Types of lung disease what you should know – Types of lung disease: what you should know. Understanding the respiratory system and the various lung diseases that can affect it is crucial for overall health. This comprehensive guide delves into the different types of lung diseases, their causes, symptoms, and treatment options. We’ll explore the impact these conditions have on daily life and offer strategies for prevention and management.
From common conditions like asthma and chronic bronchitis to rarer but serious diseases, this guide will equip you with the knowledge to navigate this complex topic. We’ll cover everything from the basic anatomy of a healthy lung to the differences in symptoms and treatments for various types. This will also explore the role of environmental factors, lifestyle choices, and genetics in developing lung diseases.
Introduction to Lung Diseases
Our lungs are the vital organs responsible for breathing, a process essential for life. They take in oxygen from the air and release carbon dioxide, enabling our bodies to function. This intricate system, comprising airways, alveoli, and blood vessels, is a marvel of biological engineering. Understanding the respiratory system’s structure and function is crucial to grasping the impact of lung diseases.Lung diseases are conditions that affect the normal functioning of the lungs.
These conditions can range from mild to severe, impacting a person’s quality of life significantly. They can interfere with the lungs’ ability to deliver oxygen to the bloodstream and remove carbon dioxide, leading to a cascade of health issues. The specific symptoms and complications depend heavily on the type of lung disease.
Overview of the Respiratory System
The respiratory system is a complex network of organs and structures working together to facilitate gas exchange. Air enters the body through the nose or mouth, travels down the trachea (windpipe), and branches into smaller and smaller airways called bronchi. These bronchi eventually lead to tiny air sacs called alveoli. The alveoli are surrounded by a network of capillaries, tiny blood vessels.
It is in these alveoli that the exchange of oxygen and carbon dioxide occurs. Oxygen from the air diffuses into the bloodstream, while carbon dioxide from the bloodstream diffuses into the air sacs to be expelled.
Common Symptoms of Lung Diseases
A variety of symptoms can indicate lung disease. These can include shortness of breath (dyspnea), coughing (which may produce mucus), chest pain, wheezing, and fatigue. The severity and frequency of these symptoms can vary greatly depending on the specific disease and its progression. Some individuals may experience only mild discomfort, while others may have severe breathing difficulties.
Factors like the underlying cause, the individual’s overall health, and the stage of the disease all play a role in symptom presentation.
Comparison of Healthy vs. Diseased Lung
| Characteristic | Healthy Lung | Diseased Lung |
|---|---|---|
| Structure | Elastic, spongy tissue with millions of alveoli. Bronchial tubes are clear and open. | Alveoli may be damaged, inflamed, or filled with fluid or mucus. Bronchial tubes may be narrowed or obstructed. Tissue may be scarred or thickened. |
| Color | Light, pinkish-gray | May appear darker, gray, or congested, depending on the disease. |
| Function | Efficient gas exchange, taking in oxygen and releasing carbon dioxide. | Reduced gas exchange capacity, potentially leading to hypoxia (low oxygen levels in the blood). |
| Texture | Soft and flexible | May be stiff or less elastic, depending on the specific disease. |
This table provides a basic comparison. The specific appearance and characteristics of a diseased lung will vary significantly depending on the type of lung disease.
Types of Lung Diseases
Understanding the various types of lung diseases is crucial for effective diagnosis and treatment. Lung diseases encompass a broad spectrum of conditions, affecting millions globally. Early detection and appropriate management are key to improving patient outcomes.
Major Categories of Lung Diseases
Lung diseases are broadly categorized based on their underlying mechanisms. These categories help clinicians identify potential causes and develop targeted interventions. The primary classifications include infectious, inflammatory, genetic, and obstructive diseases.
Infectious Lung Diseases
Infectious lung diseases are caused by pathogens like bacteria, viruses, and fungi. These pathogens invade the lungs, triggering an inflammatory response and potentially leading to severe complications. Examples include pneumonia, tuberculosis, and influenza. Pneumonia, a common infectious lung disease, can be caused by various microorganisms, leading to lung inflammation and fluid buildup. Tuberculosis, caused by the bacteriumMycobacterium tuberculosis*, often affects the lungs but can spread to other organs.
