Allergy treatments for kids are crucial for ensuring healthy development and well-being. This guide explores the complexities of childhood allergies, from common triggers and reactions to effective treatment options and proactive management strategies. We’ll delve into diagnostic methods, treatment approaches, and the importance of early intervention and education.
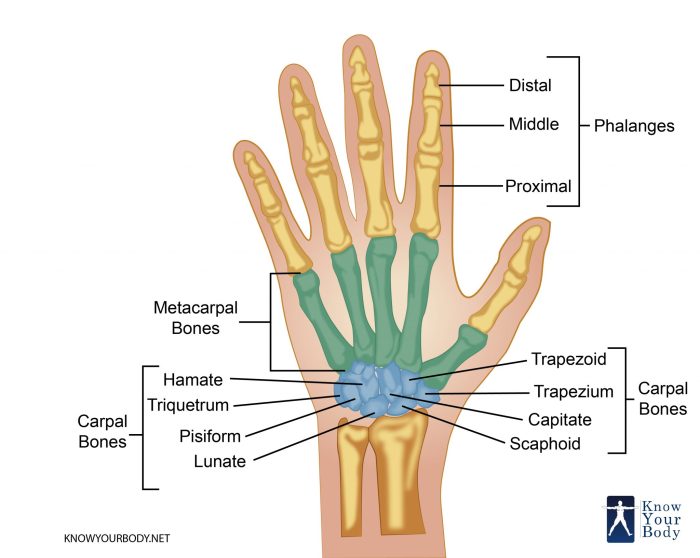
Understanding the diverse range of allergic reactions in children is vital. From skin rashes and hives to respiratory issues and gastrointestinal distress, allergies manifest in various ways. This comprehensive resource provides a detailed overview of common allergens like peanuts and dairy, highlighting their associated symptoms. The included tables offer a quick reference for comparing symptoms across different types of allergies.
Introduction to Pediatric Allergies
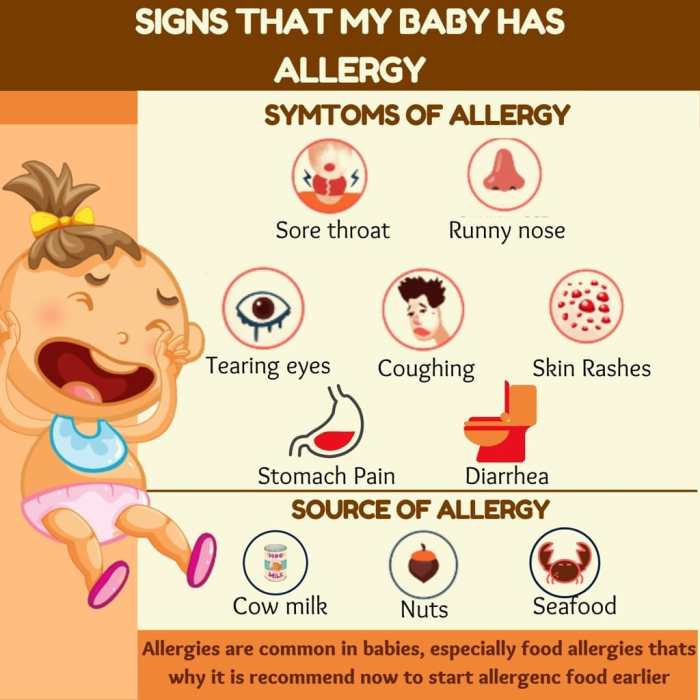
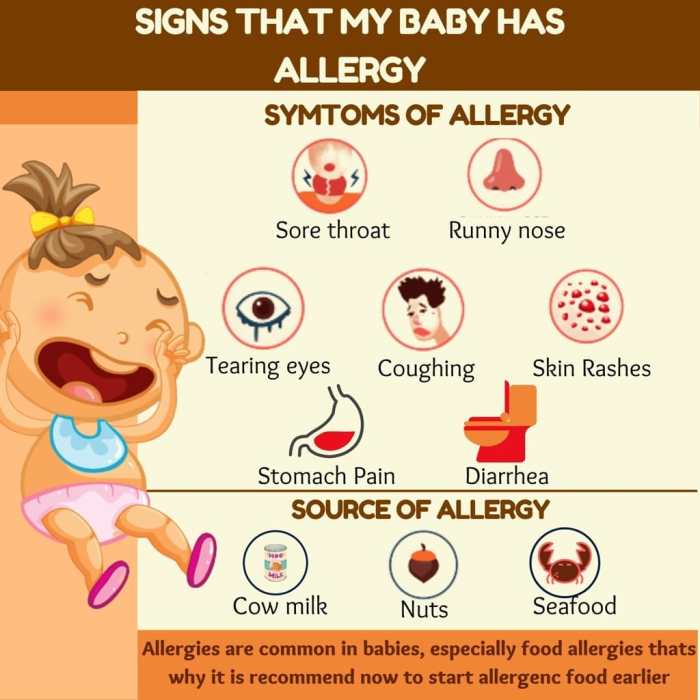
Childhood allergies are a significant health concern affecting a growing number of children worldwide. These conditions, characterized by an overreaction of the immune system to harmless substances, can manifest in various ways and impact a child’s quality of life. Understanding the types, prevalence, and symptoms of pediatric allergies is crucial for early detection and effective management.Pediatric allergies, while often mild, can sometimes lead to severe, life-threatening reactions.
Prompt diagnosis and appropriate treatment are essential to minimize the impact of these conditions on a child’s development and well-being. Early intervention can also help prevent the development of more severe allergies or complications later in life.
Common Childhood Allergies
A variety of substances can trigger allergic reactions in children. These allergens range from common foods to environmental factors. Identifying the specific triggers is vital for effective allergy management.
Types of Allergic Reactions in Children
Allergic reactions in children can vary in severity, from mild discomfort to potentially life-threatening anaphylaxis. Understanding these differences is critical for recognizing the need for immediate medical attention. Common types of allergic reactions include skin reactions, respiratory problems, and gastrointestinal issues.
