Tortuous colon and IBS: a complex interplay of digestive distress. This condition, characterized by a twisting or abnormal colon shape, often coexists with Irritable Bowel Syndrome (IBS). Understanding the symptoms, diagnostics, and management strategies is crucial for navigating this health challenge. Let’s explore the nuances of this condition together.
This comprehensive guide delves into the specifics of a tortuous colon, focusing on its connection to IBS. We’ll cover everything from defining the condition to exploring various treatment options and the importance of patient support. Get ready to gain a deeper understanding of this intricate digestive issue.
Introduction to Tortuous Colon and IBS
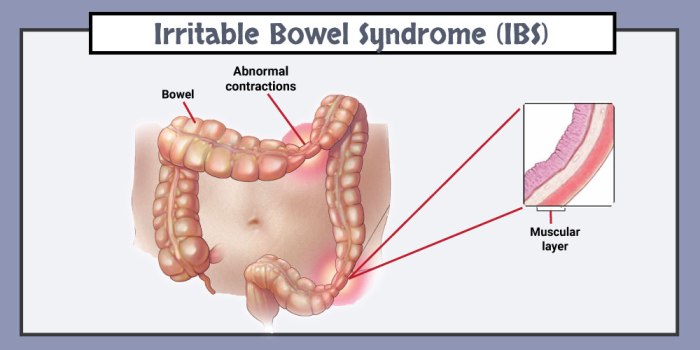
A tortuous colon, sometimes called a sigmoid colon, is a condition characterized by an abnormally coiled or twisted shape of the colon, specifically the sigmoid colon. This anatomical anomaly can lead to various digestive issues, potentially impacting the efficient movement of stool through the large intestine. The sigmoid colon, located at the juncture of the descending colon and the rectum, is particularly susceptible to this twisting or looping.
The presence of a tortuous colon is often detected incidentally during imaging procedures, such as colonoscopies or CT scans, or it may be a finding related to a family history of similar conditions.The relationship between a tortuous colon and Irritable Bowel Syndrome (IBS) is complex. While a tortuous colon isn’t a direct cause of IBS, it can exacerbate or contribute to symptoms.
The twisting of the colon can disrupt normal bowel motility, leading to constipation, diarrhea, or alternating patterns of both. The presence of a tortuous colon may increase the likelihood of experiencing IBS symptoms. It’s important to note that many individuals with a tortuous colon do not experience any symptoms at all.The prevalence of both tortuous colon and IBS is not definitively established due to varying diagnostic criteria and the often asymptomatic nature of a tortuous colon.
However, both conditions are relatively common, affecting a significant portion of the population. Demographics associated with these conditions are similar to other gastrointestinal disorders, with no specific high-risk groups. The prevalence appears to be somewhat higher in women than in men.Common symptoms associated with both conditions include abdominal pain, bloating, and changes in bowel habits. These symptoms can vary in severity and frequency, impacting daily life.
The overlapping nature of symptoms can sometimes make it challenging to differentiate between the two conditions.
Comparing Symptoms of Tortuous Colon and IBS
The following table Artikels the potential symptoms of a tortuous colon and IBS, highlighting similarities and differences:
| Symptom | Tortuous Colon | IBS |
|---|---|---|
| Abdominal Pain | Often described as cramping or localized pain, sometimes worse after eating. | Varied, including cramping, sharp, or dull pain. Often associated with bowel movements. |
| Bloating | May occur due to slowed transit time and gas accumulation. | A common symptom, often accompanied by distention and discomfort. |
| Constipation | Possible due to slowed movement of stool through the colon. | A key symptom, often alternating with diarrhea. |
| Diarrhea | Less common than constipation, but possible. | Alternating with constipation in many cases. |
| Gas | Can be exacerbated by the twisting of the colon, potentially leading to excessive gas. | Frequently reported due to bowel motility changes. |
| Nausea/Vomiting | Rare, but possible in severe cases. | Possible but less common than other symptoms. |
The table demonstrates that many symptoms overlap between tortuous colon and IBS. A thorough medical evaluation is crucial to accurately diagnose the underlying cause of these symptoms and develop appropriate management strategies. Accurate diagnosis is vital for appropriate treatment.
