The relationship between PCOS and inflammation is a crucial area of study. This post explores the intricate connection between Polycystic Ovary Syndrome (PCOS) and inflammation, delving into various aspects, from the underlying mechanisms to practical management strategies. We’ll examine different types of inflammation, their impact on PCOS symptoms, and explore dietary and lifestyle interventions, alongside potential treatments and diagnostic methods.
This comprehensive look aims to provide a clear understanding of this important relationship.
PCOS, a common hormonal disorder affecting women of reproductive age, often presents with a complex interplay of symptoms, many linked to underlying inflammation. This inflammatory response can manifest in various ways, impacting everything from insulin resistance and acne to weight gain and overall well-being. Understanding these connections is key to developing effective management strategies and improving the lives of those affected by PCOS.
Understanding PCOS and Inflammation
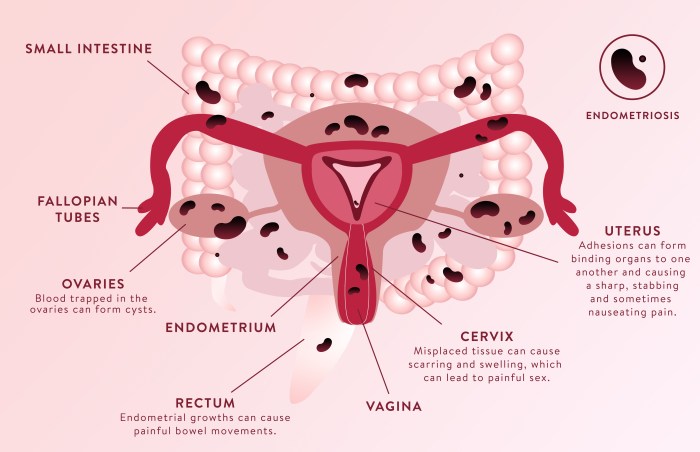
Polycystic ovary syndrome (PCOS) is a common hormonal disorder affecting women of reproductive age. Characterized by irregular periods, excess androgens (male hormones), and the presence of multiple small cysts on the ovaries, PCOS significantly impacts a woman’s reproductive health and overall well-being. Beyond the reproductive symptoms, PCOS is often linked to metabolic disturbances, including insulin resistance and increased risk of type 2 diabetes.
One crucial aspect of PCOS is the presence of chronic low-grade inflammation. This inflammation plays a complex role in the development and progression of PCOS symptoms.Inflammation, a natural bodily response to injury or infection, involves a cascade of cellular and molecular events. In PCOS, this inflammatory response appears to be heightened and sustained, even in the absence of overt infection or injury.
This persistent low-grade inflammation may contribute to the development of other PCOS-related complications. The mechanisms linking inflammation and PCOS are multifaceted and not fully understood, but involve several potential pathways. These pathways include dysregulation of the immune system, oxidative stress, and the effects of insulin resistance.
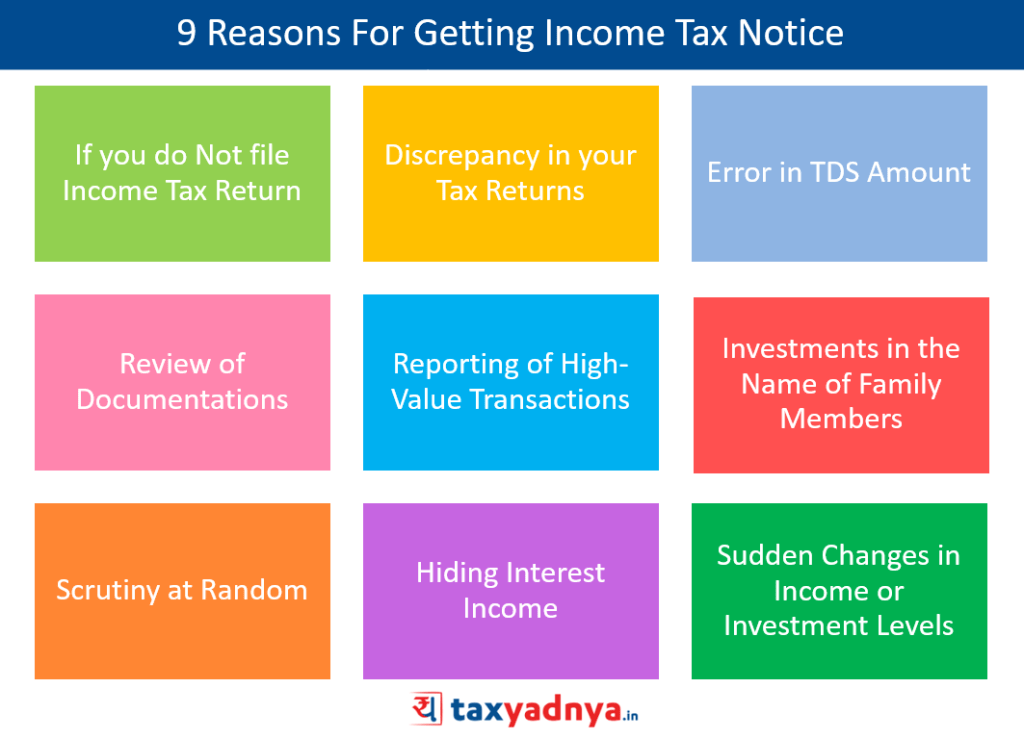
Inflammation Markers Associated with PCOS
Several inflammatory markers have been consistently associated with PCOS. These markers reflect the presence and intensity of the inflammatory process. Understanding these markers is vital for diagnosis and management of PCOS.