Influenza, a viral infection, can result in severe respiratory complications.
Inflammatory Lung Diseases
Inflammatory lung diseases involve the immune system’s response to an irritant or trigger. The immune system overreacts, leading to chronic inflammation in the lungs. Examples include asthma, chronic bronchitis, and hypersensitivity pneumonitis. Asthma is characterized by chronic airway inflammation, making breathing difficult. Chronic bronchitis is marked by long-term inflammation of the bronchial tubes, causing persistent cough and mucus production.
Understanding different types of lung disease is crucial for preventative care. One factor that might impact lung health is the presence of limonene, a compound found in citrus fruits. Learning more about limonene’s potential effects on the body can help you make informed decisions about your health, particularly if you’re concerned about lung health. For a deeper dive into the fascinating world of limonene, check out this article: what to know about limonene.
Ultimately, staying informed about potential lung issues is key to maintaining overall well-being.
Hypersensitivity pneumonitis occurs when the immune system reacts to inhaled substances like mold or dust.
Genetic Lung Diseases
Genetic lung diseases are inherited conditions that affect the structure and function of the lungs. These conditions often manifest in childhood or adolescence and can lead to progressive lung damage. Cystic fibrosis, a common example, involves mutations in a gene that affects mucus production, leading to thickened mucus that obstructs airways. Alpha-1 antitrypsin deficiency is another example, impacting the body’s ability to protect the lungs from damage.
Obstructive Lung Diseases
Obstructive lung diseases are characterized by narrowing or blockage of the airways, hindering airflow. Examples include chronic obstructive pulmonary disease (COPD), emphysema, and bronchiectasis. COPD is a progressive lung disease characterized by chronic bronchitis and emphysema, leading to airflow limitations. Emphysema damages the air sacs in the lungs, resulting in reduced lung capacity. Bronchiectasis is characterized by the permanent widening of the airways, making them prone to infection.
Table Categorizing Lung Diseases
| Category | Examples | Primary Characteristics |
|---|---|---|
| Infectious | Pneumonia, Tuberculosis, Influenza | Caused by pathogens |
| Inflammatory | Asthma, Chronic Bronchitis, Hypersensitivity Pneumonitis | Immune system overreaction |
| Genetic | Cystic Fibrosis, Alpha-1 Antitrypsin Deficiency | Inherited conditions |
| Obstructive | COPD, Emphysema, Bronchiectasis | Airway narrowing/blockage |
Rare but Important Lung Diseases
Rare lung diseases can be just as debilitating as common ones. While less prevalent, they demand specialized attention and care. Examples include pulmonary hypertension, pulmonary alveolar proteinosis, and sarcoidosis. Pulmonary hypertension involves high blood pressure in the arteries of the lungs, making it difficult for the heart to pump blood. Pulmonary alveolar proteinosis is a condition where protein accumulates in the air sacs, interfering with gas exchange.
Sarcoidosis is a disease where inflammatory cells form granulomas in various organs, including the lungs.
Causes and Risk Factors: Types Of Lung Disease What You Should Know
Understanding the causes and risk factors for lung diseases is crucial for prevention and early detection. Numerous factors contribute to the development of these conditions, encompassing environmental exposures, occupational hazards, genetic predispositions, and lifestyle choices. Identifying these risk factors allows individuals to make informed decisions to minimize their chances of developing lung-related illnesses.Environmental factors play a significant role in the development of lung diseases.
Air pollution, both indoor and outdoor, can expose individuals to harmful particles and gases that irritate the lungs and compromise their function. Exposure to secondhand smoke and other airborne pollutants can contribute to the development of chronic respiratory conditions.
Environmental Factors
Environmental exposures to pollutants and irritants are significant contributors to lung diseases. Air pollution, particularly particulate matter and ozone, is a major environmental risk factor. These pollutants can damage the delicate tissues of the lungs, leading to inflammation and chronic respiratory problems. Exposure to secondhand smoke, both indoors and outdoors, poses a serious threat to lung health.