Diagnostic Methods and Procedures
Unraveling the complexities of a tortuous colon and irritable bowel syndrome (IBS) often hinges on precise diagnostic methods. Accurate identification is crucial for tailoring effective treatment strategies. A thorough understanding of the diagnostic procedures employed is vital for both healthcare professionals and individuals seeking clarity about their health concerns.
Imaging Techniques
Imaging plays a pivotal role in visualizing the colon’s structure and identifying potential abnormalities. X-rays, particularly contrast studies, can reveal the colon’s shape and any significant twists or kinks. Radiopaque contrast material is ingested or administered rectally, allowing for detailed visualization of the colon’s pathway on X-ray images. CT scans provide cross-sectional views, offering more detailed anatomical information and helping to assess the extent of the tortuosity.
For instance, a CT scan might reveal a marked S-shaped or spiral configuration of the colon, characteristic of a tortuous colon. These images can also assist in excluding other conditions with similar symptoms.
Endoscopic Procedures
Endoscopic procedures, like colonoscopy, offer direct visualization of the colon’s lining. A flexible tube with a camera at its end (endoscope) is inserted through the rectum and advanced into the colon. This allows healthcare providers to directly observe the colon’s inner surface, identify any structural abnormalities, and collect tissue samples for further analysis if necessary. A colonoscopy is indispensable for evaluating the presence of inflammation, polyps, or other abnormalities that may co-exist with a tortuous colon.
It also aids in ruling out other potential causes of IBS symptoms.
Patient History and Physical Examination
A comprehensive patient history and physical examination are foundational to the diagnostic process. Gathering detailed information about the patient’s symptoms, including the onset, duration, and characteristics of abdominal pain, bowel habits, and associated symptoms, is crucial. This information, combined with a thorough physical examination, assists in narrowing down potential diagnoses. For example, a patient with a history of abdominal pain that worsens after meals, accompanied by changes in bowel habits, might suggest a possible link to a tortuous colon.
Diagnostic Tests and Expected Outcomes
| Diagnostic Test | Expected Outcome (Tortuous Colon) | Expected Outcome (Other Conditions) |
|---|---|---|
| Plain X-rays (with contrast) | May reveal a tortuous or abnormally shaped colon, with areas of constriction or twisting. | May reveal other bowel obstructions or gas patterns, but not necessarily tortuosity. |
| CT Scan | Provides detailed cross-sectional images, showcasing the colon’s structure, demonstrating the extent and location of the tortuosity. | Can help identify other abdominal abnormalities, such as tumors, or blockages, but not definitively diagnose tortuosity. |
| Colonoscopy | Direct visualization of the colon’s lining, enabling identification of any associated inflammation, lesions, or structural abnormalities, along with assessment of the extent of the tortuosity. | May reveal polyps, inflammation, or other conditions affecting the colon, which can be mistaken for tortuosity. |
| Patient History and Physical Examination | May reveal suggestive symptoms like intermittent abdominal pain, changes in bowel habits, and abdominal tenderness, often correlated with the location of the tortuous section. | May reveal symptoms indicative of other digestive issues, such as appendicitis, diverticulitis, or Crohn’s disease. |
Underlying Mechanisms and Risk Factors
Understanding the causes and contributing factors behind tortuous colon and IBS is crucial for effective diagnosis and management. While the precise mechanisms remain somewhat elusive, various elements play a role in their development. This section delves into potential causes, genetic predispositions, lifestyle influences, and the impact of stress on these conditions.The intricate interplay of genetic predisposition, environmental factors, and lifestyle choices contribute significantly to the manifestation of these disorders.