Potential Mechanisms Linking PCOS and Inflammation
Multiple factors may contribute to the inflammatory state observed in PCOS. One potential mechanism involves the dysregulation of the immune system. In PCOS, immune cells may be activated and produce inflammatory mediators at higher levels than in healthy individuals. This can lead to a chronic inflammatory response. Oxidative stress, a condition characterized by an imbalance between the production of reactive oxygen species and the body’s ability to neutralize them, is another possible contributing factor.
This imbalance can further exacerbate the inflammatory state. Finally, insulin resistance, a common feature of PCOS, is strongly linked to inflammation. High levels of insulin can stimulate the production of inflammatory cytokines.
So, I’ve been researching PCOS and inflammation lately, and it’s fascinating how interconnected everything seems. One aspect that’s caught my eye is the potential link between chronic inflammation and leg shaking tremor types, causes, and more, as explored in detail on this helpful resource: leg shaking tremor types causes and more. Could this be another way inflammation manifests in the body?
Further research suggests a potential connection between these symptoms and the underlying inflammatory processes associated with PCOS. It’s definitely a complex area, but one worth investigating!
Table of Inflammation Markers in PCOS
| Inflammation Marker | Possible Role in PCOS | Measurement Method |
|---|---|---|
| C-reactive protein (CRP) | A marker of systemic inflammation, often elevated in PCOS. Elevated CRP levels may contribute to insulin resistance and cardiovascular risk. | Blood test |
| Interleukin-6 (IL-6) | A cytokine involved in inflammation and immune response. Elevated levels in PCOS may contribute to insulin resistance and metabolic dysfunction. | Blood test |
| Tumor Necrosis Factor-alpha (TNF-α) | A potent inflammatory cytokine, implicated in the pathogenesis of PCOS-related complications. Elevated levels might contribute to insulin resistance and ovarian dysfunction. | Blood test |
| Adiponectin | An adipokine with anti-inflammatory properties. Reduced levels are associated with inflammation and insulin resistance in PCOS. | Blood test |
Types of Inflammation in PCOS

Inflammation is a crucial aspect of PCOS, often playing a significant role in the development and progression of the condition’s symptoms. Understanding the different types of inflammation and their characteristics is vital for effective management and treatment strategies. Chronic inflammation, a persistent low-grade state, is frequently observed in PCOS, and its effects can be far-reaching, impacting various bodily functions and exacerbating existing health concerns.Inflammation, a complex biological response to cellular injury or infection, can manifest in diverse ways, ranging from acute, short-term episodes to chronic, long-term conditions.
The types of inflammation encountered in PCOS patients are crucial to understanding the underlying mechanisms and developing personalized treatment plans.
Chronic Low-Grade Inflammation
Chronic low-grade inflammation is a hallmark of PCOS. This persistent, mild inflammatory response is characterized by a slow and gradual increase in inflammatory markers, such as C-reactive protein (CRP) and interleukin-6 (IL-6). It’s often subtle and may not present with obvious symptoms, making it challenging to detect and manage. This type of inflammation is closely linked to insulin resistance, a common feature in PCOS, contributing to the development of metabolic dysfunction.
The body’s constant state of low-level inflammation can lead to a cascade of effects, including oxidative stress and cellular damage.