Indoor air pollution from sources such as cooking fumes and mold can also negatively impact lung function.
Occupational Hazards
Certain occupations expose individuals to hazardous substances that increase the risk of lung diseases. Workers in industries such as mining, construction, and manufacturing may be exposed to silica dust, asbestos, and other harmful materials. Prolonged exposure to these substances can lead to severe lung conditions like silicosis, asbestosis, and lung cancer. Understanding these occupational hazards is essential for implementing appropriate safety measures and reducing the risk of work-related lung diseases.
Knowing the different types of lung diseases is crucial for your health. From chronic obstructive pulmonary disease (COPD) to asthma, understanding these conditions can help you take proactive steps toward better management. Learning about the various support systems, like the options for urinary catheters, such as foley catheters and other types of urinary catheters , can be vital for overall well-being.
Ultimately, recognizing the types of lung diseases and their related care options is a key part of staying informed and healthy.
- Mining: Workers in mining operations are frequently exposed to silica dust, a major risk factor for silicosis, a debilitating lung disease.
- Construction: Construction workers are at risk from exposure to asbestos, which can cause asbestosis, a progressive lung disease.
- Manufacturing: Certain manufacturing processes can expose workers to harmful chemicals and dust, increasing their risk of various lung diseases.
Genetic Predisposition
Genetic factors can influence an individual’s susceptibility to developing lung diseases. Certain genetic mutations or inherited conditions can make individuals more vulnerable to lung disorders. Family history of lung cancer or other respiratory illnesses can indicate a potential genetic predisposition. However, genetic predisposition does not guarantee disease development, and lifestyle choices and environmental factors still play a crucial role.
Lifestyle Factors
Lifestyle choices significantly influence the risk of developing lung diseases. Smoking is the leading preventable cause of lung cancer and chronic obstructive pulmonary disease (COPD). Exposure to tobacco smoke damages the delicate tissues of the lungs, leading to inflammation and impaired function. Other lifestyle factors, such as poor diet and lack of physical activity, can also contribute to lung-related issues.
- Smoking: Cigarette smoking is the single most significant lifestyle risk factor for lung cancer and COPD. The harmful chemicals in cigarette smoke damage lung tissue and impair respiratory function.
- Diet and Exercise: A poor diet and lack of physical activity can contribute to inflammation and reduced lung function, increasing the risk of respiratory issues.
Summary Table of Risk Factors
| Type of Lung Disease | Environmental Factors | Occupational Hazards | Genetic Predisposition | Lifestyle Factors |
|---|---|---|---|---|
| Lung Cancer | Air pollution, secondhand smoke | Exposure to asbestos, silica dust | Family history of lung cancer | Smoking, poor diet |
| COPD | Air pollution, secondhand smoke | Exposure to dust, fumes | Family history of COPD | Smoking, lack of exercise |
| Asthma | Air pollution, allergens | Exposure to irritants | Family history of asthma | Allergies, smoking exposure |
Symptoms and Diagnosis
Understanding the symptoms and diagnostic procedures is crucial for early detection and effective management of lung diseases. Early diagnosis allows for timely intervention, potentially improving treatment outcomes and quality of life. Recognizing the specific symptoms associated with different types of lung diseases can significantly aid in the diagnostic process.
Common Symptoms of Lung Diseases
Lung diseases manifest in a variety of ways, often affecting breathing, energy levels, and overall well-being. Common symptoms include persistent coughing, shortness of breath (dyspnea), chest pain, wheezing, and fatigue. These symptoms can range from mild to severe, and their intensity can fluctuate over time. Some symptoms may be subtle or easily overlooked, potentially delaying diagnosis.
Symptoms Differing Across Lung Disease Types
The presentation of symptoms varies significantly depending on the specific lung disease. For example, chronic obstructive pulmonary disease (COPD) typically presents with progressive shortness of breath, chronic cough, and sputum production. Asthma, on the other hand, often manifests with intermittent wheezing, chest tightness, and coughing, especially triggered by allergens or irritants. Infiltrative lung diseases like sarcoidosis may present with a dry cough, fever, and general malaise, sometimes mimicking other illnesses.