Research suggests that a combination of factors, rather than a single cause, is often responsible. This complexity underscores the need for a holistic approach to treatment and management.
Potential Causes and Contributing Factors
Tortuous colon, a condition characterized by abnormal twisting or looping of the colon, can stem from various developmental factors, often appearing in infancy or early childhood. The exact cause often remains unknown. However, congenital factors, anomalies in the formation of the colon during fetal development, can contribute to the formation of these twists. Acquired factors, such as adhesions or scar tissue resulting from previous surgeries or infections, can also lead to the development of a tortuous colon later in life.
Genetic Predisposition and Family History
A family history of either tortuous colon or IBS significantly increases an individual’s risk. Genetic factors can influence the structure and function of the gastrointestinal tract, making some individuals more susceptible to these conditions. Studies have identified specific genes associated with increased susceptibility to both conditions, although the precise role of these genes is still being investigated. This hereditary predisposition suggests a genetic component in the development of both disorders.
Impact of Lifestyle Factors
Lifestyle factors, including diet and exercise, play a critical role in the overall health of the gastrointestinal system and can potentially influence the development and severity of symptoms in individuals predisposed to these conditions. A diet high in processed foods, low in fiber, and lacking in essential nutrients may exacerbate existing IBS symptoms. Similarly, a sedentary lifestyle can contribute to poor digestive health.Regular physical activity, on the other hand, can promote healthy digestion and potentially reduce the risk of developing or worsening symptoms.
Dealing with a tortuous colon and IBS can be a real pain, figuratively and sometimes literally! It’s a frustrating journey, but sometimes a little bit of discomfort is nothing compared to a truly awful ingrown toenail. Learning how to remove an ingrown toenail properly can be a game-changer for your foot health, and there are some great resources out there, like this guide on how to remove an ingrown toenail.
Ultimately, though, navigating the complexities of a tortuous colon and IBS requires patience and a good support system. You’re not alone in this, and remember to prioritize your health and well-being.
Maintaining a balanced diet rich in fiber and a regular exercise regimen are important for managing these conditions.
Role of Stress and Emotional Factors
Stress and emotional factors can significantly influence the manifestation of IBS symptoms. The gut-brain axis, the complex communication network between the central nervous system and the gastrointestinal tract, is sensitive to emotional states. Stressful events, anxiety, and depression can trigger or exacerbate IBS symptoms in susceptible individuals. Techniques like mindfulness, yoga, and meditation can help manage stress and its impact on IBS symptoms.
Risk Factors and Potential Impact
| Risk Factor | Potential Impact |
|---|---|
| Family history of tortuous colon or IBS | Increased susceptibility to developing the condition. |
| Congenital anomalies | Abnormal colon formation during fetal development, potentially leading to tortuous colon. |
| Previous abdominal surgeries or infections | Increased risk of adhesions and scar tissue formation, potentially causing tortuous colon. |
| High-fat, low-fiber diet | May worsen existing IBS symptoms. |
| Sedentary lifestyle | Potentially contributes to poor digestive health and exacerbates symptoms. |
| Stress and emotional factors | Can trigger or worsen IBS symptoms. |
Management and Treatment Strategies
Managing tortuous colon and IBS involves a multifaceted approach, focusing on alleviating symptoms, improving quality of life, and preventing complications. This approach often combines lifestyle modifications, medication, and in some cases, surgical intervention. A personalized strategy tailored to individual needs is crucial for optimal outcomes.Effective management strategies require a thorough understanding of the specific presentation of the condition.
The interplay of symptoms, severity, and patient factors dictates the most appropriate course of action. A collaborative effort between patients, gastroenterologists, and other healthcare professionals is essential for successful long-term management.
Dealing with a tortuous colon and IBS can be tough, but recent research offers a glimmer of hope. A new study by Eli Lilly on tirzepatide, a drug that’s showing promise in reducing the risk of diabetes, might offer some interesting possibilities for managing related symptoms. This study suggests that the medication could potentially improve overall metabolic health, which could indirectly benefit those with digestive issues like IBS and a tortuous colon.
