Congestive heart failure vs heart failure is a crucial distinction to understand. This in-depth exploration delves into the nuances of these conditions, examining their similarities and differences, underlying causes, symptoms, diagnostic processes, treatment approaches, prognosis, and prevention strategies. We’ll unpack the complexities of each condition, providing a comprehensive overview to help you navigate this critical health issue.
Understanding the subtle yet significant differences between congestive heart failure (CHF) and heart failure (HF) is paramount. While often used interchangeably, crucial distinctions exist in their presentation, diagnosis, and management. This comprehensive comparison will shed light on the various facets of these related but distinct cardiac conditions.
Defining Congestive Heart Failure and Heart Failure
Heart failure, a complex condition affecting millions worldwide, is often misunderstood. While the terms “congestive heart failure” (CHF) and “heart failure” (HF) are frequently used interchangeably, there are subtle but important distinctions. Understanding these differences is crucial for accurate diagnosis and effective treatment.Heart failure is a chronic condition where the heart is unable to pump blood effectively to meet the body’s needs.
This can lead to a buildup of fluid in the lungs and other parts of the body. Congestive heart failure is a specific type of heart failure characterized by the buildup of fluid, primarily in the lungs and other tissues. The key is that while all CHF is HF, not all HF is CHF.
Defining Congestive Heart Failure (CHF)
Congestive heart failure (CHF) is a clinical syndrome characterized by the inability of the heart to pump enough blood to meet the body’s metabolic demands, leading to fluid buildup in the lungs and other tissues. This buildup results in various symptoms, such as shortness of breath and swelling in the extremities. The primary hallmark of CHF is the congestion that occurs within the circulatory system.
While often used interchangeably, congestive heart failure and heart failure aren’t exactly the same. Understanding the nuances is key, and one important aspect is grade 1 diastolic dysfunction, which involves a subtle but important impairment in the heart’s ability to relax and fill with blood. Grade 1 diastolic dysfunction can be a precursor to more severe heart conditions, and its presence can subtly impact how congestive heart failure presents itself.
Ultimately, a proper diagnosis of congestive heart failure requires a comprehensive understanding of all contributing factors.
Defining Heart Failure (HF)
Heart failure (HF) encompasses a spectrum of conditions where the heart is unable to pump blood effectively to meet the body’s needs. This includes a variety of scenarios, from mild impairment to severe dysfunction. It’s a broad term encompassing various etiologies and presentations, not simply the presence of congestion.
Relationship Between CHF and HF
CHF is a specific type of heart failure. All cases of congestive heart failure are also cases of heart failure. However, heart failure can manifest in ways other than just congestion. For example, heart failure can present with reduced cardiac output without significant congestion.
Key Similarities Between CHF and HF
Both CHF and HF share the core characteristic of impaired cardiac function. Both conditions result in reduced blood flow to the body’s organs and tissues, impacting their ability to function optimally. Symptoms and treatment approaches often overlap.
Differences Between CHF and HF
The primary difference lies in the manifestation of the underlying cardiac dysfunction. CHF is specifically characterized by the fluid buildup, while HF encompasses a broader range of potential mechanisms and presentations. One key difference is the presence or absence of fluid congestion.
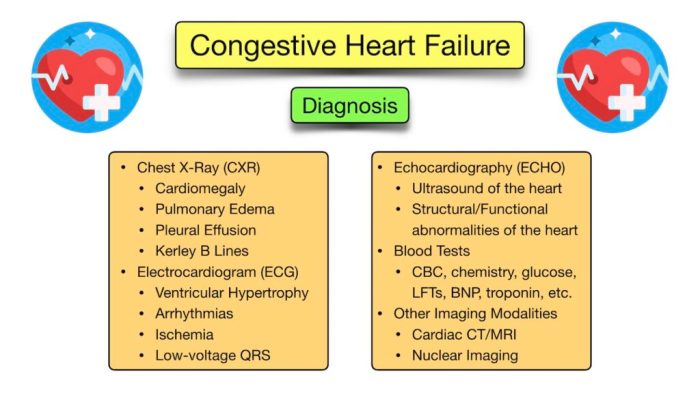
Diagnostic Criteria for CHF and HF
Diagnostic criteria for both CHF and HF rely on a combination of patient history, physical examination findings, and diagnostic tests. These tests may include echocardiograms, blood tests, and chest X-rays. The specific diagnostic criteria for each may vary slightly depending on the particular presentation. In essence, the criteria for diagnosing HF are more general, while those for CHF are more specific.