Acute Inflammation
Acute inflammation, a rapid response to injury or infection, is a temporary, localized inflammatory reaction. It’s characterized by redness, swelling, heat, pain, and loss of function in the affected area. In PCOS, acute inflammation might be triggered by an infection or a sudden hormonal shift. While acute inflammation is a natural defense mechanism, persistent or recurring episodes can contribute to chronic inflammation.
For example, an ovarian cyst rupturing might trigger an acute inflammatory response.
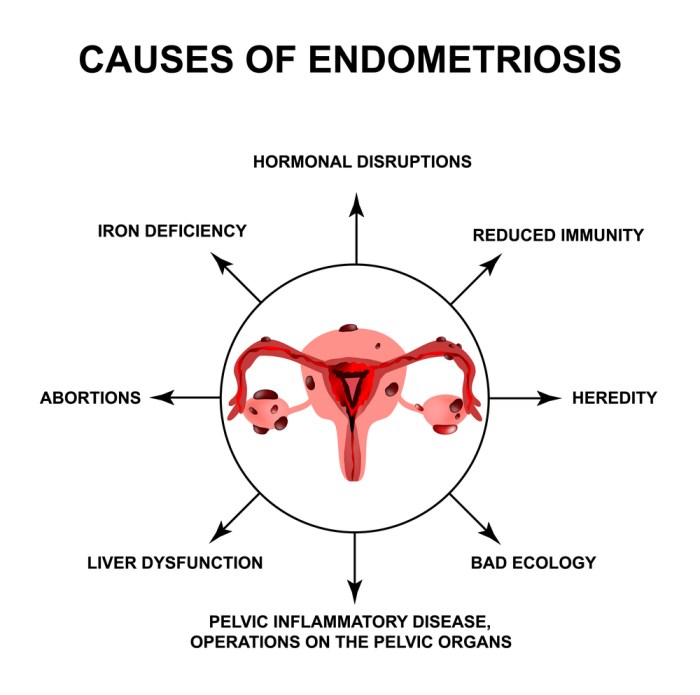
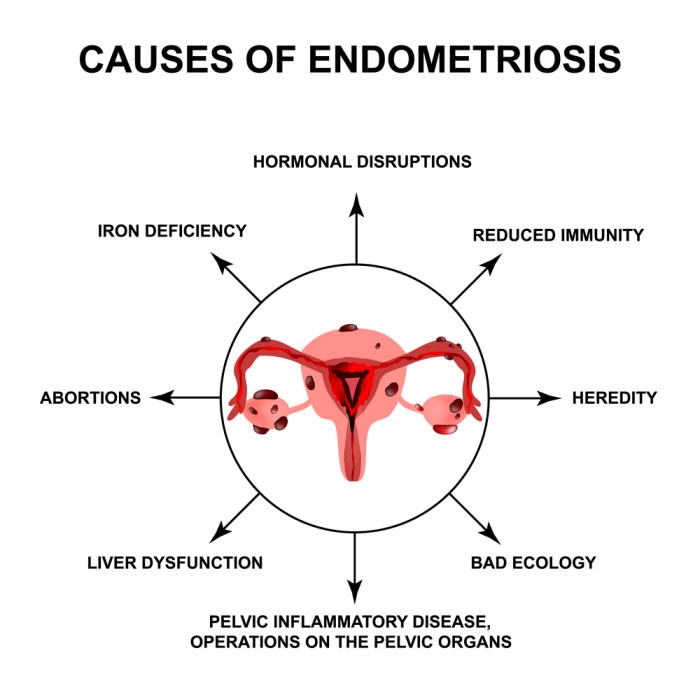
Potential Triggers of Inflammation in PCOS
Various factors can trigger inflammation in PCOS. Insulin resistance, a common feature of PCOS, is a key contributor to chronic low-grade inflammation. Insulin resistance leads to elevated insulin levels, which in turn stimulate inflammatory pathways. Additionally, hormonal imbalances, including high levels of androgens and altered estrogen levels, can also contribute to inflammation. Furthermore, obesity and a sedentary lifestyle have been associated with increased inflammation in PCOS patients.
Oxidative stress, caused by an imbalance between free radicals and antioxidants, also plays a significant role.
