Different types of obesity, a complex and multifaceted health issue, encompass a range of factors impacting body composition and overall well-being. Understanding the variations in fat distribution, genetic predispositions, environmental influences, and associated health risks is crucial for effective management and prevention strategies. This exploration delves into the intricacies of various obesity types, highlighting the interplay of genetics, lifestyle, and medical considerations.
From the role of body mass index (BMI) and its limitations to the impact of visceral fat and subcutaneous fat distribution, this in-depth look at different types of obesity will equip you with a comprehensive understanding of this critical health concern. We will analyze how various factors contribute to obesity and explore the potential consequences on your health.
Defining Obesity
Obesity is a complex health issue characterized by excessive body fat accumulation, which poses significant risks to overall well-being. Understanding its definition is crucial for accurate diagnosis and effective treatment strategies. This involves not only measuring body weight but also considering various factors influencing body composition and health.Defining obesity requires a multifaceted approach, moving beyond simple weight measurements to encompass the broader impact on health.
The medical community uses different criteria and metrics to diagnose obesity, recognizing the limitations of relying solely on one measure. Understanding these nuances is vital for developing personalized interventions tailored to individual needs.
Defining Obesity: Medical Perspectives
Obesity is not simply an excess of weight. It’s a complex metabolic disorder characterized by an excessive accumulation of body fat, often associated with an increased risk of chronic diseases. Different medical guidelines and research approaches define obesity based on various factors and their interplay. The understanding of obesity has evolved significantly over time, reflecting the increasing complexity of the condition.
Body Mass Index (BMI) and its Limitations
BMI, a widely used measure, calculates body weight relative to height. It provides a general indication of body fat, but it doesn’t account for variations in body composition. For instance, individuals with high muscle mass may have a higher BMI than those with a similar weight but less muscle mass.
BMI = weight (kg) / height2 (m 2)
Different BMI categories are used to categorize individuals based on risk:
- Underweight: BMI less than 18.5
- Normal weight: BMI between 18.5 and 24.9
- Overweight: BMI between 25 and 29.9
- Obese Class I: BMI between 30 and 34.9
- Obese Class II: BMI between 35 and 39.9
- Obese Class III (Severe Obesity): BMI of 40 or greater
These categories provide a framework for assessing risk, but they don’t fully capture the individual’s health status. Someone with a BMI in the overweight range could have a healthier body composition than someone with a similar BMI but a higher percentage of body fat.
Beyond BMI: Waist Circumference and Body Composition
Waist circumference is a crucial measure of abdominal fat, often a better predictor of health risks than BMI alone. Excess abdominal fat is linked to a higher risk of cardiovascular disease and type 2 diabetes. Body composition analysis, which measures the proportion of fat, muscle, and bone mass, offers a more detailed understanding of an individual’s physique.
- Waist circumference is measured in centimeters, and a larger waist circumference often correlates with higher health risks.
- Body composition analysis, using techniques like DEXA scans, helps determine the proportion of fat, muscle, and bone in the body.
Comparing Definitions of Obesity Across Guidelines
Different medical organizations and guidelines use varying criteria for defining obesity. This can lead to some inconsistencies in diagnoses and treatment approaches.
| Organization/Guideline | Definition of Obesity |
|---|---|
| World Health Organization (WHO) | Based on BMI, but with consideration for other risk factors. |
| National Institutes of Health (NIH) | Uses BMI, but emphasizes the importance of waist circumference and other health indicators. |
| American Heart Association (AHA) | Focuses on the relationship between obesity and cardiovascular health, with a particular emphasis on waist circumference. |
These variations highlight the evolving understanding of obesity and the need for a more comprehensive approach to diagnosis and management.
Types of Obesity Based on Distribution
Understanding obesity isn’t just about the overall amount of body fat; it’s crucial to consider how that fat is distributed. Different fat storage patterns correlate with varying health risks. This distinction helps doctors tailor treatment plans and predict potential health problems more accurately.
Visceral vs. Subcutaneous Fat
Visceral fat, often referred to as “belly fat,” is stored deep within the abdomen, surrounding the internal organs. Subcutaneous fat, on the other hand, is located directly beneath the skin, primarily in areas like the hips and thighs. The difference in location significantly impacts health.