Further research is needed, but it’s an exciting development for people navigating these complex conditions.
Dietary Modifications and Lifestyle Changes
Dietary adjustments play a significant role in managing the symptoms of tortuous colon and IBS. These modifications aim to reduce gut irritation and promote regularity. Fiber intake, while beneficial for many, can be problematic for some individuals. The goal is to find a balanced approach that meets individual needs.
Dealing with a tortuous colon and IBS can be tough, but focusing on gut health is key. While I’m no expert on that, learning how to properly care for your ears, like how to get rid of swimmers ear, how to get rid of swimmers ear , might seem unrelated, but maintaining good hygiene and avoiding infections is vital for overall health, which can indirectly affect the digestive system.
Ultimately, prioritizing a healthy lifestyle, including good ear care, can positively impact your overall well-being, especially when navigating issues like a tortuous colon and IBS.
- A gradual increase in fiber intake, monitored for adverse effects, is a key aspect of dietary management. This should be done under the guidance of a registered dietitian.
- Identifying and avoiding trigger foods, such as certain types of fatty foods, caffeine, alcohol, and high-FODMAP foods, is crucial for symptom reduction.
- Maintaining a consistent meal schedule and avoiding large meals can help regulate bowel movements and reduce bloating.
- Regular physical activity can promote healthy digestion and overall well-being.
Medications and Therapies
Pharmacological interventions are frequently employed to manage symptoms and underlying mechanisms. The specific medications and therapies used vary depending on the individual’s specific needs and the severity of their condition.
- Anti-spasmodics are often prescribed to relieve abdominal cramps and pain. Examples include dicyclomine and hyoscyamine.
- Laxatives may be used to promote bowel movements, especially in cases of constipation. The type of laxative prescribed will depend on the specific needs of the patient.
- Anti-inflammatory medications can help reduce inflammation in the colon, which can be a contributing factor to symptoms.
- Antidepressants, such as tricyclic antidepressants, may be prescribed to help manage symptoms of anxiety or depression, which can often coexist with IBS and exacerbate symptoms.
Surgical Interventions, Tortuous colon and ibs
Surgical intervention is reserved for cases of severe or intractable tortuous colon where other treatments have failed. Surgical procedures aim to correct the anatomical abnormality, relieve obstruction, and improve bowel function.
- Surgical correction of the tortuous segment of the colon is performed to restore normal colonic motility and alleviate the obstruction.
- Surgical interventions are typically considered only after conservative measures have been exhausted and when the condition poses a significant risk to the patient’s health.
Treatment Options and Effectiveness
| Treatment Option | Description | Effectiveness |
|---|---|---|
| Dietary Modifications | Adjusting diet to include fiber, avoiding trigger foods, and maintaining a regular meal schedule. | Generally effective in managing symptoms, particularly in conjunction with other therapies. |
| Medications (Anti-spasmodics, Laxatives) | Medication to reduce pain, spasms, and improve bowel movements. | Effective in reducing symptoms for many patients, but may not be suitable for all. |
| Surgical Intervention | Surgical correction of the tortuous colon segment. | Highly effective in cases of severe obstruction and failure of other treatments, restoring normal bowel function. |
Complications and Prognosis
Navigating the complexities of a tortuous colon and IBS often involves understanding the potential long-term consequences and the impact on quality of life. While these conditions can be managed effectively, it’s crucial to be aware of the possible complications and the importance of proactive monitoring. This section delves into the potential problems, prognosis, and the need for ongoing care.
Potential Complications
Understanding the potential complications associated with a tortuous colon and IBS is essential for proactive management. These conditions, while often manageable, can lead to a range of issues if not properly addressed. The severity and frequency of these complications can vary significantly depending on the individual and the specific nature of their condition.
