medications, and potential future care, are often significant.
The emotional toll of chronic illness and treatment can significantly impact an individual’s well-being. Addressing these emotional challenges is crucial.
Assessing Patient Well-being

Deciding to discontinue dialysis is a deeply personal and complex process. It’s not simply about the medical facts, but also about the patient’s overall well-being and quality of life. Understanding the various factors that contribute to a patient’s experience is crucial for making an informed decision. This assessment involves considering the impact of dialysis itself, the patient’s physical and emotional state, and their social support network.This exploration delves into the specific indicators of decreased quality of life associated with dialysis, how declining health influences the decision-making process, the importance of patient autonomy, and different methods of measuring patient well-being.
By examining these facets, we can better grasp the multifaceted nature of this critical decision.
Deciding to stop dialysis is a monumental choice, filled with complex emotions. It’s a deeply personal decision, weighing the pros and cons, and understanding the potential impact on quality of life. Sometimes, skin reactions from the dialysis treatments themselves can be a significant factor, like contact dermatitis. If you’re experiencing skin issues, understanding the process of patch testing for contact dermatitis can help determine if the reactions are related to specific materials in the dialysis equipment or products used.
Ultimately, the decision to stop dialysis remains a personal one, with ongoing support from healthcare professionals crucial throughout the process.
Potential Indicators of Decreased Quality of Life
The burden of dialysis can manifest in various ways, impacting a patient’s quality of life. These indicators include: physical discomfort from treatment procedures, fatigue and energy depletion, decreased mobility and independence, and cognitive impairment. Social isolation can also arise due to the time commitment and logistical demands of dialysis. These factors significantly influence the patient’s ability to participate in activities they once enjoyed and maintain fulfilling relationships.
Impact of Declining Health on the Decision-Making Process
Declining health, regardless of the specific cause, inevitably affects the decision-making process. Physical limitations, cognitive changes, and emotional distress can all hinder a patient’s ability to process information and weigh options. This necessitates a careful and sensitive approach to ensure the patient’s voice and preferences are heard, even as their capacity to articulate them may diminish. Understanding the patient’s evolving health status is crucial for tailoring the support and guidance provided.
Importance of Patient Autonomy
Patient autonomy is paramount in this decision. The choice to discontinue dialysis must ultimately be the patient’s, based on their values, preferences, and current situation. Providers must respect the patient’s right to self-determination, even if the choice is not aligned with their own expectations or recommendations. This means fostering open communication, providing comprehensive information, and empowering the patient to make a decision that aligns with their personal goals and priorities.
Comparison of Well-being Measures
Various tools and methods exist to assess patient well-being. Each method has its strengths and weaknesses, and the most appropriate measure depends on the specific context and the information sought. Understanding the nuances of each measure is critical for a comprehensive evaluation.
| Measure | Description | Pros | Cons |
|---|---|---|---|
| Short Form Health Survey (SF-36) | A widely used questionnaire assessing physical and mental health. | Relatively easy to administer, well-validated, and standardized. Provides a comprehensive overview of well-being. | May not capture the specific issues relevant to dialysis patients. Can be time-consuming for patients with cognitive impairments. |
| Dialysis Patient Quality of Life Index (DPQLI) | Specific to dialysis patients, evaluating various aspects of their lives affected by treatment. | Directly addresses the concerns of dialysis patients, offering a personalized view. | May not be as broadly applicable to other patient populations. May not be readily available in all settings. |
| Glasgow Coma Scale | A neurological scale assessing consciousness in patients. | Provides a quantifiable measure of consciousness. Essential in acute care situations. | Does not capture the broader dimensions of quality of life. Not relevant for assessing well-being in chronic conditions. |
| Patient Reported Outcomes (PROs) | Measures of health status reported directly by the patient. | Provides a direct and patient-centric view of their experiences. Can be customized to address specific concerns. | Can be influenced by factors such as literacy, cognitive ability, or emotional state. May not be reliable in all circumstances. |
Medical Considerations
Deciding to discontinue dialysis is a deeply personal choice, and understanding the medical realities is crucial for informed decision-making. This section explores the potential medical complications, the expected course of events, and the possible outcomes of this significant step. It is essential to approach this information with a realistic understanding of the complexities involved and to discuss these details thoroughly with your healthcare team.
Medical Realities of Dialysis Discontinuation
Dialysis is a life-sustaining treatment for individuals with kidney failure. Stopping dialysis means the body will no longer receive the support it needs to eliminate waste products and regulate essential fluids and electrolytes. This can lead to a rapid accumulation of toxins and imbalances, impacting various organ systems. The specific medical realities will vary depending on individual health conditions and the duration of dialysis treatment.