Health Implications of Fat Distribution
Visceral fat is particularly problematic due to its close proximity to vital organs. This proximity leads to increased inflammation and hormonal imbalances, which are linked to a higher risk of chronic diseases. Subcutaneous fat, while still contributing to obesity, tends to have a less direct and significant impact on metabolic function. The body’s ability to process insulin is directly affected by visceral fat accumulation.
Understanding the different types of obesity is crucial for effective treatment, but did you know that certain health conditions can be linked? For example, some studies suggest a potential correlation between obesity and age-related macular degeneration. Learning more about the factors influencing this connection is key. Checking out age related macular degeneration facts can provide valuable insights.
Ultimately, understanding the various types of obesity remains essential for a holistic approach to patient care.
Correlation with Metabolic Syndrome
Abdominal obesity, characterized by a high level of visceral fat, is strongly correlated with metabolic syndrome. Metabolic syndrome is a cluster of conditions that increase the risk of heart disease, stroke, and type 2 diabetes. Individuals with abdominal obesity often exhibit insulin resistance, high blood pressure, high blood sugar, and abnormal cholesterol levels. These combined factors significantly increase the risk of developing cardiovascular issues.
Clinical Features and Associated Risks, Different types of obesity
| Fat Distribution Type | Clinical Features | Associated Risks |
|---|---|---|
| Visceral Fat | Increased waist circumference, deep abdominal fat, apple-shaped body type, higher insulin resistance, elevated blood pressure, dyslipidemia (abnormal blood fats). | Increased risk of type 2 diabetes, cardiovascular disease (heart disease and stroke), non-alcoholic fatty liver disease, some types of cancer, sleep apnea, and osteoarthritis. |
| Subcutaneous Fat | Fat accumulation primarily under the skin, pear-shaped body type, less significant impact on insulin resistance and blood pressure compared to visceral fat. | Increased risk of type 2 diabetes (though less pronounced than with visceral fat), cardiovascular disease (though less pronounced than with visceral fat), and some types of cancer. However, these risks are often influenced by the overall body fat percentage. |
Note: Waist circumference measurements are often used to assess abdominal obesity risk.
Genetic Predisposition to Obesity
Our understanding of obesity is constantly evolving, and a crucial aspect is recognizing the role of genetics in influencing our susceptibility to this complex condition. While environmental factors undoubtedly play a significant part, inheriting specific genetic predispositions can significantly impact an individual’s likelihood of developing obesity. This is not a simple “gene-on” or “gene-off” switch; rather, it’s a complex interplay of multiple genes and environmental influences that determine an individual’s weight.Genes influence various aspects of metabolism, appetite regulation, and energy expenditure.
Some individuals may be predisposed to store fat more readily, have a higher appetite, or experience a slower metabolism, all of which contribute to a greater risk of weight gain. These predispositions, combined with environmental factors like diet and lifestyle choices, can lead to the development of obesity. Understanding the genetic landscape of obesity is critical for developing personalized strategies to prevent and manage this condition.
The Influence of Genes on Weight Regulation
Genes play a pivotal role in controlling numerous processes related to weight regulation. They influence how the body metabolizes food, how much energy is burned, and the signals that tell us when we’re hungry or full. Variations in these genes can impact an individual’s susceptibility to weight gain. The impact of genetic mutations on weight regulation is often complex and multifaceted.
Understanding the different types of obesity is crucial for personalized treatment plans. While recovering from food poisoning, a delicate approach to nutrition is paramount. Following a diet like the one recommended in what to eat after food poisoning is key to restoring your body’s balance and preventing further complications. This is especially important because different types of obesity often have unique underlying causes, which affect how your body reacts to various foods.
Specific Genetic Mutations and Their Impact
Specific genetic mutations can directly affect weight regulation pathways. These mutations can alter the production or function of hormones, enzymes, and receptors involved in appetite control, energy expenditure, and fat storage. Examples include variations in genes related to leptin and ghrelin, hormones that regulate appetite, and genes involved in fat metabolism and storage. Understanding these mutations is crucial for developing targeted interventions.
Interaction of Genes and Environment
Obesity is not solely determined by genetics. Environmental factors, such as diet, physical activity, and lifestyle choices, play a crucial role in shaping an individual’s weight. The interplay between genetic predisposition and environmental factors is complex and can be visualized as a spectrum. Individuals with a strong genetic predisposition to obesity may be more susceptible to weight gain in environments characterized by high-calorie diets and low physical activity levels.