- Obstruction: A tortuous colon, characterized by abnormal bends and twists, can sometimes lead to a complete or partial blockage of the bowel. This can cause severe pain, nausea, vomiting, and abdominal distension. If left untreated, it can necessitate surgical intervention.
- Inflammatory Bowel Disease (IBD): Individuals with a tortuous colon and IBS have an increased risk of developing inflammatory bowel diseases, such as Crohn’s disease or ulcerative colitis. These conditions are characterized by chronic inflammation of the digestive tract and can lead to significant discomfort and complications.
- Hemorrhage: The increased pressure and strain on the colon due to tortuosity can sometimes lead to bleeding. This can manifest as rectal bleeding, blood in the stool, or even more severe internal bleeding requiring medical attention.
- Nutritional Deficiencies: Persistent digestive issues can impact nutrient absorption. This can lead to deficiencies in essential vitamins and minerals, which may require supplementation or dietary adjustments.
- Chronic Pain and Discomfort: The underlying conditions often result in chronic pain and discomfort, significantly impacting quality of life. Managing this pain effectively is crucial for overall well-being.
Long-Term Prognosis and Quality of Life
The long-term prognosis for individuals with a tortuous colon and IBS varies depending on several factors. While the condition can be managed effectively, the impact on quality of life can be significant, affecting daily activities, social interactions, and emotional well-being.
- Variability in Severity: The severity of symptoms and the frequency of flare-ups can vary greatly from person to person. Some individuals may experience only mild discomfort, while others may have more severe and debilitating symptoms that significantly impact their daily lives.
- Impact on Daily Life: The unpredictable nature of IBS symptoms can lead to missed work or school, reduced social activities, and a general feeling of anxiety and frustration. Managing these disruptions is an ongoing challenge.
- Psychological Impact: Living with chronic pain and digestive issues can take a toll on mental health. Anxiety, depression, and stress are common concerns for those affected by these conditions.
- Potential for Improvement: Many individuals with a tortuous colon and IBS can lead fulfilling lives with proper management and support. Lifestyle modifications, medications, and therapies can often significantly improve symptom control and quality of life.
Potential for Developing Other Related Conditions
The presence of a tortuous colon and IBS might increase the likelihood of developing other related conditions. This underscores the importance of proactive monitoring and management.
- Anal Fissures: Increased pressure on the colon can lead to anal fissures, small tears in the lining of the anus.
- Fistulas: In some cases, inflammation and complications can lead to the formation of fistulas, abnormal connections between different parts of the body.
Importance of Regular Follow-up and Monitoring
Regular follow-up visits and monitoring are crucial for effective management and early detection of potential complications. This proactive approach allows for prompt intervention and helps maintain a good quality of life.
Potential Complications Summary Table
| Potential Complication | Likelihood |
|---|---|
| Obstruction | Moderate |
| Inflammatory Bowel Disease (IBD) | Increased |
| Hemorrhage | Low to Moderate |
| Nutritional Deficiencies | Moderate |
| Chronic Pain and Discomfort | High |
| Anal Fissures | Moderate |
| Fistulas | Low |
Patient Experiences and Support: Tortuous Colon And Ibs
Living with a tortuous colon and IBS can be incredibly challenging. Beyond the physical discomfort, the unpredictable nature of these conditions often impacts daily life, relationships, and mental well-being. Understanding the experiences of others and developing effective coping mechanisms are crucial for navigating this journey. This section delves into the realities of living with these conditions, emphasizing the importance of support and empowerment.
Real-Life Experiences
Many individuals with tortuous colon and IBS face a spectrum of symptoms, ranging from mild discomfort to debilitating pain. A common thread is the unpredictable nature of the condition. One patient might experience severe cramping and bloating after eating certain foods, while another might struggle with chronic constipation and significant discomfort. The impact extends beyond the physical; the anxiety and fear surrounding the unpredictability of symptoms can lead to significant stress and emotional distress.