Comparison of Symptoms
| Symptom | CHF | HF |
|---|---|---|
| Shortness of breath (dyspnea) | Often pronounced, especially with exertion or lying down | Can vary from mild shortness of breath to severe breathlessness |
| Fatigue | Common and often profound | Common, impacting daily activities |
| Edema (swelling) | Typically present in lower extremities, potentially in the abdomen (ascites) | May be present, depending on the type and severity of the heart failure |
| Cough | May be present, often productive of frothy or blood-tinged sputum | May or may not be present |
| Rapid or irregular heartbeat (tachycardia or arrhythmias) | May occur | May occur |
| Chest pain | Possible, but less common | Possible, but less common |
Underlying Causes and Risk Factors
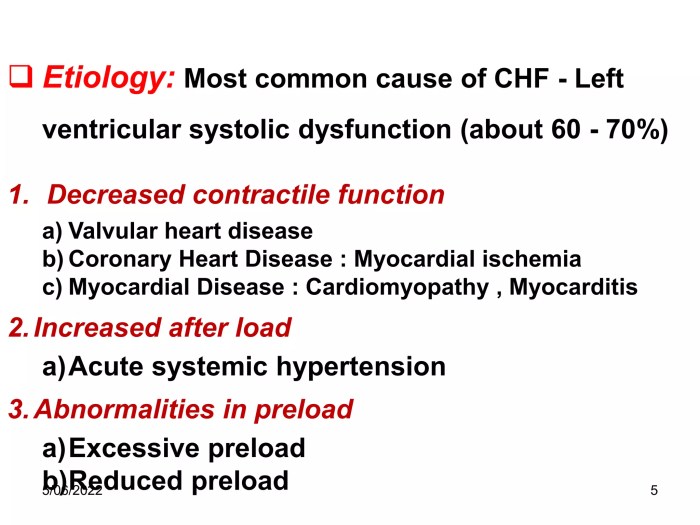
Understanding the causes and risk factors for heart failure (HF), and specifically congestive heart failure (CHF), is crucial for prevention and management. These conditions often stem from a combination of factors, making identification and intervention complex. Identifying individual risk profiles can help healthcare professionals tailor strategies for reducing the likelihood of developing these conditions.Heart failure, in its various forms, results from a complex interplay of underlying conditions.
While the specific mechanisms differ, the common thread is a weakening or dysfunction of the heart’s ability to pump blood efficiently. This ultimately leads to fluid buildup in the body, causing symptoms such as shortness of breath and swelling.
Common Causes of CHF
Congestive heart failure often arises from conditions that directly impact the heart’s ability to contract and relax properly. Coronary artery disease, a narrowing of the arteries supplying blood to the heart, is a leading cause. High blood pressure, persistently elevated blood pressure, damages the heart over time, increasing the risk of CHF. Valvular heart disease, where heart valves don’t open or close correctly, obstructs blood flow and can contribute to CHF.
Myocardial infarction, commonly known as a heart attack, damages the heart muscle, leading to weakening and potential CHF. Cardiomyopathy, a disease of the heart muscle, can cause the heart to enlarge or stiffen, impairing its pumping function and increasing the risk of CHF. Certain infections, such as rheumatic fever, can also damage the heart valves and contribute to CHF.
Common Causes of Heart Failure (HF)
Similar to CHF, various factors contribute to heart failure. High blood pressure, as mentioned, is a major risk. Coronary artery disease, again, significantly impacts the heart’s ability to receive adequate oxygen and can lead to HF. Diabetes, a condition affecting blood sugar regulation, is linked to the development of heart failure due to its impact on blood vessels and the heart itself.
Obesity, characterized by excess body fat, increases the strain on the heart, increasing the risk of heart failure. Certain genetic factors can also increase the likelihood of developing heart failure. A family history of heart conditions significantly elevates the risk. Some medications can also indirectly lead to HF.