Conversely, individuals with a weaker genetic predisposition may still develop obesity if exposed to highly obesogenic environments. This highlights the importance of considering both genetic and environmental influences when addressing obesity.
Examples of Genetic-Environmental Interactions
Consider a person with a genetic predisposition for a slower metabolism. In a high-calorie, sedentary environment, this predisposition may manifest as significant weight gain. On the other hand, the same genetic predisposition in a healthy environment, where the individual actively maintains a balanced diet and regular exercise regimen, might not result in obesity. This exemplifies the dynamic interplay between genes and environment in shaping an individual’s weight.
Comparison of Genes Associated with Obesity Risk
| Gene | Mechanism of Action |
|---|---|
| FTO | Associated with changes in appetite regulation and energy expenditure. Variations in the FTO gene have been linked to increased food intake and reduced energy expenditure. |
| MC4R | Plays a critical role in regulating appetite and satiety. Mutations in the MC4R gene can lead to increased appetite and decreased satiety, potentially contributing to weight gain. |
| LEP | Codes for leptin, a hormone that signals the brain about energy stores. Variations in the LEP gene or its receptor can disrupt the body’s ability to regulate appetite and energy balance. |
| POMC | Involved in the production of hormones that regulate appetite and metabolism. Mutations in the POMC gene can lead to an imbalance in these hormones, impacting weight regulation. |
Environmental Factors Contributing to Obesity
Our environment plays a significant role in shaping our health, including our weight. Factors like dietary choices, physical activity levels, and socioeconomic conditions all intersect to influence the prevalence of obesity. Understanding these elements is crucial for developing effective strategies to combat this global health concern.Beyond genetics and individual choices, external forces mold our behaviors and access to resources, thereby impacting our likelihood of becoming obese.
The interplay of these environmental factors often leads to a cycle of poor health outcomes, highlighting the need for comprehensive approaches to address obesity.
Dietary Habits and Obesity
A diet high in processed foods, sugary drinks, and unhealthy fats contributes significantly to weight gain. These foods often lack essential nutrients and are typically high in calories, leading to energy imbalances and promoting fat storage. A lack of fruits, vegetables, and whole grains further exacerbates the problem. The availability and affordability of these foods also play a crucial role, as readily accessible and inexpensive options often prioritize processed ingredients.
Physical Activity Levels and Weight Management
Insufficient physical activity is a major contributor to obesity. Modern lifestyles, characterized by prolonged periods of sitting and sedentary work, often restrict opportunities for exercise. This lack of movement reduces calorie expenditure, exacerbating the effects of a high-calorie diet. Furthermore, limited access to safe and affordable recreational facilities further hinders opportunities for physical activity, especially in disadvantaged communities.
Socioeconomic Factors and Obesity Rates
Socioeconomic disparities significantly influence obesity rates. Individuals in lower socioeconomic groups often face limited access to healthy food options and have reduced opportunities for physical activity due to factors like lack of safe recreational areas and financial constraints. These conditions can lead to increased consumption of affordable, energy-dense, processed foods, and limited opportunities for active lifestyles. Additionally, stress related to poverty and financial insecurity can influence hormone levels and contribute to weight gain.
Correlation Between Environmental Factors and Obesity Prevalence
| Environmental Factor | Specific Impact on Obesity | Prevalence Correlation |
|---|---|---|
| High Availability of Processed Foods | Increased consumption of calorie-dense, nutrient-poor foods, contributing to energy imbalance. | Strong positive correlation. Studies show that areas with higher density of fast-food restaurants tend to have higher obesity rates. |
| Limited Access to Healthy Foods | Reduced intake of fruits, vegetables, and whole grains, leading to nutritional deficiencies and potential weight gain. | Strong positive correlation. Food deserts, where healthy food options are scarce, are often associated with higher obesity rates. |
| Lack of Physical Activity Opportunities | Reduced calorie expenditure, leading to an imbalance between calorie intake and energy expenditure. | Strong positive correlation. Communities with limited parks, playgrounds, and safe walking paths often exhibit higher obesity rates. |
| Socioeconomic Disadvantage | Limited access to healthy food options, financial constraints, and stress, all potentially leading to weight gain. | Strong positive correlation. Studies show a clear link between lower socioeconomic status and higher obesity prevalence. |
| Sedentary Work Environments | Prolonged periods of sitting, reducing opportunities for physical activity. | Moderate to strong positive correlation. Office workers, for example, may experience higher obesity rates compared to those with physically demanding jobs. |
Obesity and Associated Health Risks

Obesity is a significant public health concern, not only for the physical discomfort it can cause but also for the myriad of serious health complications it can trigger. These complications often impact multiple organ systems, leading to a reduced quality of life and increased risk of premature mortality. Understanding the connections between obesity and various diseases is crucial for developing effective prevention and treatment strategies.