For example, social gatherings or travel can become sources of anxiety due to the potential for flare-ups. These real-life experiences highlight the importance of tailored support and management strategies.
Emotional Support and Coping Mechanisms
Managing the emotional toll of a tortuous colon and IBS is just as important as managing the physical symptoms. Chronic pain and discomfort can lead to feelings of frustration, anger, and even depression. Developing healthy coping mechanisms is vital for maintaining overall well-being. These strategies can include stress-reduction techniques like meditation, yoga, or deep breathing exercises, as well as maintaining a healthy lifestyle through regular exercise and a balanced diet.
Seeking professional counseling or therapy can provide additional support and guidance in navigating the emotional aspects of the condition.
Support Groups and Online Communities
Connecting with others who understand the unique challenges of living with a tortuous colon and IBS can be incredibly beneficial. Support groups, both in-person and online, offer a safe space for sharing experiences, exchanging advice, and finding encouragement. Online communities provide similar benefits, allowing individuals to connect with others from anywhere in the world, fostering a sense of belonging and reducing feelings of isolation.
The shared experiences and support within these groups can be a powerful resource for coping with the condition.
Patient Education and Empowerment
Empowering patients with knowledge about their condition is critical for effective self-management. Understanding the triggers, symptoms, and available treatment options allows patients to actively participate in their care. This involves educating patients on dietary modifications, stress management techniques, and the importance of regular medical check-ups. Patient education fosters a sense of control and empowers individuals to take an active role in managing their health.
This knowledge, coupled with support from healthcare professionals and fellow patients, empowers them to navigate their condition more effectively.
Common Patient Concerns and Potential Solutions
| Common Patient Concerns | Potential Solutions |
|---|---|
| Unpredictable symptoms and their impact on daily life | Developing a personalized symptom diary, identifying triggers, and exploring strategies to manage symptoms proactively. This includes dietary modifications, stress-reduction techniques, and exploring alternative therapies. |
| Anxiety and fear surrounding potential flare-ups | Cognitive behavioral therapy (CBT) to challenge negative thought patterns, relaxation techniques, and support groups or online communities to share experiences and reduce isolation. |
| Difficulty maintaining a social life due to symptoms | Open communication with friends and family about the condition, planning social activities with awareness of potential triggers, and utilizing support systems. |
| Limited access to specialized care or information | Seeking referrals to gastroenterologists or specialists experienced in managing tortuous colon and IBS, and utilizing online resources, patient support groups, and educational materials. |
| Feeling isolated or alone in their struggles | Joining support groups, participating in online communities, connecting with healthcare providers, and educating oneself about the condition to better understand it. |
Illustrative Case Studies
Understanding tortuous colon and IBS requires delving into real-world examples. Case studies offer valuable insights into the diagnostic journey, treatment approaches, and long-term outcomes. These accounts highlight the diverse presentations and complexities of these conditions, offering a deeper understanding of the human experience.
Case Study: A Young Adult with Chronic Abdominal Pain
This case study involves a 25-year-old female presenting with chronic abdominal pain, cramping, and altered bowel habits for the past two years. The pain was described as severe and intermittent, often localized to the lower left quadrant. The patient also reported bloating, nausea, and fatigue.
Diagnostic Process
The diagnostic process began with a thorough medical history and physical examination. Initial investigations included blood tests, stool analysis, and abdominal X-rays. These initial tests revealed no significant abnormalities. Subsequently, a CT scan of the abdomen and pelvis was performed, which revealed a segment of tortuous colon. Further, a colonoscopy confirmed the presence of the tortuous segment, as well as mild inflammation and mucosal irregularities.
The findings strongly suggested the diagnosis of a tortuous colon, contributing to the patient’s IBS symptoms.