Prevalence of Allergies in Children
The prevalence of childhood allergies is on the rise globally. Several factors contribute to this increase, including environmental changes, lifestyle modifications, and potentially increased exposure to allergens in early childhood. While exact figures vary by region and specific allergen, data consistently shows a substantial portion of children experience some form of allergic reaction.
Symptoms of Common Childhood Allergies
Recognizing the symptoms associated with various allergens is key to early intervention. This allows for timely medical attention and appropriate treatment. The table below provides a concise overview of common symptoms, categorized by allergen and affected system.
| Allergen | Symptoms (Skin) | Symptoms (Respiratory) | Symptoms (Gastrointestinal) |
|---|---|---|---|
| Peanuts | Rash, hives, itching, swelling | Wheezing, coughing, shortness of breath, throat tightness | Vomiting, diarrhea, abdominal cramps, nausea |
| Dairy | Skin rash, eczema, hives, itching | Runny nose, congestion, sneezing, coughing | Stomach ache, bloating, gas, diarrhea |
| Eggs | Hives, itching, swelling | Coughing, wheezing, shortness of breath, runny nose | Vomiting, diarrhea, abdominal pain |
| Tree Nuts | Rash, hives, itching, swelling | Wheezing, coughing, shortness of breath, throat tightness | Vomiting, diarrhea, abdominal cramps, nausea |
| Soy | Skin rash, eczema, hives, itching | Runny nose, congestion, sneezing, coughing | Vomiting, diarrhea, abdominal pain |
Diagnostic Methods for Childhood Allergies
Identifying the specific cause of a child’s allergy symptoms is crucial for effective management and treatment. Accurate diagnosis allows for personalized strategies to minimize exposure to allergens and prevent severe reactions. Different diagnostic methods provide varying levels of accuracy and are often used in combination to reach a definitive conclusion.
Finding the right allergy treatments for kids can be tricky, especially when other issues crop up. For example, if your child is experiencing pain in the back of their knee while walking, it could be something completely unrelated to allergies, like pain in back of knee when walking. Thankfully, there are many effective allergy treatments available, so don’t hesitate to talk to your pediatrician about options.