Cardiovascular Disease
Obesity significantly increases the risk of developing cardiovascular diseases. Excess body fat contributes to elevated blood pressure, high cholesterol levels, and insulin resistance. These factors create a pro-inflammatory environment in the body, increasing the risk of atherosclerosis, the buildup of plaque in the arteries. This plaque buildup can lead to narrowed arteries, reducing blood flow to vital organs and increasing the risk of heart attacks and strokes.
For example, individuals with obesity often exhibit higher levels of triglycerides and low-density lipoprotein (LDL) cholesterol, which are crucial risk factors for heart disease.
Type 2 Diabetes
Obesity is a major contributor to the development of type 2 diabetes. The excess fat tissue in obese individuals often leads to insulin resistance. This means that the body’s cells do not respond effectively to insulin, a hormone that regulates blood sugar levels. As a result, blood sugar levels rise, increasing the risk of developing type 2 diabetes.
The strong correlation between obesity and type 2 diabetes is well-documented in numerous studies and clinical observations.
Sleep Apnea
Obesity is a significant risk factor for sleep apnea. The excess weight and fat accumulation around the neck can narrow the airway, making it difficult to breathe during sleep. This can lead to pauses in breathing, known as apneas, which disrupt sleep patterns and reduce the amount of restful sleep. These sleep disruptions can have serious consequences, including daytime fatigue, impaired cognitive function, and increased risk of cardiovascular problems.
For instance, a person with moderate to severe obesity might experience 30 or more apneas per hour during sleep, leading to significant sleep deprivation.
Osteoarthritis
Obesity significantly increases the risk of developing osteoarthritis. The extra weight places a substantial mechanical load on joints, particularly weight-bearing joints like the knees and hips. This increased stress can accelerate the breakdown of cartilage, leading to pain, stiffness, and reduced joint function. The repetitive stress and strain on the joints, caused by the extra weight, can damage cartilage and lead to inflammation, which are key factors in the development of osteoarthritis.
This can be particularly debilitating in individuals with severe obesity.
Other Health Complications Linked to Obesity
| Health Complication | Description |
|---|---|
| Gallstones | Excess weight can increase the risk of gallstones formation. |
| Certain Cancers | Studies suggest a link between obesity and increased risk of some types of cancer, including colon, breast, and endometrial cancers. |
| Mental Health Conditions | Obesity has been associated with an increased risk of depression, anxiety, and other mental health conditions. |
| Fatty Liver Disease | Accumulation of fat in the liver is common in obese individuals and can lead to inflammation and liver damage. |
| Reproductive Issues | Obesity can affect fertility in both men and women. |
Diagnostic Methods for Different Obesity Types
Pinpointing the precise type of obesity is crucial for effective treatment strategies. This involves a multi-faceted approach that goes beyond simply measuring weight. Understanding the underlying causes and contributing factors is essential for tailoring interventions to address the specific needs of each individual. This section delves into the various diagnostic methods employed to identify different obesity types.Accurate diagnosis requires a comprehensive evaluation, combining objective measurements with a thorough understanding of an individual’s medical history, lifestyle, and potential genetic predispositions.
This multifaceted assessment ensures that treatment plans are not only effective but also personalized, taking into account the specific characteristics of each case.
Procedures Used to Diagnose Obesity
A proper diagnosis of obesity encompasses a range of procedures that assess various aspects of the individual’s health. These procedures not only measure weight and body mass index (BMI), but also investigate the underlying factors contributing to the condition. This comprehensive approach ensures a complete understanding of the individual’s health status and helps tailor treatment plans accordingly.The process usually begins with a detailed medical history, including a review of family medical history, lifestyle factors, and any existing health conditions.