Diagnostic Tests for Lung Diseases
Various diagnostic tests are employed to identify lung diseases. These tests include physical examinations, pulmonary function tests (PFTs), blood tests, and imaging studies. A thorough physical examination, including listening to the lungs with a stethoscope, can reveal signs suggestive of certain lung conditions. PFTs measure lung capacity and airflow, providing objective data about lung function. Blood tests can help identify inflammation or other markers associated with lung diseases.
Imaging Techniques in Lung Disease Diagnosis
Imaging plays a vital role in diagnosing lung diseases. X-rays provide basic images of the lungs, revealing abnormalities such as pneumonia, tumors, or fluid buildup. Computed tomography (CT) scans offer more detailed images, allowing visualization of structures within the lungs and surrounding tissues. CT scans are particularly useful in identifying subtle abnormalities and assessing the extent of lung disease.
The choice of imaging technique depends on the suspected diagnosis and the specific information needed.
Comparison of Imaging Techniques
| Imaging Technique | Description | Advantages | Disadvantages |
|---|---|---|---|
| X-ray | Simple, inexpensive, and readily available imaging method. | Quick, non-invasive, and good for detecting large abnormalities. | Limited detail, less sensitive for subtle changes. |
| CT Scan | Detailed cross-sectional images of the lungs and surrounding tissues. | High resolution, provides detailed information about the extent and location of the disease. | More expensive, involves radiation exposure. |
Common Symptoms and Associated Lung Diseases
The following table Artikels some common symptoms and the lung diseases they might be associated with. It is crucial to remember that this is not an exhaustive list and a healthcare professional should be consulted for accurate diagnosis.
| Symptom | Associated Lung Diseases |
|---|---|
| Persistent cough | COPD, bronchitis, lung cancer, asthma, cystic fibrosis |
| Shortness of breath (dyspnea) | COPD, asthma, pulmonary embolism, interstitial lung disease, heart failure |
| Wheezing | Asthma, COPD, bronchiolitis |
| Chest pain | Pleurisy, lung cancer, pneumonia, pulmonary embolism |
| Fatigue | Many lung diseases, including interstitial lung disease, lung cancer, and cystic fibrosis |
Treatment and Management
Treating lung diseases requires a multifaceted approach, tailored to the specific condition and the individual’s overall health. Effective management involves a combination of medical interventions, lifestyle adjustments, and ongoing support. The goal is to improve quality of life, control symptoms, and slow disease progression whenever possible.A personalized treatment plan is crucial, as the best approach varies significantly depending on the type and severity of the lung disease.
Factors like the patient’s age, overall health, and the presence of other medical conditions all play a role in determining the most appropriate course of action. Early detection and prompt intervention are key to maximizing treatment outcomes.
Medical Treatments
Various medical treatments are employed to address lung diseases. These include medications, therapies, and surgical interventions, each playing a specific role in managing symptoms and addressing the underlying causes.
- Medications: A wide range of medications is used to treat lung diseases. Bronchodilators, for example, relax the airways, making breathing easier. Corticosteroids can reduce inflammation. Antibiotics are used to combat infections, while immunosuppressants can help manage autoimmune conditions affecting the lungs. Specific medications target particular types of lung diseases, like targeted therapies for some cancers.
- Respiratory Therapies: These therapies aim to improve lung function and overall respiratory health. Examples include pulmonary rehabilitation programs, which often involve exercises and education to improve breathing techniques and stamina. Oxygen therapy can provide supplemental oxygen to patients with low blood oxygen levels.
- Surgical Interventions: In some cases, surgical procedures may be necessary to address lung diseases. This could include lung volume reduction surgery for emphysema or lung transplantation for severe cases of chronic lung disease. The decision to pursue surgery depends on the specific disease, its severity, and the patient’s overall health.
Lifestyle Changes
Lifestyle modifications can significantly impact the management of lung diseases. Adopting healthy habits can improve lung function, reduce symptoms, and enhance overall well-being.
- Smoking Cessation: Smoking is a significant risk factor for many lung diseases. Quitting smoking is one of the most important lifestyle changes a person can make to improve their lung health. Support groups, medications, and counseling can assist individuals in quitting.