A proper diagnosis is key to finding the best solution for your child’s specific needs.
Common Diagnostic Tests
Various tests are used to pinpoint allergies in children. These tests help identify potential triggers and guide treatment decisions. Careful consideration of the results is essential, as false positives and negatives can occur.
Skin Prick Tests
Skin prick tests are a common and relatively quick method for identifying allergies. The procedure involves placing small amounts of suspected allergens on the skin, usually the forearm. A tiny prick is made in the skin above the allergen, allowing the allergen to contact the underlying tissues. A positive reaction, such as redness, swelling, or hives at the prick site, indicates an allergic response.
The severity of the reaction correlates with the degree of sensitivity to the allergen.
Blood Tests
Blood tests, such as specific IgE blood tests, measure the levels of immunoglobulin E (IgE) antibodies in the blood. IgE antibodies are produced by the immune system in response to allergens. Elevated levels of specific IgE antibodies to particular allergens suggest an allergic reaction. This method is helpful when skin prick tests are not suitable or feasible.
Comparison of Diagnostic Methods
Both skin prick tests and blood tests have their advantages and disadvantages. The accuracy and reliability of each method can vary depending on factors like the child’s age, the type of allergen, and the experience of the healthcare professional. These factors are essential to consider when evaluating the results.
| Test | Pros | Cons |
|---|---|---|
| Skin Prick Test | Relatively quick and easy; can identify multiple allergens simultaneously; less expensive than some blood tests; often suitable for younger children; immediate results. | Can cause mild skin reactions; not suitable for children with severe skin conditions or those taking certain medications; false-negative results are possible; potential for false-positive results; requires careful interpretation. |
| Blood Test | Useful when skin prick tests are not possible; provides a more comprehensive overview of the immune response; can identify allergies to allergens that are difficult to test with skin prick tests; can be used to monitor the effectiveness of treatment over time. | More expensive than skin prick tests; takes longer to get results; may not always correlate directly with the severity of symptoms; requires a blood draw, which can be stressful for some children. |
Treatment Options for Childhood Allergies: Allergy Treatments For Kids
Treating childhood allergies requires a multifaceted approach, encompassing both immediate relief and long-term management strategies. Understanding the different treatment options and their effectiveness is crucial for parents and caregivers to make informed decisions about their child’s care. A personalized plan, developed in consultation with a pediatrician, is essential to ensure the best possible outcomes.
Pharmacological Treatments
Various medications can help alleviate allergy symptoms. Antihistamines are commonly prescribed to block the effects of histamine, a chemical released during an allergic reaction. These medications can effectively reduce itching, sneezing, and runny noses. Some antihistamines are available over-the-counter, while others require a prescription. It’s important to note that different antihistamines have varying degrees of effectiveness and potential side effects.
Consult a healthcare professional for appropriate recommendations.
Finding the right allergy treatments for kids can be tricky, especially when considering all the options. Sometimes, a child might not respond well to certain medications, like GLP-1 drugs. If you’re wondering if a GLP-1 drug isn’t working for you, check out this helpful article on signs glp 1 drugs dont work for you.
Understanding these signs can help guide your discussion with the pediatrician to find a more suitable allergy treatment plan for your child.
Immunotherapy
Allergen immunotherapy, also known as allergy shots, is a long-term treatment option for children with allergies. It involves gradually exposing the child to increasing amounts of allergens over time. This process aims to desensitize the immune system, reducing the body’s reaction to allergens. While allergy shots can be very effective, they require a significant commitment to regular appointments and can sometimes cause mild side effects.
Successful immunotherapy often leads to a decreased reliance on other allergy medications.
Environmental Control
Identifying and minimizing exposure to allergens in the child’s environment is crucial. This involves measures like controlling indoor dust mites, pet dander, and mold. Strategies include using allergen-proof bedding, regularly cleaning and vacuuming, and keeping pets out of bedrooms. Proper environmental control is often a critical component of a comprehensive allergy management plan, especially for children with severe allergies.