Summary Table
| Type of Inflammation | Characteristics | Potential Causes in PCOS |
|---|---|---|
| Chronic Low-Grade Inflammation | Persistent, mild inflammatory response; elevated inflammatory markers (e.g., CRP, IL-6); often subtle symptoms; linked to insulin resistance. | Insulin resistance, hormonal imbalances (high androgens, altered estrogen), obesity, sedentary lifestyle, oxidative stress. |
| Acute Inflammation | Rapid, localized response to injury or infection; characterized by redness, swelling, heat, pain; temporary. | Ovarian cyst rupture, infection, sudden hormonal shifts. |
Impact of Inflammation on PCOS Symptoms
Inflammation plays a significant role in the development and progression of PCOS symptoms. It’s not just an irritating side effect, but a key driver of the complex hormonal imbalances and metabolic disturbances characteristic of PCOS. Understanding how inflammation fuels these symptoms is crucial for effective management and treatment strategies.Inflammation in PCOS isn’t simply a localized response. It’s a systemic process, affecting various organs and tissues throughout the body.
This widespread inflammation creates a cascade of effects that contribute to the diverse range of symptoms experienced by women with PCOS. The mechanisms through which inflammation impacts these symptoms are multifaceted and not fully understood, but research is uncovering key pathways.
Inflammation and Insulin Resistance
Chronic inflammation can impair insulin sensitivity, leading to insulin resistance. This means that the body’s cells become less responsive to insulin, a hormone responsible for regulating blood sugar levels. As a result, the pancreas produces more insulin to compensate, which can further exacerbate the inflammatory response. This vicious cycle can contribute to elevated blood sugar levels and an increased risk of type 2 diabetes.
Elevated inflammatory markers like TNF-α and IL-6 are frequently linked to insulin resistance in women with PCOS.
Inflammation and Acne
Inflammation is directly implicated in the development of acne in PCOS. Increased androgen levels, a hallmark of PCOS, combined with the inflammatory response, can trigger sebaceous gland activity. This leads to excess oil production and clogged pores, creating an environment conducive to acne formation. Studies show a correlation between elevated inflammatory markers and acne severity in women with PCOS.
Inflammation and Weight Gain
Inflammation can contribute to weight gain in PCOS by disrupting the body’s metabolism. Chronic inflammation can interfere with the body’s ability to properly utilize energy, leading to an increase in fat storage. Moreover, the inflammatory process can impact appetite regulation, potentially leading to increased food intake and further weight gain. It’s also important to note that the inflammatory response can negatively affect fat distribution, potentially leading to central obesity.
Inflammation and Other Symptoms
Inflammation is also suspected to play a role in other PCOS symptoms, such as fatigue, hair loss, and sleep disturbances. While the exact mechanisms are still being researched, the chronic inflammatory state can lead to systemic issues that affect multiple bodily functions.
Correlation between Inflammation Markers and PCOS Symptoms
| Inflammation Marker | Potential Impact on PCOS Symptoms |
|---|---|
| TNF-α (Tumor Necrosis Factor-alpha) | Insulin resistance, acne, weight gain, and potentially other symptoms |
| IL-6 (Interleukin-6) | Insulin resistance, acne, weight gain, and potentially other symptoms |
| CRP (C-reactive protein) | Systemic inflammation, potentially impacting various symptoms like insulin resistance and weight gain |
Note: This table provides a simplified overview. The exact correlation between specific inflammation markers and individual symptoms can vary among women with PCOS.
Role of Diet and Lifestyle in Managing Inflammation in PCOS
Inflammation plays a crucial role in the development and progression of PCOS symptoms. Fortunately, dietary choices and lifestyle modifications can significantly impact inflammation levels, offering a valuable avenue for managing PCOS. Understanding how diet and lifestyle choices interact with inflammation is key to creating a personalized approach to PCOS management.Dietary choices have a profound impact on inflammation levels in individuals with PCOS.
Foods high in processed sugars, unhealthy fats, and refined carbohydrates tend to promote inflammation. Conversely, a diet rich in anti-inflammatory foods can help reduce inflammation and improve overall well-being. By making conscious food choices, individuals with PCOS can actively manage their inflammation levels.
Impact of Dietary Choices on Inflammation in PCOS
A diet rich in processed foods, saturated fats, and refined carbohydrates often leads to higher inflammation levels. These foods can increase the production of inflammatory markers in the body. Conversely, a diet emphasizing whole, unprocessed foods, healthy fats, and complex carbohydrates can help reduce inflammation. The type and quality of the foods consumed significantly influence the inflammatory response.