Potential Medical Complications
Several potential complications can arise after discontinuing dialysis. These include, but are not limited to, fluid overload, electrolyte imbalances (such as potassium or sodium), metabolic acidosis, uremia (a buildup of waste products in the blood), and central nervous system complications like seizures or altered mental status. The severity of these complications can range from mild discomfort to life-threatening conditions.
Expected Course of Events Following the Decision
The course of events following dialysis discontinuation is influenced by individual factors such as the duration of dialysis treatment, overall health status, and the presence of other underlying medical conditions. Symptoms may begin to manifest relatively quickly after discontinuation. A period of close monitoring and supportive care is crucial to manage any developing complications. This often involves frequent blood tests and close observation by healthcare professionals.
Potential Side Effects and Complications
Understanding potential side effects and complications is essential for preparing for the transition. A comprehensive list, while not exhaustive, includes:
- Rapid increase in blood urea nitrogen (BUN) and creatinine levels
- Fluid retention and swelling (edema)
- Electrolyte disturbances, such as hyperkalemia
- Metabolic acidosis
- Nausea, vomiting, and anorexia
- Neurological changes, such as confusion, disorientation, and seizures
- Decreased blood pressure
- Respiratory distress
- Heart failure
Possible Outcomes of Stopping Dialysis
The table below Artikels possible outcomes of discontinuing dialysis, highlighting their descriptions, probability, and impact. It is important to note that these are not absolute predictions and individual outcomes may vary.
| Outcome | Description | Probability | Impact |
|---|---|---|---|
| Rapid deterioration and death | A swift decline in health leading to death within days or weeks. | Low to Moderate | High |
| Gradual decline and death | A more prolonged decline in health, often spanning weeks or months, culminating in death. | Moderate | High |
| Stabilization with supportive care | A period of relative stability and manageable symptoms with medical interventions. | Low to Moderate | Moderate |
| Significant symptom relief | Noticeable reduction in symptoms, allowing for a more comfortable period of life. | Low to Moderate | Low to Moderate |
| Unpredictable course | An outcome that cannot be accurately estimated due to the complexity of individual factors. | Moderate | High |
Practical Implications
Choosing to discontinue dialysis is a deeply personal decision, requiring careful consideration of the practical aspects beyond the medical considerations. This involves navigating financial implications, arranging support systems, and planning for end-of-life care. Understanding these practical implications is crucial for making an informed choice and ensuring a peaceful transition.This section details the practical arrangements needed for discontinuation, the financial implications, the role of support systems, and key end-of-life care considerations.
It provides a structured approach to this challenging process, offering a framework for individuals and their families.
Practical Arrangements for Discontinuation
The discontinuation process necessitates careful planning to ensure a smooth and dignified transition. This involves coordinating with healthcare providers, arranging for necessary medications, and making provisions for comfort and well-being in the final stages. Specific arrangements may include: setting up a schedule for decreasing dialysis sessions, ensuring adequate pain management, and coordinating transportation if needed.
Financial Implications
Financial considerations are often a significant factor in such decisions. The cost of dialysis is substantial, and discontinuation may present unforeseen financial burdens or opportunities. This involves assessing the remaining financial resources, evaluating potential support from insurance or government programs, and exploring options for long-term care, if applicable. Examples include Medicaid, Medicare, or private insurance policies, which may offer benefits for end-of-life care.
Role of Support Systems and Resources
A robust support system is vital during this time. This includes family, friends, support groups, and healthcare professionals. The availability of hospice care, palliative care, or counseling services can significantly impact the quality of life for the patient and their loved ones. Support groups offer a valuable forum for sharing experiences and receiving emotional support from others facing similar situations.
Making the tough decision to stop dialysis is incredibly personal, often fraught with complex emotions. A crucial part of this process involves understanding pain management options, like adjuvant analgesics, which can enhance the effectiveness of other pain medications. What are adjuvant analgesics are frequently used in end-of-life care to improve comfort and quality of life during this challenging time.
Ultimately, choosing to discontinue dialysis is a deeply personal choice, weighed against the potential benefits and burdens of continued treatment.
These resources are instrumental in providing practical assistance, emotional comfort, and guidance throughout the process.