A thorough physical examination is conducted to assess vital signs, including blood pressure, heart rate, and respiratory rate. Further evaluations may involve blood tests to assess metabolic markers, such as cholesterol levels and glucose tolerance.
Role of Medical Imaging in Assessing Body Composition
Medical imaging plays a vital role in assessing body composition beyond just weight and BMI. Techniques like dual-energy X-ray absorptiometry (DEXA) provide a detailed analysis of bone mineral density, fat mass, and lean muscle mass. This information is crucial for understanding the distribution of fat within the body, distinguishing between different types of obesity, and assessing the overall health risks associated with the condition.
Computed tomography (CT) scans and magnetic resonance imaging (MRI) can also be used to evaluate visceral fat accumulation in the abdomen, which is often associated with increased health risks.
Importance of Conducting Thorough Physical Examinations
A comprehensive physical examination is indispensable in diagnosing obesity and identifying potential associated health risks. It involves evaluating various systems of the body, including the cardiovascular, respiratory, and musculoskeletal systems. This examination can reveal signs of complications arising from obesity, such as high blood pressure, sleep apnea, or joint pain. Furthermore, a thorough physical exam helps to identify any underlying medical conditions that may be contributing to or exacerbating obesity.
Comparing and Contrasting Diagnostic Methods
| Diagnostic Method | Description | Advantages | Disadvantages | Suitability for Different Obesity Types |
|---|---|---|---|---|
| Weight and BMI Measurement | Basic measurement of body weight and calculation of body mass index. | Simple, inexpensive, and readily available. | Does not provide information on body composition or fat distribution. | Useful as a first screening tool for all obesity types. |
| Dual-Energy X-ray Absorptiometry (DEXA) | Uses X-rays to measure bone mineral density, fat mass, and lean muscle mass. | Precisely assesses body composition, including fat distribution. | Requires specialized equipment and trained personnel. Can be expensive. | Especially valuable for identifying central obesity and assessing overall health risks. |
| Computed Tomography (CT) Scan | Uses X-rays to create cross-sectional images of the body. | Can visualize visceral fat accumulation, useful in assessing metabolic risk. | Exposure to ionizing radiation. More expensive than DEXA. | Beneficial in diagnosing abdominal obesity and associated metabolic complications. |
| Magnetic Resonance Imaging (MRI) | Uses magnetic fields and radio waves to create detailed images of the body. | Excellent soft tissue contrast, provides detailed images of organs and tissues. | Can be more expensive than CT scans, may not be suitable for individuals with certain medical conditions or implants. | Useful for comprehensive assessment of body composition and identifying potential complications. |
Management Strategies for Different Obesity Types
Obesity management is a multifaceted process that requires a personalized approach. Success hinges on understanding the underlying causes of obesity in each individual, including genetic predispositions, environmental factors, and existing health conditions. Effective management strategies integrate lifestyle modifications, dietary interventions, physical activity, and potentially, pharmaceutical interventions. The goal is not just weight loss, but also the improvement of overall health and well-being.Successful management of obesity involves addressing the interplay of various factors.
This approach recognizes that one-size-fits-all solutions are rarely effective. Instead, it emphasizes tailored interventions that consider individual needs and circumstances. By acknowledging the complex nature of obesity, we can move towards more sustainable and effective long-term management strategies.
Understanding the different types of obesity is crucial for effective treatment strategies. While various factors contribute to the condition, some research suggests that incorporating natural remedies like turmeric and black pepper into your diet might be beneficial. A recent study explored the potential synergistic effects of these spices, specifically focusing on their impact on the body’s metabolic processes.
For a deeper dive into the potential benefits of turmeric and black pepper, check out this informative article on the subject: turmeric and black pepper. Ultimately, a comprehensive approach, considering individual needs and diverse forms of obesity, remains key to managing this health concern effectively.
Lifestyle Modifications for Obesity Management
Lifestyle modifications are the cornerstone of obesity management. They involve fundamental changes to daily habits, promoting healthier choices across various aspects of life. These changes are crucial for long-term weight loss and maintenance, aiming to reduce the overall energy intake and increase energy expenditure.