Anti-Inflammatory Foods and Dietary Patterns for PCOS
A diet rich in fruits, vegetables, and whole grains is highly beneficial for managing inflammation in PCOS. These foods provide essential vitamins, minerals, and antioxidants, all of which contribute to a reduced inflammatory response. Lean proteins, such as fish and poultry, are also beneficial, providing essential nutrients without excessive saturated fat. Furthermore, incorporating healthy fats, such as those found in avocados, nuts, and seeds, can support overall health and reduce inflammation.
The Mediterranean diet, with its emphasis on fruits, vegetables, whole grains, and healthy fats, is often recommended for its anti-inflammatory properties.
Managing Inflammation Through Lifestyle Modifications
Regular exercise is a crucial lifestyle modification for managing inflammation in PCOS. Physical activity helps to improve insulin sensitivity, reduce body weight, and lower inflammatory markers. Aiming for at least 150 minutes of moderate-intensity aerobic exercise per week, along with strength training exercises two times a week, can significantly contribute to reducing inflammation and improving overall health. Adequate sleep is also essential, as sleep deprivation can increase inflammation.
Table Summarizing Anti-Inflammatory Dietary Strategies
| Dietary Strategy | Potential Impact on PCOS Symptoms |
|---|---|
| Increased intake of fruits and vegetables | Reduced inflammation, improved nutrient intake, and potential weight management |
| Emphasis on whole grains | Improved insulin sensitivity, sustained energy levels, and potential weight management |
| Inclusion of lean proteins (fish, poultry) | Provides essential nutrients without excessive saturated fat, promoting satiety, and supporting muscle mass |
| Healthy fats (avocados, nuts, seeds) | Support overall health, promote satiety, and reduce inflammation |
| Reduced intake of processed foods, refined sugars, and unhealthy fats | Reduction in inflammatory triggers, improved blood sugar control, and weight management |
| Regular exercise (aerobic and strength training) | Improved insulin sensitivity, reduced body weight, and lower inflammatory markers |
| Adequate sleep | Improved hormone regulation, reduced stress, and decreased inflammation |
Potential Treatments Targeting Inflammation in PCOS: The Relationship Between Pcos And Inflammation
Inflammation plays a crucial role in the development and progression of PCOS symptoms. Therefore, targeting and managing inflammation is a key aspect of PCOS management. Effective treatment strategies aim to reduce inflammation, which can positively impact various symptoms, including insulin resistance, hormonal imbalances, and metabolic issues. This approach also aims to improve overall health and well-being.Several treatment approaches have shown promise in mitigating inflammation associated with PCOS.
These approaches address the underlying causes of inflammation and work to alleviate its negative effects on the body. The efficacy of these treatments varies among individuals, and the best course of action should be determined in consultation with a healthcare professional.
Medications with Anti-inflammatory Properties
Several medications commonly used to treat PCOS symptoms can also exhibit anti-inflammatory effects. These medications often address various aspects of the condition, including hormonal imbalances, insulin resistance, and the inflammatory response itself.
Understanding the link between PCOS and inflammation is crucial. High levels of inflammation can significantly impact various aspects of health, and it’s often linked to PCOS symptoms. This inflammation can sometimes necessitate surgical procedures, where the methods of closing incisions, like sutures, staples, or glue ( incision closed sutures staples glue ), become important factors to consider. Ultimately, managing inflammation is key to mitigating the long-term effects of PCOS.
- Metformin: This medication is frequently prescribed for PCOS due to its ability to improve insulin sensitivity. Improved insulin sensitivity can contribute to reduced inflammation throughout the body. Metformin’s anti-inflammatory action is believed to stem from its ability to regulate blood glucose levels and improve mitochondrial function. This, in turn, reduces oxidative stress, a key contributor to inflammation.
- Anti-androgens: These medications, like spironolactone and others, help regulate androgens, which can be elevated in PCOS. Elevated androgens are associated with inflammation. By reducing androgen levels, anti-androgens can help reduce the inflammatory response. It is important to remember that these medications address the symptoms and potential underlying causes of inflammation.
- NSAIDs (Nonsteroidal Anti-inflammatory Drugs): While not specifically designed for PCOS, NSAIDs like ibuprofen or naproxen can provide temporary relief from inflammatory symptoms. Their use should be carefully considered and monitored due to potential side effects and should not be a primary treatment approach.
Lifestyle Interventions
Lifestyle interventions play a vital role in managing inflammation in PCOS. These interventions address the root causes of inflammation and promote overall well-being.