Key Considerations for End-of-Life Care Planning
End-of-life care planning is essential for ensuring that the patient’s wishes are respected and that their final days are as comfortable and peaceful as possible. This involves documenting preferences for pain management, communication, and the overall approach to care. Advance directives, such as living wills and durable power of attorney for healthcare, provide legal frameworks for carrying out these wishes.
They can offer clarity and comfort for all involved.
Steps in the Discontinuation Process
| Step | Description | Responsibility | Timeline |
|---|---|---|---|
| 1 | Assessment of patient’s physical and mental state, and discussion with healthcare team | Patient, Healthcare Team | Ongoing, leading up to decision |
| 2 | Development of a care plan outlining the discontinuation schedule | Healthcare Team | Within 1-2 weeks of decision |
| 3 | Coordination with hospice or palliative care team (if applicable) | Patient, Healthcare Team | Within 1-4 weeks of decision |
| 4 | Review and update of advance directives (if necessary) | Patient, Legal Counsel (if needed) | Ongoing, preferably before decision |
| 5 | Arranging for necessary medications and supplies | Patient, Family, Pharmacy | Immediately following decision |
| 6 | Discussions with family and close contacts about the plan | Patient, Family | Ongoing, throughout the process |
| 7 | Implementation of the care plan and monitoring of the patient’s well-being | Healthcare Team, Family | Ongoing, until end-of-life |
Support and Resources
Navigating the decision to stop dialysis is a deeply personal journey, often laden with emotional and practical challenges. Finding the right support system is crucial during this time. Understanding the available resources and support networks can ease the burden and empower both the patient and their loved ones.This section will delve into the vital role of support groups and counseling, highlighting the resources available for patients and families facing this difficult decision.
It will also detail the support systems in place for patients and provide concrete examples of such support networks.
Support Groups and Counseling
Support groups offer a safe and confidential space for patients to share their experiences, anxieties, and feelings with others who understand. These groups provide a sense of community and validation, helping patients feel less isolated and more empowered. Similarly, counseling can provide individual support, helping patients process emotions, address anxieties, and develop coping strategies. Both support groups and counseling can offer a safe space to explore options and make informed decisions.
Resources for Patients and Families
A plethora of resources are available to aid patients and families during this challenging time. These resources may include information on palliative care, hospice services, advanced directives, and end-of-life planning. Understanding these options can help navigate the practical aspects of the decision. This is also a time for families to seek advice from medical professionals and therapists who can provide support and guidance.
Support Systems for Patients
Dedicated support systems are in place to assist patients and families throughout this process. These systems often involve a multidisciplinary team including physicians, nurses, social workers, and counselors. They can provide comprehensive support encompassing emotional, medical, and practical needs. This multidisciplinary approach ensures a holistic support system tailored to individual needs.
Examples of Support Networks
Support networks for patients considering stopping dialysis often include hospitals, clinics, and community organizations. Examples include palliative care teams, hospice agencies, and support groups specifically dedicated to kidney disease. These networks can provide practical assistance with things like transportation, financial aid, and emotional support.
Available Support Resources
| Resource | Description | Contact Info | Availability |
|---|---|---|---|
| Hospice Agencies | Provide end-of-life care, including pain management, emotional support, and practical assistance. | Local listings, online search | Usually available in most regions |
| Palliative Care Teams | Manage symptoms and improve quality of life for patients with serious illnesses. | Hospitals, clinics | Often integrated into hospital systems |
| Support Groups (Kidney Disease) | Offer a peer support network for patients and families. | Local community centers, online forums | Vary by location, often free or low-cost |
| Social Workers | Provide counseling, emotional support, and connect patients with resources. | Hospitals, clinics, community agencies | Available through healthcare systems |
| Financial Assistance Programs | Offer financial support for medical expenses and other needs. | Government agencies, non-profits | Vary by region, eligibility criteria apply |
Ethical Considerations
Choosing to discontinue dialysis involves complex ethical considerations that extend beyond the medical aspects of the decision. It necessitates careful navigation of patient autonomy, healthcare professional responsibilities, and the principles of informed consent. This process requires sensitivity and a commitment to upholding the patient’s dignity and well-being throughout the decision-making process.The decision to stop dialysis often triggers a multitude of ethical dilemmas.
The patient’s right to self-determination must be balanced against the potential for irreversible harm. The potential for emotional distress for both the patient and family members is significant. This necessitates a careful, compassionate approach from healthcare professionals to ensure that the patient’s wishes are respected while maintaining their safety and well-being.