Dietary Avoidance
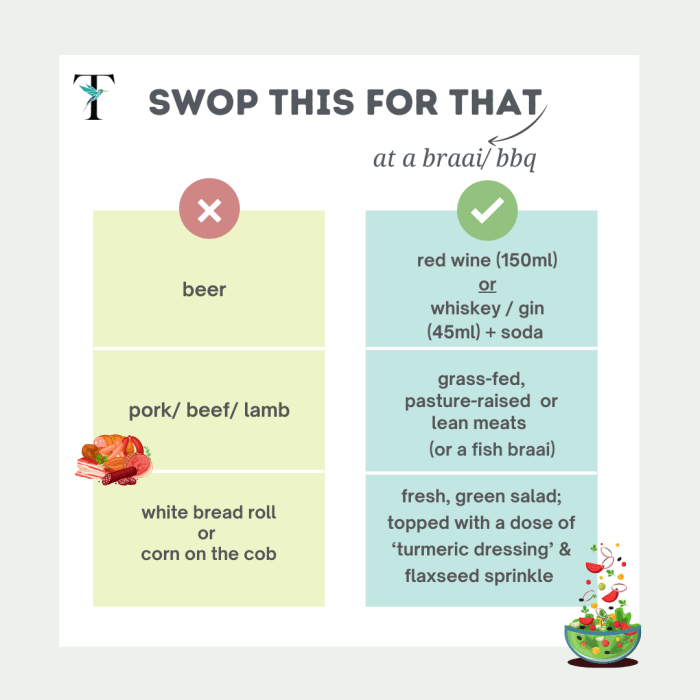
Avoiding allergenic foods is paramount in managing food allergies. This involves careful reading of food labels, educating family members and caregivers about potential allergens, and creating an environment that prioritizes safe food preparation and consumption. Severe food allergies can trigger life-threatening reactions, making meticulous avoidance essential.
Allergen-Free Recipes for Children
Creating delicious and nutritious meals without allergens is achievable. Here are some examples of allergen-free recipes for children:
- Peanut-Free Peanut Butter Alternatives: Sunflower seed butter, almond butter, or cashew butter can be used as substitutes in recipes. These can be spread on toast, used in smoothies, or added to homemade trail mix.
- Dairy-Free Smoothies: Smoothies can be easily made dairy-free using plant-based milk alternatives like almond milk, soy milk, or oat milk. Fruit, vegetables, and protein powder can be added for a complete and nutritious meal.
- Egg-Free Pancakes: Banana, apple, or mashed sweet potato can be incorporated into pancake recipes to replace eggs. These pancakes can be served with fresh fruit and maple syrup.
These examples demonstrate that children can enjoy delicious meals even with dietary restrictions. Remember to consult with a registered dietitian or allergist for personalized guidance on creating safe and nutritious meal plans for your child.
Management Strategies for Families

Navigating the world of childhood allergies can feel overwhelming. However, with proactive strategies and a well-informed approach, families can effectively manage these conditions and empower their children to live full and healthy lives. Understanding the nuances of allergy management is crucial for both immediate and long-term well-being.Effective allergy management involves more than just medications; it necessitates a comprehensive approach that encompasses home environment, school preparedness, and open communication with the child.
This requires a partnership between parents, healthcare professionals, and educators to create a supportive network for the child’s well-being.
Managing Allergies at Home
Creating an allergy-friendly home environment is paramount. This involves identifying and minimizing exposure to allergens. Dust mites, pet dander, mold, and pollen can all trigger allergic reactions. Regular cleaning, especially in bedrooms, is essential. Using allergen-proof bedding and vacuuming with HEPA filters can significantly reduce exposure.
If pets are present, regular grooming and limiting their access to certain areas can also help.
Importance of Early Intervention and Education
Early intervention and education are critical components of allergy management. The sooner a child’s allergies are diagnosed and managed, the better equipped they are to navigate daily life. This includes educating the child about their condition and teaching them how to recognize and avoid triggers. Education fosters a sense of responsibility and empowers the child to actively participate in their care.