So, you’re trying to figure out congestive heart failure vs heart failure? It’s a tricky distinction, but essentially, congestive heart failure is a type of heart failure. Sometimes, unusual symptoms like passing excessive gas can be a sign of underlying health issues, so if you’re concerned about that, check out this helpful guide on when should I worry about passing too much gas.
Regardless of the specific type of heart failure, it’s crucial to discuss any unusual symptoms with your doctor. Knowing the difference between these types of heart conditions is important for appropriate treatment.
Risk Factors for Developing CHF
Several factors increase the likelihood of developing congestive heart failure. A family history of heart conditions is a significant risk factor. High blood pressure is a persistent and powerful risk, often contributing to the weakening of the heart over time. Smoking, with its detrimental effects on blood vessels, also significantly raises the risk. Obesity, characterized by excessive body fat, increases the strain on the heart.
A history of heart attacks or other heart-related events further elevates the risk. Age, as a general factor, is also a risk factor. Certain lifestyle choices, like a diet high in saturated fat and lack of regular exercise, increase the likelihood of developing CHF.
Risk Factors for Developing Heart Failure (HF)
Similarly, various factors increase the risk of developing heart failure. A family history of heart conditions is a significant risk factor. High blood pressure, a common risk factor for heart disease, is a strong predictor of HF. Smoking, due to its harmful effects on blood vessels, is a significant contributor to the development of HF. A history of heart attacks or other heart-related events greatly increases the risk of developing HF.
Diabetes, affecting blood sugar levels, can damage blood vessels and the heart, increasing the risk of HF. Age, as a general factor, is also a risk factor. A sedentary lifestyle and a diet high in saturated fat contribute to the risk.
So, you’re trying to understand congestive heart failure versus just plain heart failure? It’s a bit confusing, isn’t it? One key aspect to consider is what your urinalysis results might reveal, as these can offer clues about the underlying condition. For instance, learning more about the different components of your urinalysis can help doctors distinguish between the two.
what do your urinalysis results mean is a great resource to help you understand how those results connect to potential heart conditions. Ultimately, a thorough evaluation by a medical professional is necessary to correctly diagnose congestive heart failure vs. heart failure.
Comparison of Risk Factors for CHF and HF
While the specific mechanisms of CHF and HF can differ, the underlying risk factors often overlap significantly. Both conditions are strongly associated with a family history of heart disease, high blood pressure, and a history of heart attacks. Both are influenced by lifestyle choices like smoking, obesity, and diet. Age, in general, is also a crucial factor.
The primary difference lies in the specific initiating conditions that trigger the heart’s dysfunction and ultimately lead to fluid buildup (CHF) versus the heart’s inability to pump effectively (HF).
Risk Factor Table
| Category | Risk Factor | Explanation |
|---|---|---|
| Lifestyle | Smoking | Damages blood vessels, increasing the risk of heart disease and subsequent heart failure. |
| Lifestyle | High Blood Pressure | Damages blood vessels and the heart over time, increasing the risk of heart failure. |
| Lifestyle | Obesity | Increases the strain on the heart, leading to heart failure. |
| Lifestyle | Poor Diet | A diet high in saturated fat and cholesterol can increase the risk of heart disease, ultimately contributing to heart failure. |
| Lifestyle | Lack of Exercise | Reduces cardiovascular health and increases the risk of obesity and high blood pressure, increasing the likelihood of heart failure. |
| Medical History | Family History of Heart Disease | Inherited factors increase the susceptibility to heart conditions. |
| Medical History | Previous Heart Attacks | Damages the heart muscle, making it less efficient and more prone to failure. |
| Medical History | Diabetes | Affects blood sugar levels, which can damage blood vessels and the heart, contributing to heart failure. |
| Medical History | Coronary Artery Disease | Narrowing of the arteries supplying blood to the heart reduces oxygen supply, weakening the heart and increasing the risk of heart failure. |
| Age | Advanced Age | The risk of heart conditions increases with age. |
Symptoms and Diagnosis
Understanding the symptoms and diagnostic process is crucial for early detection and effective management of heart failure. Accurate diagnosis allows for personalized treatment plans tailored to individual needs, maximizing the chances of successful outcomes. Early intervention can significantly improve quality of life and potentially extend lifespan.Heart failure, encompassing both congestive heart failure (CHF) and other forms, presents a spectrum of symptoms, often subtle and easily misconstrued.