Inflammation plays a significant role in PCOS, often contributing to symptoms like fatigue and acne. Interestingly, some research suggests that certain natural remedies, like Lion’s Mane mushrooms, might help manage ADHD symptoms. Lions mane for adhd could potentially be a helpful tool for managing some of the underlying inflammation and cognitive function challenges. However, more research is needed to fully understand how this relates to the root causes of PCOS symptoms.
The connection between inflammation and PCOS remains a key area of investigation.
- Dietary Changes: A diet rich in anti-inflammatory foods, such as fruits, vegetables, and healthy fats, can contribute to reducing inflammation. A balanced diet can help maintain healthy weight, reduce insulin resistance, and regulate blood sugar levels. This approach aims to create a more stable and healthier environment for the body, reducing inflammation.
- Regular Exercise: Physical activity is crucial for managing inflammation and improving overall health. Exercise helps regulate blood sugar, improve insulin sensitivity, and promote overall well-being. These effects contribute to a decrease in inflammation.
- Stress Management Techniques: Chronic stress can exacerbate inflammation. Practices like yoga, meditation, and deep breathing exercises can help manage stress and reduce inflammation.
Potential Therapies
Some therapies have shown promise in reducing inflammation associated with PCOS. These approaches often target specific inflammatory pathways or promote overall well-being.
- Nutritional Supplements: Certain supplements, such as vitamin D, omega-3 fatty acids, and curcumin, have demonstrated anti-inflammatory properties. These supplements can be beneficial in supporting overall health and reducing inflammation. It is essential to consult with a healthcare professional before incorporating any new supplements into your routine.
Treatment Approaches Table
| Treatment Approach | Mechanism of Action | Potential Benefits for Managing Inflammation in PCOS |
|---|---|---|
| Metformin | Improves insulin sensitivity, regulates blood glucose, and potentially reduces oxidative stress. | Reduces inflammation associated with insulin resistance and improves metabolic function. |
| Anti-androgens | Regulates androgen levels, which are often elevated in PCOS and associated with inflammation. | Reduces inflammation related to androgen excess, improving hormonal balance. |
| NSAIDs | Provide temporary relief from inflammatory symptoms. | Can offer temporary relief from pain and inflammation, but should not be a primary treatment approach. |
| Dietary Changes | Provide anti-inflammatory foods and nutrients. | Supports overall health and reduces inflammation by regulating blood sugar and maintaining a healthy weight. |
| Regular Exercise | Improves insulin sensitivity, regulates blood sugar, and promotes overall well-being. | Reduces inflammation by regulating blood sugar, improving metabolic function, and enhancing overall health. |
| Stress Management Techniques | Reduces chronic stress, which can exacerbate inflammation. | Reduces inflammation by mitigating the negative impact of stress on the body. |
| Nutritional Supplements (e.g., Vitamin D, Omega-3s, Curcumin) | Offer anti-inflammatory properties, supporting overall health. | May help reduce inflammation by supporting various bodily functions. |
Diagnostic Tests for Inflammation in PCOS
Understanding inflammation in PCOS is crucial for effective management. Different diagnostic tests help identify the presence and extent of inflammation, guiding treatment strategies tailored to individual needs. These tests, when interpreted correctly by healthcare professionals, provide valuable insights into the underlying inflammatory processes affecting PCOS patients.Identifying the presence and extent of inflammation is crucial for personalized treatment approaches.
Different tests provide varying levels of detail, and the choice of test often depends on factors like patient symptoms, cost considerations, and available resources. The results of these tests, combined with clinical assessments, allow healthcare professionals to develop a comprehensive understanding of the patient’s condition and to recommend the most appropriate management strategies.
Common Diagnostic Tests for Inflammation
Various blood tests are commonly employed to assess inflammation in PCOS patients. These tests measure substances in the blood that indicate the presence and degree of inflammation. The interpretation of results is critical, as these markers can fluctuate based on various factors.
- High-Sensitivity C-Reactive Protein (hs-CRP): This blood test measures the level of C-reactive protein (CRP) in the blood. CRP is a protein produced by the liver in response to inflammation. Higher levels of hs-CRP indicate a greater degree of inflammation. A blood sample is collected, and the lab measures the amount of CRP present. Elevated hs-CRP levels can signify underlying inflammation in PCOS, potentially affecting insulin resistance and other symptoms.
This test is non-invasive and relatively inexpensive, making it a valuable initial screening tool.