Managing Allergic Reactions in School Settings
Collaborating with schools is vital for managing allergic reactions during school hours. This involves developing an action plan in conjunction with the child’s healthcare provider. The plan should detail the specific allergens, symptoms, and steps to take in case of a reaction. A clear communication protocol between parents and school staff is essential. This includes providing the school with emergency medication, instructions for administration, and a list of emergency contacts.
Having a designated trained staff member familiar with the plan is crucial.
Teaching Children About Their Allergies
Age-appropriate education is crucial for teaching children about their allergies. For younger children, simple explanations and visual aids can be helpful. Older children can understand more complex information, including the science behind allergies and the importance of avoidance. Encouraging the child to participate in decision-making and take responsibility for their health fosters a sense of empowerment and self-reliance.
This can involve keeping a diary or log of their symptoms, or even participating in discussions with healthcare professionals.
Resources for Families Dealing with Childhood Allergies, Allergy treatments for kids
Numerous resources are available to support families dealing with childhood allergies. These include support groups, online forums, and educational materials from reputable organizations. Connecting with other families facing similar challenges can provide valuable insights, emotional support, and practical advice.
| Resource Type | Examples |
|---|---|
| Support Groups | Local allergy support groups, online forums, parent-to-parent networks |
| Educational Materials | Websites of organizations like the Asthma and Allergy Foundation of America (AAFA), patient education materials from healthcare providers |
“Early intervention and education are critical for children with allergies. They empower the child to understand and manage their condition.”
Medications for Treating Allergic Reactions
Treating allergic reactions in children often involves a combination of strategies, and medications play a crucial role in managing symptoms and preventing severe complications. Prompt and appropriate medication administration can significantly improve a child’s comfort and well-being. Understanding the various medications, their dosages, and potential side effects is essential for parents and caregivers.
Common Medications Used
Different medications are used to target various aspects of an allergic reaction. These include antihistamines, epinephrine, and corticosteroids, each with specific roles and potential benefits.
Antihistamines
Antihistamines work by blocking the effects of histamine, a chemical released during allergic reactions. They are commonly used to treat mild to moderate allergic symptoms like itching, runny nose, and sneezing. Over-the-counter (OTC) antihistamines are frequently prescribed for children, and are often effective in reducing these symptoms.
- Dosage and Administration: Dosage varies greatly depending on the specific medication and the child’s age and weight. It’s crucial to follow the directions on the prescription label or provided by the pediatrician precisely. Oral administration is the most common method. Some antihistamines are also available in liquid form for easier administration, especially for younger children.
- Potential Side Effects: Common side effects include drowsiness, dry mouth, and stomach upset. More serious side effects are rare but possible. Parents should be aware of any unusual reactions and report them to their pediatrician immediately.
- Effectiveness and Safety Profile: Antihistamines are generally well-tolerated and effective for managing mild to moderate allergic reactions. However, their effectiveness in preventing severe reactions or anaphylaxis is limited. The choice of antihistamine and dosage will depend on the specific child and the severity of their allergy.
Epinephrine
Epinephrine is a crucial medication for treating severe allergic reactions, also known as anaphylaxis. It works rapidly to reverse the effects of anaphylaxis by constricting blood vessels and opening airways.
- Dosage and Administration: Epinephrine is typically administered via an auto-injector (e.g., EpiPen). The dosage and administration method are crucial in anaphylaxis. Proper training on the use of the auto-injector is essential for both parents and caregivers.
- Potential Side Effects: Common side effects of epinephrine include increased heart rate, anxiety, and tremors. More serious side effects are rare but can occur, including high blood pressure or chest pain. Careful monitoring is important during and after administration.
- Effectiveness and Safety Profile: Epinephrine is the first-line treatment for anaphylaxis and is vital in preventing life-threatening complications. Its rapid action makes it essential for immediate administration. However, the potential side effects require careful monitoring and understanding.
Corticosteroids
Corticosteroids are potent anti-inflammatory medications that can be used to reduce inflammation associated with allergic reactions. They are often prescribed for more severe allergic reactions, or when antihistamines are not sufficient.