- Nutrition and Exercise: A balanced diet and regular exercise can support lung health. A healthy diet provides essential nutrients, while regular exercise improves cardiovascular health and strengthens respiratory muscles. This is particularly important for individuals with conditions like chronic obstructive pulmonary disease (COPD).
- Environmental Factors: Exposure to irritants like pollutants and allergens can worsen lung conditions. Minimizing exposure to these triggers can help manage symptoms and improve lung function.
Importance of Early Detection and Intervention
Early detection and prompt intervention are crucial for managing lung diseases effectively. The earlier a diagnosis is made, the more options may be available to manage the disease, improve outcomes, and potentially prevent serious complications. This is especially true for conditions that progress over time, like chronic bronchitis and emphysema.
Knowing the different types of lung disease is crucial for your health. From chronic obstructive pulmonary disease (COPD) to asthma, understanding these conditions can empower you to make informed decisions about your well-being. However, did you know that some natural remedies, like St. John’s Wort, might interact with medications for lung conditions? For a comprehensive guide on everything you need to know about St.
John’s Wort, check out this article: everything you need to know about st johns wort. Ultimately, it’s always best to consult with a healthcare professional before trying any new remedies, especially when dealing with potential lung issues.
Treatment Comparison Table
| Lung Disease | Medication Examples | Therapy Examples | Surgical Options |
|---|---|---|---|
| Chronic Obstructive Pulmonary Disease (COPD) | Bronchodilators, corticosteroids, antibiotics | Pulmonary rehabilitation, oxygen therapy | Lung volume reduction surgery |
| Asthma | Bronchodilators, corticosteroids, leukotriene modifiers | Inhaler technique education | Rarely, but possible in severe cases |
| Cystic Fibrosis | Pancreatic enzymes, airway clearance therapies | Physiotherapy, nutritional support | Lung transplantation (in severe cases) |
| Lung Cancer | Chemotherapy, targeted therapies, radiation therapy | Palliative care, symptom management | Surgery, radiation therapy, chemotherapy |
Prevention and Education
Taking proactive steps to prevent lung diseases is crucial for maintaining respiratory health. Understanding the risk factors and implementing preventive measures can significantly reduce the likelihood of developing these conditions. Early detection and prompt treatment also play a vital role in improving outcomes.Preventing lung diseases involves a multifaceted approach encompassing lifestyle choices, vaccination strategies, and public health initiatives.
By understanding the causes and promoting healthy habits, individuals can significantly decrease their risk.
Strategies for Preventing Lung Diseases
Effective prevention strategies encompass various facets of a healthy lifestyle. A crucial element is avoiding exposure to harmful environmental factors. This includes limiting exposure to secondhand smoke, air pollution, and occupational hazards. Adopting a healthy diet and maintaining a healthy weight are also important components of prevention. Regular physical activity contributes to overall well-being, including respiratory health.
Importance of Vaccination and Screening
Vaccination against certain infectious agents plays a vital role in preventing lung infections. Pneumonia and influenza are examples of infections that can lead to serious complications, particularly in individuals with underlying lung conditions. Routine vaccinations, especially for the elderly and those with compromised immune systems, can significantly reduce the risk of these infections. Screening programs, such as those for lung cancer, are essential for early detection and treatment.
Early detection significantly improves treatment outcomes and reduces the likelihood of advanced stages.
Role of Public Health Initiatives
Public health initiatives play a crucial role in creating supportive environments for respiratory health. These initiatives include implementing smoke-free policies in public spaces, promoting awareness campaigns about air pollution, and advocating for improved air quality standards. Collaboration between public health agencies, healthcare providers, and communities is essential to effectively implement these programs. This collaborative effort ensures the dissemination of vital information, making preventive measures accessible to a wider population.
Educational Resources
Numerous educational resources are available to enhance understanding of lung diseases and their prevention. These include websites of reputable health organizations, educational materials provided by medical professionals, and public health campaigns. Educational resources offer valuable insights into risk factors, preventive measures, and early warning signs. By utilizing these resources, individuals can make informed decisions about their health and well-being.