- Erythrocyte Sedimentation Rate (ESR): ESR measures how quickly red blood cells settle at the bottom of a test tube. Increased settling speed often correlates with inflammation. A blood sample is drawn and allowed to settle in a calibrated tube. The rate at which the red blood cells fall is then measured. A high ESR can suggest inflammation, although it’s not specific to PCOS.
It can be a useful marker for monitoring the inflammatory response over time in conjunction with other tests.
- Complete Blood Count (CBC): A CBC provides a comprehensive overview of the components of the blood, including red blood cells, white blood cells, and platelets. Elevated white blood cell counts can sometimes indicate inflammation. A blood sample is analyzed in a laboratory. Elevated white blood cell counts could suggest inflammation, but they can also be caused by other conditions. This test is a general indicator of inflammation, not specific to PCOS.
Comparing Diagnostic Tests for Inflammation
Different diagnostic tests have varying degrees of accuracy, cost, and invasiveness. The choice of test depends on specific needs and considerations.
| Test | Accuracy | Cost | Invasiveness | Description |
|---|---|---|---|---|
| hs-CRP | Moderate to High | Low | Non-invasive | Measures C-reactive protein, a marker of inflammation. |
| ESR | Moderate | Low | Non-invasive | Measures the rate at which red blood cells settle. |
| CBC | Moderate | Low | Non-invasive | Provides a comprehensive blood count, including white blood cell count. |
Note: Accuracy, cost, and invasiveness can vary depending on the specific laboratory and testing procedures. Consulting with a healthcare professional is essential to determine the most appropriate test for a particular patient.
Illustrative Case Studies: PCOS and Inflammation
Understanding the complex interplay between PCOS and inflammation requires exploring real-world examples. Case studies provide valuable insights into how inflammation manifests in individuals with PCOS, the diagnostic process, and the effectiveness of different treatment approaches. This allows us to gain a more comprehensive understanding of the disease and its management.The following case studies illustrate the relationship between inflammation and PCOS, highlighting the impact of treatment on inflammation markers and PCOS symptoms.
Each case demonstrates the variability of PCOS presentation and the importance of personalized approaches to management.
Case Study 1: A Young Woman with Persistent Acne and Irregular Periods
“A 25-year-old woman presented with a history of irregular menstrual cycles, acne, and fatigue. Her symptoms had worsened over the past two years.”
This patient reported significant discomfort related to the acne, affecting her self-esteem and daily life. Initial blood tests revealed elevated levels of inflammatory markers, including C-reactive protein (CRP) and interleukin-6 (IL-6). These elevated markers suggested a state of chronic low-grade inflammation. Further examination confirmed a diagnosis of PCOS.The treatment plan focused on addressing both the inflammation and the PCOS symptoms.
This included a dietary intervention emphasizing anti-inflammatory foods like fruits, vegetables, and lean protein. Regular exercise and stress-reduction techniques were also incorporated. The patient also started a low-dose oral contraceptive pill to regulate her menstrual cycle and improve hormonal balance. Over the course of three months, the patient observed a significant improvement in her acne and menstrual irregularities.
Repeat blood tests showed a substantial decrease in inflammatory markers. The patient reported feeling more energetic and having increased confidence. This case study demonstrates how a comprehensive approach, addressing both inflammation and hormonal imbalances, can effectively manage PCOS symptoms.
Case Study 2: A Woman with Insulin Resistance and Weight Gain
“A 32-year-old woman presented with insulin resistance, weight gain, and excessive hair growth (hirsutism). She had a family history of PCOS.”
The patient’s symptoms suggested a combination of hormonal and metabolic issues potentially associated with PCOS. Blood tests revealed elevated fasting insulin levels, a key indicator of insulin resistance, and elevated inflammatory markers. Further diagnostic tests confirmed a diagnosis of PCOS.Treatment focused on improving insulin sensitivity and reducing inflammation. This included a combination of lifestyle modifications, such as a balanced diet and regular exercise, as well as metformin to help improve insulin sensitivity.
A dermatologist recommended topical treatments for hirsutism.After six months of treatment, the patient experienced a noticeable decrease in weight and improvement in insulin resistance. Her inflammatory markers also showed a positive response. The patient reported a significant improvement in her overall well-being and quality of life. This case study highlights the crucial role of insulin resistance in PCOS and the importance of addressing it along with inflammation.