Treatment and Outcome
The patient was initially managed with dietary modifications, including a high-fiber diet and avoidance of trigger foods. Medications such as anti-spasmodics and laxatives were also prescribed to manage pain and improve bowel regularity. Despite these interventions, the patient’s symptoms persisted. Therefore, a surgical intervention, namely a colon resection, was ultimately recommended to address the tortuous segment of the colon.
The surgical procedure was successful, and the patient experienced a significant improvement in her symptoms. She reported a reduction in abdominal pain, improved bowel habits, and an overall enhanced quality of life.
Factors Contributing to Development
The precise etiology of tortuous colon is often unknown. However, potential factors that might have contributed to the development of this condition in the case study could include a family history of bowel abnormalities or conditions. Genetic predisposition or other underlying medical conditions may also have played a role. Furthermore, lifestyle factors such as poor diet and lack of physical activity may have contributed to the condition’s progression.
Long-Term Implications
The long-term implications for the patient included the need for regular follow-up appointments with her gastroenterologist to monitor for any recurrence of symptoms or complications. The patient was educated on the importance of adhering to a healthy lifestyle, including a balanced diet, regular exercise, and stress management techniques. Furthermore, she was advised on strategies to prevent future exacerbations of her symptoms.
The patient was also provided with resources for support groups to connect with others experiencing similar conditions.
Summary Table
| Category | Details |
|---|---|
| Patient Age | 25 |
| Presenting Symptoms | Chronic abdominal pain, cramping, altered bowel habits |
| Diagnostic Tests | Blood tests, stool analysis, abdominal X-rays, CT scan, colonoscopy |
| Diagnosis | Tortuous colon, contributing to IBS |
| Treatment | Dietary modifications, medications, surgical resection |
| Outcome | Significant symptom improvement, enhanced quality of life |
| Long-term Implications | Regular follow-up, lifestyle modifications, support groups |
Dietary Considerations
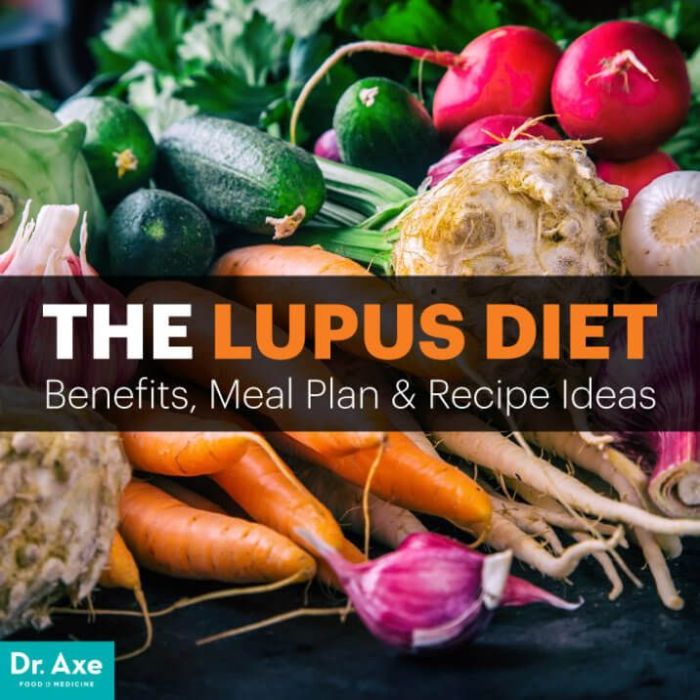
Navigating a tortuous colon and IBS often feels like a culinary minefield. Understanding which foods are your allies and which are your enemies can significantly impact your overall well-being and symptom management. This section delves into crucial dietary strategies tailored to minimize discomfort and maximize digestive health.
Sample Meal Plan
A sample meal plan for managing tortuous colon and IBS is highly individualized. This example demonstrates a balanced approach, but consulting with a registered dietitian or gastroenterologist is essential for personalized recommendations.