Accurate diagnosis requires a comprehensive evaluation, combining patient history, physical examination, and various diagnostic tests.
Common Symptoms of CHF
The symptoms of congestive heart failure often manifest gradually, increasing in severity over time. Common symptoms include shortness of breath, especially with exertion or while lying down, swelling in the legs, ankles, and feet (edema), persistent cough or wheezing, rapid or irregular heartbeat, fatigue, and reduced ability to exercise. Fluid buildup in the lungs can cause a characteristic crackling sound (rales) during breathing, audible during a physical examination.
Common Symptoms of Heart Failure, Congestive heart failure vs heart failure
Similar to CHF, symptoms of heart failure often present gradually and worsen over time. Common symptoms include shortness of breath, fatigue, swelling in the legs, ankles, and feet, persistent cough or wheezing, chest pain, and rapid or irregular heartbeat. Individuals may also experience decreased urine output, confusion, and weakness.
Diagnostic Process for CHF
The diagnostic process for congestive heart failure involves a multi-faceted approach. A detailed medical history, including a patient’s lifestyle, risk factors, and prior medical conditions, is essential. A thorough physical examination, focusing on signs of fluid buildup, heart rate, and blood pressure, is critical. This is followed by a series of diagnostic tests, each providing valuable insights into the underlying cause and severity of the condition.
Diagnostic Process for Heart Failure
The diagnostic process for heart failure mirrors that of CHF, emphasizing a comprehensive evaluation. It starts with a detailed patient history, including lifestyle factors, symptoms, and past medical conditions. A physical examination is conducted to assess vital signs, listen to the heart and lungs, and look for signs of fluid retention. Various diagnostic tests are employed to confirm the diagnosis and assess the severity of the condition.
Comparison of Diagnostic Tests for CHF and HF
While the underlying mechanisms may vary slightly between CHF and other forms of heart failure, the diagnostic tests employed often overlap significantly. Both conditions require evaluation of heart function, blood flow, and overall cardiovascular health. Echocardiograms, electrocardiograms, and blood tests are frequently used in both cases. The specific tests and their interpretation are crucial for establishing a definitive diagnosis and guiding appropriate treatment strategies.
Diagnostic Tests and Their Significance
| Test | Description | Significance |
|---|---|---|
| Echocardiogram | An ultrasound of the heart, providing detailed images of heart structure and function. | Evaluates heart chambers, valves, and pumping ability; helps assess ejection fraction (EF), a key indicator of heart function. |
| Electrocardiogram (ECG/EKG) | Records the electrical activity of the heart. | Detects abnormal heart rhythms (arrhythmias), identifies previous heart attacks, and assesses the overall electrical function of the heart. |
| Blood Tests | Measure various blood components, including levels of sodium, potassium, and other electrolytes, as well as cardiac markers. | Helps identify underlying conditions, assess kidney function, and rule out other potential causes of symptoms. |
| Chest X-ray | Provides a visual image of the chest, including the heart and lungs. | Evaluates the size and shape of the heart, detects fluid buildup in the lungs (pulmonary edema), and assesses the overall condition of the lungs. |
| Cardiac Catheterization | A procedure where a thin tube (catheter) is inserted into a blood vessel to access the heart. | Provides detailed information about coronary artery blockages, heart pressure, and blood flow. Used in cases where other tests are inconclusive or in advanced stages of heart failure. |
Treatment Approaches and Management
Heart failure, encompassing both congestive heart failure (CHF) and other forms of heart failure, requires a multifaceted approach to treatment and management. Effective strategies address the underlying causes, reduce symptoms, and improve quality of life. The treatment plans often overlap but may differ in specific medications and intensity of lifestyle modifications based on the individual’s condition.Medical treatments are crucial for managing heart failure, but a comprehensive approach that incorporates lifestyle modifications is essential for long-term success.
These strategies, when implemented consistently, can significantly impact the progression of the disease and enhance the patient’s overall well-being.