Future Directions in Research on PCOS and Inflammation
The intricate relationship between Polycystic Ovary Syndrome (PCOS) and inflammation remains a significant area of ongoing investigation. Understanding the precise mechanisms driving this inflammation is crucial for developing targeted therapies and improving the lives of those affected by PCOS. While current research has shed light on the complex interplay, many unanswered questions persist, paving the way for exciting future discoveries.
Exploring the Underlying Mechanisms
Research efforts are actively focused on dissecting the specific inflammatory pathways involved in PCOS. This involves identifying key inflammatory mediators and exploring their interactions with hormonal imbalances and metabolic dysregulation frequently observed in PCOS. Researchers are investigating the role of specific immune cells and cytokines, aiming to delineate the precise inflammatory responses associated with different PCOS phenotypes. Understanding the cellular and molecular mechanisms underpinning this inflammation will allow for more effective therapeutic strategies.
Developing Novel Therapeutic Targets, The relationship between pcos and inflammation
The development of novel therapies targeting inflammation in PCOS is a critical area of research. One promising avenue involves exploring the potential of anti-inflammatory agents that are currently used in other conditions. Researchers are also investigating the efficacy of natural compounds with anti-inflammatory properties, such as certain plant extracts and dietary components. Careful evaluation of these agents’ safety and efficacy in the context of PCOS is crucial to ensure patient well-being.
Investigating the Role of Gut Microbiota
The gut microbiota plays a significant role in overall health, and emerging evidence suggests its involvement in PCOS-related inflammation. Further research is needed to elucidate the specific mechanisms through which gut microbiota dysbiosis contributes to the inflammatory processes observed in PCOS. This could involve examining the composition of the gut microbiome in women with PCOS compared to healthy controls and exploring the potential of probiotic interventions to mitigate inflammation.
This research may lead to novel dietary strategies or targeted interventions to restore gut microbiota balance.
Personalized Medicine Approaches
Future research should explore personalized medicine approaches to manage PCOS-related inflammation. This involves identifying biomarkers that accurately predict individual responses to different treatments. Researchers are investigating whether specific genetic markers or metabolic profiles can identify women at higher risk for developing inflammation-related PCOS symptoms. Personalized treatments tailored to the individual’s specific inflammatory profile may lead to more effective and efficient management of the condition.
Future Research Directions
- Investigating the role of specific inflammatory cytokines: This research aims to identify the key inflammatory cytokines driving the inflammatory response in PCOS. Identifying these specific inflammatory markers could lead to targeted therapies, allowing for more precise and effective interventions. This would involve in-depth analysis of various inflammatory markers in women with PCOS, correlating these with specific symptoms and severity of the condition.
- Developing targeted therapies to modulate inflammation: This includes exploring new drugs and compounds that selectively target specific inflammatory pathways. Developing these therapies requires meticulous preclinical and clinical trials to assess efficacy and safety in a PCOS population. This could involve testing already-existing anti-inflammatory drugs and exploring their efficacy in reducing PCOS symptoms, focusing on specific inflammatory mediators.
- Evaluating the impact of gut microbiota on inflammation: This research aims to establish a causal link between gut microbiota dysbiosis and the inflammatory processes in PCOS. This will likely involve investigating the composition of the gut microbiome in PCOS patients, exploring potential probiotic interventions to modulate the gut microbiota, and correlating these changes with inflammatory markers.
- Developing biomarkers for predicting treatment response: This research will focus on identifying specific biomarkers that can predict individual responses to various treatments, allowing for personalized treatment plans and optimizing therapeutic outcomes. This would involve investigating various blood and tissue markers, correlating them with inflammation levels, and tracking their response to different interventions. This could potentially lead to more effective and targeted therapies for women with PCOS.
- Investigating the role of environmental factors: Further investigation into the influence of environmental factors, such as exposure to toxins or dietary habits, on PCOS-related inflammation is needed. This could involve exploring correlations between environmental exposures and inflammation markers, potentially identifying modifiable risk factors and developing preventative strategies. This could also involve examining the relationship between dietary components, environmental factors, and inflammatory responses in PCOS.
Last Recap
In conclusion, the relationship between PCOS and inflammation is multifaceted and significant. From understanding the different types of inflammation to exploring potential triggers, impacts on symptoms, and management strategies, this exploration underscores the importance of considering inflammation as a key component in the overall management of PCOS. Further research and improved diagnostic tools will continue to refine our understanding, paving the way for more targeted and effective treatments in the future.