Preventative Measures Individuals Can Take
- Avoid Tobacco Use: Smoking is a major risk factor for various lung diseases. Quitting smoking or avoiding tobacco use altogether is one of the most significant preventative steps individuals can take. Secondhand smoke also poses a risk, so avoiding exposure to smoke is equally important.
- Maintain a Healthy Diet and Weight: A balanced diet rich in fruits, vegetables, and whole grains, coupled with maintaining a healthy weight, supports overall respiratory health. Nutrients are vital for maintaining a strong immune system and promoting general well-being, thereby reducing the likelihood of infections and respiratory illnesses.
- Regular Exercise: Regular physical activity strengthens the respiratory system and improves overall health. Exercise contributes to better lung function and reduces the risk of chronic respiratory conditions.
- Limit Exposure to Environmental Pollutants: Reducing exposure to air pollution, secondhand smoke, and other environmental pollutants is essential for preventing lung diseases. Individuals should be mindful of their surroundings and take necessary precautions to minimize exposure to harmful substances.
- Get Vaccinated: Regular vaccination against influenza and pneumonia can significantly reduce the risk of lung infections. Vaccinations are particularly important for vulnerable populations, such as the elderly and those with chronic health conditions.
Living with Lung Disease
Living with a lung disease can be challenging, impacting every aspect of daily life. From the physical limitations to the emotional toll, understanding how to navigate these challenges is crucial for maintaining well-being. This section delves into the practical realities of living with lung conditions, highlighting support systems and strategies for coping.
Impact on Daily Life
Lung diseases often lead to reduced lung capacity and shortness of breath, significantly affecting activities of daily living. Simple tasks like climbing stairs, walking, or even talking can become strenuous or impossible. This can impact work, social life, and overall quality of life. Fatigue is another common symptom, making even basic self-care tasks difficult. The constant awareness of one’s condition and the need for careful management can lead to anxiety and depression.
Importance of Support Groups and Resources, Types of lung disease what you should know
Connecting with others facing similar challenges is invaluable. Support groups provide a safe space for sharing experiences, exchanging coping strategies, and offering mutual encouragement. These groups can offer a sense of community and reduce feelings of isolation. Additionally, accessing reliable resources like pulmonary rehabilitation programs, educational materials, and healthcare professionals specializing in lung diseases is essential. These resources provide crucial information, guidance, and support for effective management.
Adhering to Treatment Plans
Adherence to prescribed treatment plans is paramount for managing lung disease effectively. This includes taking medications as directed, attending appointments, and making lifestyle adjustments recommended by healthcare providers. A consistent approach ensures the best possible outcomes and prevents complications. Regular monitoring and adjustments to the treatment plan as needed, based on individual response, are critical components of successful management.
Coping Mechanisms for Managing Challenges
Developing effective coping mechanisms is essential for navigating the challenges of lung disease. These include stress management techniques such as meditation, yoga, or deep breathing exercises. Maintaining a healthy diet and regular exercise, as tolerated, can also improve overall well-being. Seeking professional help for emotional distress, such as counseling or therapy, is also beneficial. Building a strong support network with family and friends is equally important in providing emotional support and practical assistance.
Support Resources and Organizations
| Organization | Description | Contact Information (Example) |
|---|---|---|
| American Lung Association | Provides vital resources, support groups, and advocacy for lung health. | (Phone number) | (Website) |
| National Jewish Health | Offers comprehensive care for a range of respiratory conditions, including extensive research and educational programs. | (Phone number) | (Website) |
| The COPD Foundation | Dedicated to improving the lives of people with chronic obstructive pulmonary disease (COPD). | (Phone number) | (Website) |
| Local Pulmonary Rehabilitation Programs | Offers specialized exercise programs and educational sessions for managing lung conditions. | (Contact your local hospital or healthcare system) |
This table presents a small selection of valuable organizations. Many more local and national organizations exist that can offer support and guidance. It is highly recommended to research and connect with resources relevant to your specific lung condition.