Medical Treatments for CHF
Medical treatments for CHF focus on improving cardiac function, reducing fluid buildup, and managing associated symptoms. Pharmacological interventions are commonly employed, targeting specific mechanisms like improving heart contractions, reducing blood pressure, and managing fluid retention. Angiotensin-converting enzyme (ACE) inhibitors, beta-blockers, and diuretics are frequently prescribed. In severe cases, implantable cardiac devices like pacemakers or defibrillators may be considered.
Some patients may also benefit from specialized procedures like cardiac resynchronization therapy (CRT).
Medical Treatments for HF
Similar to CHF, medical treatments for heart failure (HF) aim to improve heart function, reduce symptoms, and prevent disease progression. Pharmacological interventions remain a cornerstone of treatment, addressing issues like fluid overload, blood pressure regulation, and heart rhythm disturbances. Commonly prescribed medications include ACE inhibitors, beta-blockers, and diuretics, as well as other drugs targeting specific aspects of heart failure.
In advanced cases, advanced interventions like cardiac resynchronization therapy (CRT) or other advanced therapies may be necessary.
Comparison of Treatment Plans
The treatment plans for CHF and other forms of heart failure often share overlapping medications and lifestyle modifications. However, the intensity and specific choices may vary depending on the severity of the condition and the individual patient’s response. For example, a patient with mild CHF might primarily benefit from lifestyle changes and certain medications, whereas a patient with severe CHF might require more intensive therapies, including specialized procedures.
Importance of Lifestyle Modifications in Managing CHF
Lifestyle modifications play a critical role in managing CHF. A balanced diet, regular exercise, and stress management techniques are crucial for improving overall health and reducing the strain on the heart. Weight management is particularly important, as excess weight exacerbates the workload on the heart. Avoiding smoking and excessive alcohol consumption are also vital for maintaining cardiovascular health.
Importance of Lifestyle Modifications in Managing HF
Similar to CHF, lifestyle modifications are crucial for managing HF. A healthy diet, regular exercise, stress management, and weight management are essential for improving cardiac function and reducing symptoms. Managing risk factors such as high blood pressure, high cholesterol, and diabetes is also vital for preventing the progression of heart failure. The positive impact of these changes is well-documented.
How Lifestyle Changes Prevent Progression
Lifestyle modifications, when consistently practiced, can significantly slow the progression of CHF and HF. Regular exercise strengthens the heart muscle, improving its efficiency. A balanced diet reduces the workload on the heart by maintaining a healthy weight and managing blood pressure and cholesterol levels. Stress management techniques help reduce the impact of stress hormones on the cardiovascular system.
These measures, when combined with appropriate medical treatments, can significantly improve outcomes and extend the quality of life for individuals with heart failure.
Treatment Options Table
| Treatment | Description | Effectiveness |
|---|---|---|
| ACE Inhibitors | Reduce blood pressure and improve heart function. | Generally highly effective in reducing symptoms and slowing disease progression. |
| Beta-Blockers | Slow heart rate and reduce workload on the heart. | Effective in reducing symptoms and improving survival rates. |
| Diuretics | Remove excess fluid from the body. | Effective in relieving fluid overload and improving breathing. |
| Implantable Cardioverter-Defibrillators (ICDs) | Provide electrical shocks to correct irregular heartbeats. | Effective in preventing sudden cardiac death in high-risk patients. |
| Cardiac Resynchronization Therapy (CRT) | Coordinate the electrical activity of the heart. | Effective in improving heart function and reducing symptoms in certain patients. |
| Lifestyle Modifications (Diet, Exercise, Stress Management) | Improve overall health and reduce strain on the heart. | Essential for long-term management and preventing progression of heart failure. |
Prognosis and Long-Term Outcomes
Heart failure, encompassing both congestive heart failure (CHF) and other forms of heart failure (HF), significantly impacts a patient’s long-term well-being. Understanding the prognosis and potential complications is crucial for effective management and patient support. This section delves into the factors that influence the long-term outcomes for both CHF and HF, along with the potential complications and the importance of regular follow-up care.
Prognosis of Congestive Heart Failure (CHF)
The prognosis for CHF varies greatly depending on several factors, including the severity of the underlying heart condition, the presence of other health issues, and the patient’s overall health status. Patients with stable CHF and well-managed conditions often maintain a reasonable quality of life, albeit with ongoing limitations. However, advanced stages of CHF can lead to a more serious prognosis, potentially impacting lifespan.