- Dosage and Administration: Corticosteroids are available in various forms, including oral tablets, nasal sprays, and inhalers. The dosage and administration method will depend on the specific condition and the child’s age. Following the prescribed dosage and administration schedule is critical for optimal effectiveness.
- Potential Side Effects: Side effects of corticosteroids can vary depending on the route of administration and the dosage. Possible side effects include increased appetite, weight gain, and mood changes. Long-term use can have more serious effects, such as growth suppression or weakening of bones. Parents should be aware of any potential risks and discuss them with the pediatrician.
- Effectiveness and Safety Profile: Corticosteroids are effective in reducing inflammation and controlling symptoms of allergic reactions. However, their long-term use needs to be carefully considered due to the potential side effects. They should be used only when necessary and under the guidance of a healthcare professional.
Medication Summary Table
| Medication Type | Use Case | Potential Side Effects |
|---|---|---|
| Antihistamines | Mild to moderate allergic symptoms (itching, runny nose, sneezing) | Drowsiness, dry mouth, stomach upset |
| Epinephrine | Severe allergic reactions (anaphylaxis) | Increased heart rate, anxiety, tremors, high blood pressure |
| Corticosteroids | Severe allergic reactions, inflammation control | Increased appetite, weight gain, mood changes, growth suppression, bone weakening |
Preventive Measures and Long-Term Management

Managing childhood allergies requires a proactive approach that extends beyond immediate treatment. This involves understanding preventative measures and establishing strategies for long-term management. A comprehensive plan ensures children can lead healthy, fulfilling lives despite their allergies.Effective allergy management often hinges on recognizing triggers and avoiding them. Consistent monitoring and follow-up appointments play a vital role in adjusting treatment plans as needed.
A well-structured approach allows families to navigate the challenges of childhood allergies effectively.
Preventing Allergic Reactions
Understanding and avoiding triggers is paramount in preventing allergic reactions. This involves meticulous identification and subsequent avoidance of specific allergens.
Finding the right allergy treatments for kids can be tricky, but understanding how different medications work is key. For example, treatments like symbicort, dulera, advair, and breo are often prescribed to manage asthma, conditions sometimes linked to allergies. Learning more about these options can be helpful for parents. Check out this resource on symbicort dulera advair and breo to treat asthma for a deeper dive into how these inhalers can help.
Ultimately, open communication with your child’s doctor is crucial for selecting the most suitable allergy treatments.
- Identifying Allergens: Regular allergy testing and meticulous tracking of symptoms can pinpoint specific allergens. This information allows for the development of targeted avoidance strategies. For instance, if a child experiences hives after consuming peanuts, avoiding peanuts becomes a crucial preventive measure.
- Environmental Control: Minimizing exposure to common allergens in the home and surroundings is a key preventative step. Controlling dust mites, mold, and pet dander through regular cleaning and other environmental modifications can significantly reduce the risk of allergic reactions.
- Proper Hygiene Practices: Maintaining good hygiene practices, such as regular handwashing and avoiding direct contact with known allergens, can also help prevent allergic reactions.
Importance of Regular Monitoring and Follow-up
Regular monitoring and follow-up appointments are essential for managing allergies effectively. These appointments allow for adjustments to treatment plans based on the child’s evolving needs.
- Tracking Symptoms: Tracking symptoms, including the severity and frequency of reactions, provides valuable data for healthcare professionals to assess treatment effectiveness and make necessary adjustments.
- Adjusting Treatment Plans: As children grow, their allergies may evolve. Regular check-ups enable healthcare providers to monitor the child’s response to treatment and adjust medications or therapies as needed.
- Early Intervention: Early detection and intervention are critical. Regular monitoring allows for early identification of emerging issues and helps in preventing more severe reactions.
Strategies for Long-Term Management
Long-term allergy management requires a comprehensive approach encompassing avoidance strategies, medication adherence, and regular monitoring. A personalized plan tailored to each child’s specific needs is crucial for success.
- Personalized Action Plans: Developing personalized action plans for managing allergic reactions helps parents and caregivers understand the steps to take during a reaction. This can include specific medication dosages and administration instructions.