Patient Rights and Autonomy
Patients have a fundamental right to autonomy in healthcare decisions, including the right to refuse medical treatment, even if that treatment is life-sustaining. This principle underscores the importance of respecting the patient’s values, beliefs, and preferences. The patient’s right to self-determination extends to the decision to discontinue dialysis, providing they are fully informed and competent to make the choice.
Capacity for decision-making is evaluated considering factors like cognitive function and understanding of the implications of the decision.
Role of Healthcare Professionals
Healthcare professionals play a crucial role in supporting the patient through this process. Their responsibility extends beyond the technical aspects of dialysis to include empathetic communication and support. They must facilitate open and honest discussions about the patient’s options, potential outcomes, and the decision-making process. Furthermore, healthcare professionals should act as advocates for the patient, ensuring their needs and wishes are respected.
This includes ensuring access to necessary resources and support systems.
Informed Consent
Informed consent is paramount in any medical decision, especially one as significant as discontinuing dialysis. This involves ensuring the patient fully understands the implications of the decision, including potential benefits, risks, and alternatives. The patient must be provided with clear and comprehensive information, using language they can understand. Furthermore, the process should allow ample time for questions and discussion to ensure the patient’s understanding and agreement.
This process is not a one-time event; ongoing communication and reassessment of the patient’s understanding are essential.
Ethical Considerations Table
| Ethical Principle | Description | Potential Conflict | Resolution |
|---|---|---|---|
| Autonomy | Respecting the patient’s right to self-determination | Patient’s decision may conflict with healthcare professional’s perception of best interest. | Facilitating open communication and ensuring the patient’s capacity to make informed decisions. |
| Beneficence | Acting in the patient’s best interest | Discontinuing dialysis may seem detrimental to the patient’s physical well-being. | Thorough discussion of all potential outcomes, including the benefits and risks of continuing dialysis. |
| Non-maleficence | Avoiding harm to the patient | Discontinuing dialysis could lead to physical harm. | Carefully considering the patient’s overall quality of life and ensuring appropriate palliative care. |
| Justice | Fair and equitable treatment for all patients | Disparity in access to resources for dialysis discontinuation. | Ensuring equitable access to information and support for all patients considering this decision. |
Closing Notes

Choosing to discontinue dialysis is a profoundly personal journey. This guide has explored the various facets of this decision, emphasizing the importance of understanding the factors influencing the choice, assessing well-being, and considering medical and practical implications. Crucially, it highlights the support available to patients and families throughout this process, ultimately aiming to empower those facing this difficult decision.


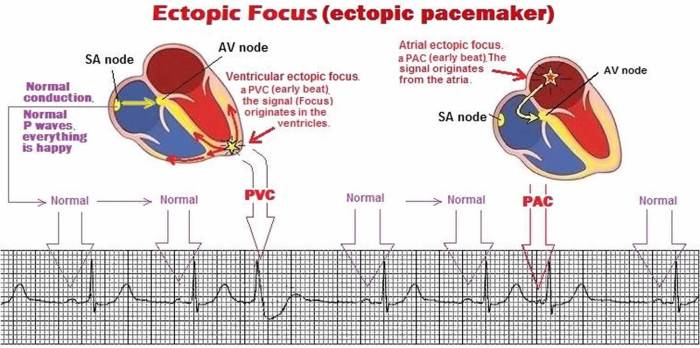
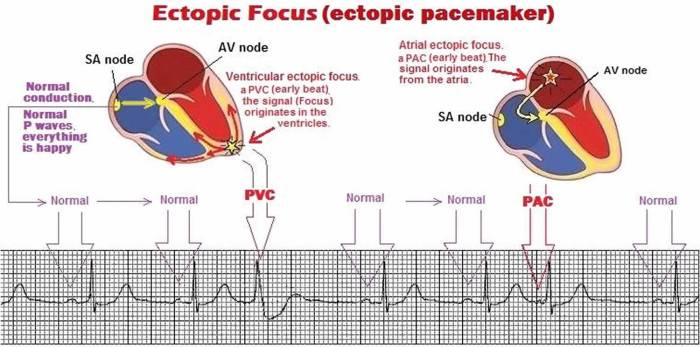
 (Diagram placeholder. A permanent pacemaker is typically implanted under the skin near the collarbone, with thin wires (leads) extending to the heart chambers. The pulse generator is housed within the implanted casing.)
(Diagram placeholder. A permanent pacemaker is typically implanted under the skin near the collarbone, with thin wires (leads) extending to the heart chambers. The pulse generator is housed within the implanted casing.)