The progression of CHF is often gradual but unpredictable.
Prognosis of Heart Failure (HF)
Heart failure, in its broader definition, encompasses a range of conditions. The prognosis for HF varies significantly depending on the specific type of heart failure, the severity of the condition, and the effectiveness of treatment. Factors such as age, overall health, and the presence of co-morbidities influence the trajectory of the disease. The course of HF is not always uniform, and its progression can be unpredictable.
Factors Influencing Long-Term Outcomes for CHF
Several factors influence the long-term outcomes for patients with CHF. These factors include:
- Severity of heart damage: The extent of the underlying heart damage plays a crucial role. More severe damage generally leads to a poorer prognosis. For example, a patient with severe left ventricular dysfunction is more likely to experience adverse outcomes compared to someone with mild dysfunction.
- Presence of other health conditions: Co-morbidities like diabetes, high blood pressure, or kidney disease can significantly impact the course of CHF. These conditions can exacerbate symptoms and lead to more rapid progression.
- Adherence to treatment plan: A patient’s willingness and ability to follow the prescribed treatment plan is a key factor. Regular medication intake, lifestyle modifications, and adherence to medical recommendations directly impact the long-term outcome.
- Overall health status: The patient’s general health, including their nutritional status, physical activity levels, and mental well-being, all contribute to the long-term outcomes. Healthy lifestyle choices often translate to better outcomes for patients with CHF.
Factors Influencing Long-Term Outcomes for HF
Similar to CHF, several factors influence the long-term outcomes for HF. These include:
- Type of heart failure: Different types of HF, such as systolic or diastolic failure, have varying prognoses. For instance, systolic heart failure, characterized by the heart’s inability to pump effectively, typically carries a more significant impact on long-term outcomes than diastolic heart failure.
- Underlying cause: The specific cause of the HF, such as coronary artery disease or valvular heart disease, impacts the prognosis. For example, HF resulting from a known and treatable cause may have a more favorable outlook compared to HF with an unidentified etiology.
- Age and overall health: Age and the presence of other health conditions significantly affect the prognosis. Older individuals and those with multiple co-morbidities often face a less favorable prognosis.
- Treatment response: The patient’s response to treatment, including medication and lifestyle modifications, is a critical factor. Patients who respond well to treatment generally have better long-term outcomes.
Potential Complications of CHF and HF
CHF and HF can lead to a range of serious complications. These include:
- Kidney damage: The reduced blood flow to the kidneys can damage kidney function.
- Liver damage: Reduced blood flow to the liver can lead to liver problems.
- Respiratory problems: Fluid buildup in the lungs can cause breathing difficulties.
- Heart rhythm disturbances: HF can lead to abnormal heart rhythms, which can further compromise heart function.
Importance of Regular Follow-up Care
Regular follow-up care is essential for managing CHF and HF effectively. Regular check-ups allow healthcare providers to monitor the patient’s condition, adjust treatment plans as needed, and detect any complications early. Early detection and intervention can significantly improve outcomes.
Comparison of Potential Outcomes
| Factor | CHF Outcome | HF Outcome |
|---|---|---|
| Severity of heart damage | Poorer prognosis with more severe damage | Poorer prognosis with more severe damage, varying by specific type |
| Presence of other health conditions | Adverse outcomes with co-morbidities | Adverse outcomes with co-morbidities, varying by specific type |
| Treatment adherence | Better outcomes with good adherence | Better outcomes with good adherence, varying by specific type |
| Overall health | Better outcomes with good health | Better outcomes with good health, varying by specific type |
Prevention and Early Detection: Congestive Heart Failure Vs Heart Failure
Heart failure, whether congestive (CHF) or simply heart failure (HF), is a serious condition that can significantly impact quality of life. Proactive measures, encompassing lifestyle changes and vigilant monitoring, are crucial in preventing its onset or delaying its progression. Early detection is equally vital, as timely intervention can dramatically improve outcomes. Understanding the strategies for both prevention and early detection is paramount for those at risk or concerned about their heart health.Early detection and proactive prevention are not just about delaying the inevitable; they’re about empowering individuals to take control of their heart health and potentially avoid the debilitating effects of heart failure.