- Medication Adherence: Adherence to prescribed medications is critical for controlling allergies. Consistent medication use prevents exacerbations and minimizes the severity of allergic reactions.
- Lifestyle Modifications: Implementing lifestyle modifications, such as avoiding known allergens and maintaining a healthy diet, can significantly improve long-term allergy management.
The Role of Immunotherapy
Immunotherapy, a long-term treatment option, involves gradually introducing increasing amounts of allergens to the body, thereby desensitizing the immune system. This approach can significantly reduce the severity and frequency of allergic reactions over time.
- Desensitization: Immunotherapy aims to desensitize the immune system to specific allergens, effectively reducing the body’s response to them.
- Long-Term Relief: Immunotherapy can offer long-term relief from allergies, potentially reducing the need for frequent medications and minimizing the impact of allergic reactions.
- Suitable for Specific Allergies: Immunotherapy is often a suitable option for certain types of allergies, such as pollen allergies, insect venom allergies, and food allergies.
Addressing Specific Allergies
Understanding and managing childhood allergies requires a nuanced approach, tailoring treatment to the specific allergen. This section delves into common allergies like peanut, milk, and egg allergies, examining treatment strategies, long-term implications, and success stories. These allergies often require a multifaceted approach, encompassing both immediate reactions and long-term management.Specific allergies, like peanut allergies, demand careful attention to prevent severe reactions.
Proper identification and management strategies are crucial for minimizing long-term consequences.
Peanut Allergy
Peanut allergy is a significant concern, frequently leading to severe allergic reactions. Early diagnosis and strict avoidance are paramount. Treatment protocols typically focus on emergency preparedness, including epinephrine auto-injectors (e.g., EpiPen), and a thorough understanding of triggers.
- Emergency Preparedness: Families should have a plan for immediate action, including the location and use of epinephrine auto-injectors, and clear communication with schools and childcare providers. This proactive approach minimizes the risk of a severe reaction.
- Dietary Restrictions: Strict avoidance of peanuts and peanut products is essential. Cross-contamination is a significant risk, requiring vigilance in food preparation and handling. Label reading and careful selection of foods are crucial for avoiding accidental exposure.
- Long-Term Implications: Peanut allergy can have significant long-term implications, potentially impacting dietary choices, social interactions, and overall quality of life. Ongoing monitoring and management are vital for mitigating these consequences. A potential complication involves the development of other allergies (e.g., tree nuts).
Milk Allergy
Milk allergy is common in young children, often presenting with gastrointestinal symptoms. Early identification and dietary modifications are key to managing this allergy.
- Dietary Management: Strict avoidance of milk and milk-containing products is essential. This includes dairy-based foods, beverages, and processed products that may contain milk as an ingredient. Alternative milk options, such as soy or almond milk, need to be carefully selected.
- Symptoms and Management: Recognition of symptoms, like skin rashes, digestive upset, or respiratory difficulties, is crucial. Parents should work closely with allergists to understand and manage potential reactions effectively.
- Long-Term Implications: Milk allergy can influence nutritional intake and overall health, particularly in terms of calcium and vitamin D absorption. Carefully planned diets and supplementation can help address nutritional needs. The allergy often resolves in childhood, though not always.
Egg Allergy
Egg allergy is another common childhood allergy, potentially causing a range of symptoms. Early diagnosis and avoidance strategies are vital for managing this allergy.
- Allergen Avoidance: Strict avoidance of egg and egg-containing foods is critical. This includes baked goods, sauces, and processed foods. Cross-contamination during food preparation requires meticulous attention to detail.
- Symptom Recognition: Identifying the specific symptoms of an egg allergy is essential for appropriate management. These symptoms can range from skin rashes to respiratory issues. Recognizing patterns is key to early intervention.
- Long-Term Management: Egg allergy typically improves or resolves with age, though some children may experience persistent symptoms. Ongoing monitoring and communication with healthcare providers are necessary. It is possible for children to develop other allergies, including milk, in conjunction with an egg allergy.
Educational Resources for Parents
Navigating the world of childhood allergies can feel overwhelming. Knowing where to turn for reliable information and support is crucial for managing your child’s health effectively. This section offers a range of resources to empower you with knowledge and practical strategies.