Final Thoughts
In conclusion, understanding the diverse types of lung diseases, their causes, symptoms, and treatment options is vital for proactive health management. This comprehensive overview equips readers with the necessary knowledge to make informed decisions regarding their well-being and empowers them to take steps towards prevention. Remember that early detection and proactive management are key in ensuring a healthy life.




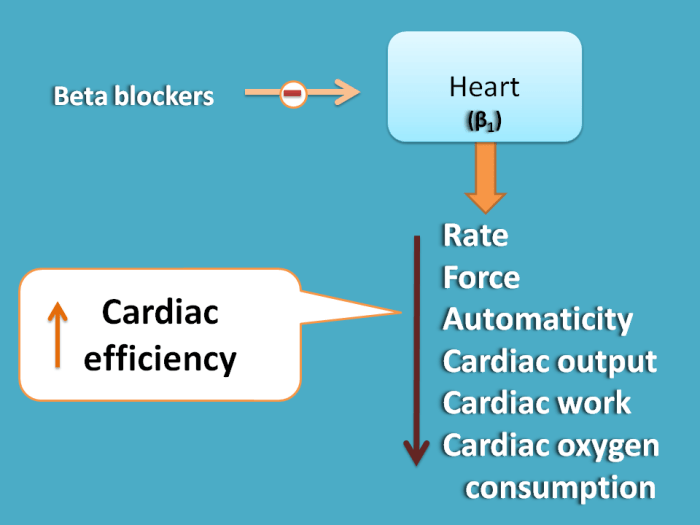

 Diagram Description: A diagram illustrating the renin-angiotensin-aldosterone system. The diagram depicts the sequential activation of enzymes and hormones, culminating in the production of angiotensin II and aldosterone. The diagram should show the key components like renin, angiotensinogen, angiotensin-converting enzyme (ACE), angiotensin II, and aldosterone. It should also visually demonstrate the effects of these hormones on blood vessels and the kidneys.
Diagram Description: A diagram illustrating the renin-angiotensin-aldosterone system. The diagram depicts the sequential activation of enzymes and hormones, culminating in the production of angiotensin II and aldosterone. The diagram should show the key components like renin, angiotensinogen, angiotensin-converting enzyme (ACE), angiotensin II, and aldosterone. It should also visually demonstrate the effects of these hormones on blood vessels and the kidneys. Diagram Description: A diagram showcasing the sympathetic nervous system’s impact on blood vessels. The diagram should depict the pathway of sympathetic nerve impulses, the release of norepinephrine, and the subsequent vasoconstriction of blood vessels. The diagram should highlight the involvement of alpha- and beta-adrenergic receptors in this process.
Diagram Description: A diagram showcasing the sympathetic nervous system’s impact on blood vessels. The diagram should depict the pathway of sympathetic nerve impulses, the release of norepinephrine, and the subsequent vasoconstriction of blood vessels. The diagram should highlight the involvement of alpha- and beta-adrenergic receptors in this process. Diagram Description: A diagram illustrating the mechanism of action of ACE inhibitors. The diagram should visually represent the normal conversion of angiotensin I to angiotensin II, and how ACE inhibitors inhibit this conversion. The diagram should highlight the decreased vasoconstriction and aldosterone release as a result of this inhibition.
Diagram Description: A diagram illustrating the mechanism of action of ACE inhibitors. The diagram should visually represent the normal conversion of angiotensin I to angiotensin II, and how ACE inhibitors inhibit this conversion. The diagram should highlight the decreased vasoconstriction and aldosterone release as a result of this inhibition. Diagram Description: A diagram illustrating the mechanism of action of beta-blockers. The diagram should visually demonstrate the interaction of beta-blockers with beta-adrenergic receptors in the heart and blood vessels. It should illustrate the resultant decrease in heart rate and contractility, and the potential for vasodilation.
Diagram Description: A diagram illustrating the mechanism of action of beta-blockers. The diagram should visually demonstrate the interaction of beta-blockers with beta-adrenergic receptors in the heart and blood vessels. It should illustrate the resultant decrease in heart rate and contractility, and the potential for vasodilation.