- Breakfast (Example): Oatmeal with berries and a sprinkle of nuts, a small glass of low-lactose milk (if tolerated), and a slice of whole-wheat toast. This provides complex carbohydrates, fiber, and essential nutrients.
- Lunch (Example): Grilled chicken salad with mixed greens, avocado, and a light vinaigrette dressing. A side of brown rice or quinoa can further boost fiber intake.
- Dinner (Example): Baked fish with roasted vegetables (broccoli, carrots, sweet potatoes) and a small portion of brown rice. Lean protein and a variety of colorful vegetables offer essential nutrients.
- Snacks (Examples): Plain yogurt (low-lactose if needed), a handful of almonds, or a piece of fruit like a small apple or banana. These provide sustained energy and help regulate blood sugar levels.
Importance of Fiber
Dietary fiber is crucial for healthy digestion in individuals with tortuous colon and IBS. It promotes regular bowel movements and helps maintain a healthy gut microbiome. Soluble fiber, like that found in oats and beans, dissolves in water, forming a gel-like substance that slows down digestion and helps regulate blood sugar. Insoluble fiber, found in whole grains and vegetables, adds bulk to stool, making it easier to pass.
Foods to Avoid
Identifying and avoiding trigger foods is a significant aspect of managing IBS and tortuous colon. Individual sensitivities vary greatly.
- High-Fat Foods: Foods high in fat, such as fried foods, fatty meats, and processed snacks, can exacerbate symptoms. Fat can often slow down digestion and cause bloating or cramping.
- Processed Foods: Processed foods often contain additives and preservatives that can irritate the digestive system. These can include packaged snacks, fast food, and highly processed meats.
- Spicy Foods: Spicy foods can trigger gastrointestinal distress in some individuals, leading to increased inflammation and discomfort.
- Caffeine and Alcohol: Caffeine and alcohol can have a stimulatory effect on the digestive system, potentially leading to diarrhea or constipation in some individuals.
- High-FODMAP Foods: Foods high in FODMAPs (fermentable oligosaccharides, disaccharides, monosaccharides, and polyols) can trigger symptoms in individuals with IBS. These include wheat, dairy, beans, and certain fruits and vegetables. Consult with a dietitian to create a personalized low-FODMAP diet if appropriate.
Dietary Approaches
Various dietary approaches can be beneficial for managing tortuous colon and IBS.
- Low-FODMAP Diet: This diet restricts foods containing fermentable carbohydrates that can trigger IBS symptoms. It’s crucial to work with a registered dietitian to implement this diet effectively, as improper restriction can lead to nutritional deficiencies.
- High-Fiber Diet: Increasing dietary fiber can promote regular bowel movements and potentially reduce IBS symptoms. It’s essential to increase fiber intake gradually to avoid gas and bloating.
- Anti-inflammatory Diet: Reducing inflammation in the gut can help manage symptoms. This approach focuses on foods rich in antioxidants and anti-inflammatory compounds. It often involves a diet rich in fruits, vegetables, and whole grains.
High-Fiber Foods
Fiber-rich foods are essential for digestive health.
| Food | Fiber Content (approximate) | Benefits |
|---|---|---|
| Oatmeal | 5-8g per serving | Promotes regularity, slows digestion |
| Beans (kidney, black, pinto) | 7-10g per cup | Excellent source of protein and fiber, promotes regularity |
| Broccoli | 5g per serving | Rich in vitamins, minerals, and fiber |
| Spinach | 2g per serving | Rich in vitamins, minerals, and fiber |
| Apples | 4g per medium apple | Rich in fiber and antioxidants |
Final Summary
In conclusion, navigating tortuous colon and IBS requires a multifaceted approach. From accurate diagnosis and personalized treatment plans to the crucial role of patient support and dietary adjustments, understanding the complexities of this condition is paramount. By exploring the various aspects discussed, readers can better understand the challenges and possible solutions for managing this condition. Remember, proactive management and open communication with healthcare professionals are key.