Reliable Websites and Organizations
Understanding the diverse spectrum of resources available can simplify the journey. A plethora of websites and organizations provide invaluable information, support, and community for parents dealing with allergies.
- The American Academy of Allergy, Asthma & Immunology (AAAAI): A leading medical organization, the AAAAI offers comprehensive information on various allergies, including diagnosis, treatment, and management strategies. Their website is a trusted source for evidence-based information and up-to-date guidelines.
- The Food Allergy & Anaphylaxis Network (FAAN): FAAN is a dedicated resource for families affected by food allergies. They provide crucial support, advocacy, and educational materials, including information on anaphylaxis prevention and management.
- The Asthma and Allergy Foundation of America (AAFA): AAFA offers a wealth of information on asthma, allergies, and related conditions. Their resources cover various aspects, from diagnosis to treatment, and they often host support groups for families.
- The National Institutes of Health (NIH): The NIH provides access to a wide range of health information, including allergy-related research and clinical trials. This is a great resource for staying informed about the latest advancements in allergy science.
Books for Parents
Books can provide valuable insights and practical guidance. They offer a deeper dive into specific topics and often include personal stories, which can be incredibly helpful.
- The Food Allergy Survival Guide by Dr. Robert G. Hamilton: This book is a practical guide for families navigating the complexities of food allergies, offering practical strategies and advice for managing the condition.
- Living with Allergies by [Author Name]: This book may offer various perspectives and provide additional insight for parents, providing different points of view and approaches to managing allergies.
Managing Allergies in the Classroom
Effective allergy management in schools is crucial for children’s safety and well-being. Collaboration between parents, teachers, and school staff is essential for creating a supportive environment.
- Communication is Key: Maintain open communication with teachers and school staff about your child’s allergy. Provide them with detailed information about the specific allergy, including triggers, symptoms, and emergency procedures. Regular check-ins and updates are important for proactive management.
- Emergency Action Plans (EAPs): Ensure your child’s school has a comprehensive EAP in place. This plan should Artikel specific steps to be taken in case of an allergic reaction, including the administration of medications (if applicable), and contact information for emergency personnel.
- Classroom Accommodations: Work with the school to create a safe and supportive learning environment. Discuss strategies to minimize exposure to allergens, such as avoiding certain foods or cleaning procedures. This might include dedicated storage areas for allergy-free snacks and drinks.
The Role of Schools in Supporting Children with Allergies
Schools play a pivotal role in the safe and successful education of children with allergies. A supportive school environment can greatly impact a child’s well-being and academic success.
- Training Staff: Schools should provide allergy awareness training for all staff members. This training should cover recognizing symptoms of allergic reactions, understanding the school’s EAP, and proper administration of medications.
- Designated Staff: Designating staff members to be responsible for managing allergies can improve coordination and ensure quick responses in case of emergencies.
- Accessibility to Medications: Ensuring that emergency medications are readily available and properly stored in the school is crucial. Establish clear protocols for access and administration.
Educating Children about Their Allergies
Teaching children about their allergies empowers them to take an active role in managing their health. Open communication and age-appropriate education are key to building confidence and independence.
- Age-Appropriate Education: Tailor the information to your child’s developmental stage. Young children may benefit from simple explanations and visual aids, while older children can understand more complex details. This can involve using age-appropriate visuals, role-playing, and interactive games.
- Independence and Responsibility: Encourage your child to understand their allergy triggers and symptoms. Involve them in managing their allergy, providing them with the knowledge and tools to stay safe. Teach them to recognize signs of an allergic reaction and the importance of seeking help immediately.
- Peer Support: If appropriate, consider strategies to help children with allergies feel supported by their peers. This could include support groups or classroom discussions about allergies.
Outcome Summary
In conclusion, navigating childhood allergies requires a multifaceted approach encompassing diagnosis, treatment, and proactive management. This guide equips parents and caregivers with the knowledge and resources necessary to support children with allergies, promoting their overall health and well-being. Remember that early intervention, open communication, and consistent monitoring are key to successful long-term management.