By understanding risk factors and implementing preventive strategies, individuals can significantly reduce their chances of developing this condition.
Strategies for Preventing CHF and HF
Lifestyle modifications play a significant role in reducing the risk of developing heart failure. Maintaining a healthy weight, managing blood pressure and cholesterol levels, and quitting smoking are cornerstones of preventative care. A balanced diet rich in fruits, vegetables, and whole grains, coupled with regular physical activity, further supports cardiovascular health.
Strategies for Preventing CHF and HF
A comprehensive approach is necessary to prevent heart failure. This involves addressing underlying risk factors and adopting healthy lifestyle choices. Regular medical checkups and adherence to prescribed medications are essential. Individuals with pre-existing conditions, such as high blood pressure or diabetes, require meticulous management to minimize the risk of heart failure. Furthermore, understanding and managing stress levels is vital, as chronic stress can negatively impact cardiovascular health.
Importance of Early Detection
Early detection of heart failure symptoms is crucial for effective treatment and improved outcomes. Prompt diagnosis allows for timely intervention, potentially slowing disease progression and mitigating its impact on daily life. Early intervention often involves adjustments to medications, lifestyle changes, and, in some cases, advanced therapies.
Methods for Identifying Early Signs and Symptoms
Recognizing the early warning signs of heart failure is critical. Common symptoms include shortness of breath, especially with exertion, persistent cough or wheezing, swelling in the ankles, feet, or legs, fatigue, and rapid or irregular heartbeat. Noticeable weight gain, often due to fluid retention, can also be an early indicator. It’s important to remember that these symptoms may not always be indicative of heart failure, but they warrant a prompt visit to a healthcare professional for proper evaluation.
Examples of Preventive Measures
Implementing preventive measures is a cornerstone of managing heart health and minimizing the risk of heart failure. A comprehensive strategy includes:
- Maintaining a healthy weight through a balanced diet and regular exercise.
- Controlling blood pressure and cholesterol levels through lifestyle modifications and medication if necessary.
- Quitting smoking to reduce cardiovascular strain.
- Managing underlying conditions like diabetes and high blood pressure through medication and lifestyle changes.
- Engaging in regular physical activity to strengthen the heart muscle and improve circulation.
- Following a heart-healthy diet rich in fruits, vegetables, and whole grains, while limiting saturated and trans fats.
- Managing stress levels through relaxation techniques, mindfulness, and sufficient sleep.
- Regular check-ups with a healthcare provider to monitor overall health and identify potential risks early.
Strategies for Reducing the Risk
Implementing a multi-faceted approach is essential in reducing the risk of developing heart failure. This involves adopting a healthy lifestyle, effectively managing underlying conditions, and maintaining regular communication with healthcare providers. Early detection and proactive interventions can significantly minimize the risk and impact of this potentially serious condition.
Preventive Measures
- Maintain a healthy weight: A balanced diet and regular exercise contribute significantly to maintaining a healthy weight, which is crucial in preventing heart failure.
- Control blood pressure and cholesterol: Regular monitoring and appropriate management of blood pressure and cholesterol are vital in reducing cardiovascular strain and preventing heart failure.
- Quit smoking: Smoking significantly increases the risk of heart failure. Quitting is a crucial step in minimizing cardiovascular risks.
- Manage underlying conditions: Effective management of conditions like diabetes and high blood pressure is essential to minimize the risk of heart failure.
- Engage in regular physical activity: Regular exercise strengthens the heart muscle and improves circulation, contributing to a lower risk of heart failure.
- Follow a heart-healthy diet: A diet rich in fruits, vegetables, and whole grains, coupled with a reduction in saturated and trans fats, is crucial for cardiovascular health.
- Manage stress: Chronic stress can negatively impact heart health. Implementing stress-reducing techniques can minimize cardiovascular risks.
Wrap-Up
In conclusion, understanding the differences between congestive heart failure and heart failure is essential for effective diagnosis and treatment. This comparison highlights the critical similarities and differences in symptoms, causes, diagnostics, and management strategies. Armed with this knowledge, individuals and healthcare providers can better navigate the complexities of these conditions, promoting proactive health management and improved outcomes.