- Balanced Diet Planning: Developing a personalized dietary plan that prioritizes nutrient-rich foods while controlling portion sizes is crucial. This plan must be tailored to individual preferences and cultural contexts, ensuring that it is sustainable and enjoyable.
- Regular Physical Activity: Incorporating regular physical activity into daily routines is essential. This can include a variety of activities, from brisk walking to swimming, and should be gradually increased to maintain motivation and avoid injury. The goal is to achieve at least 150 minutes of moderate-intensity or 75 minutes of vigorous-intensity aerobic activity per week.
- Stress Management Techniques: Chronic stress can negatively impact weight management. Integrating stress-reduction techniques, such as mindfulness, yoga, or meditation, can contribute to overall well-being and improve adherence to lifestyle changes.
Dietary Interventions in Weight Loss and Maintenance
Dietary interventions play a vital role in weight management. Choosing the right foods and controlling portion sizes are crucial components of a successful weight loss strategy. A balanced diet, rich in fruits, vegetables, lean proteins, and whole grains, is essential for sustained weight loss and long-term health.
- Calorie Control: Creating a calorie deficit is a cornerstone of weight loss. A registered dietitian or nutritionist can help calculate appropriate calorie targets based on individual needs and activity levels.
- Nutrient-Dense Foods: Prioritizing nutrient-dense foods, such as fruits, vegetables, lean proteins, and whole grains, over processed foods, sugary drinks, and excessive fats is essential for maintaining overall health and well-being.
- Portion Control: Controlling portion sizes is equally important. Using smaller plates, mindful eating practices, and paying attention to hunger and fullness cues can significantly impact calorie intake.
Importance of Regular Physical Activity in Weight Management
Regular physical activity is essential for weight management. It not only helps burn calories but also improves overall health and well-being. Different types of physical activity offer varying benefits, and finding activities that are enjoyable and sustainable is key to long-term adherence.
- Cardiovascular Exercise: Cardiovascular exercises, such as running, swimming, or cycling, are highly effective for calorie burning and improving cardiovascular health. Consistency is key to achieving and maintaining fitness levels.
- Strength Training: Strength training exercises, such as weightlifting or bodyweight exercises, are important for building muscle mass. Muscle tissue burns more calories at rest, which can contribute to weight loss.
- Flexibility and Balance Exercises: Incorporating flexibility and balance exercises, such as yoga or Pilates, can improve posture, reduce risk of injury, and enhance overall well-being.
Use of Pharmaceutical Interventions in Treating Obesity
Pharmaceutical interventions can be considered as part of a comprehensive obesity management plan. They are not a substitute for lifestyle modifications but can be used in conjunction to enhance weight loss efforts. However, their use should be carefully considered and guided by a healthcare professional.
- Prescription Medications: Some medications can help suppress appetite, increase metabolism, or reduce fat absorption. However, these medications should only be used under the supervision of a physician.
- Medical Supervision: Individuals considering pharmaceutical interventions should discuss the potential benefits and risks with their physician. Regular monitoring is crucial to ensure safety and effectiveness.
Summary Table of Obesity Management Approaches
| Approach | Focus | Considerations | Examples |
|---|---|---|---|
| Lifestyle Modifications | Dietary changes, physical activity, stress management | Individual needs, cultural context, sustainability | Balanced diet, regular exercise, stress-reducing activities |
| Dietary Interventions | Calorie control, nutrient-dense foods, portion control | Individual calorie needs, food preferences, cultural factors | Portion control, mindful eating, increased fruit/vegetable intake |
| Physical Activity | Cardiovascular exercise, strength training, flexibility | Individual preferences, safety considerations, gradual increase | Walking, running, swimming, strength training |
| Pharmaceutical Interventions | Appetite suppression, increased metabolism | Medical supervision, potential side effects, long-term use | Prescription medications, regular monitoring |
Illustrative Case Studies
Understanding the complexities of obesity requires looking at real-world examples. These case studies, while anonymized for privacy, offer valuable insights into the diverse factors influencing obesity, from genetics and environment to individual choices and medical histories. They highlight the importance of personalized treatment plans and the unique challenges faced by each individual.Analyzing case studies helps us understand the nuances of obesity management.
They reveal how different types of obesity can manifest, emphasizing the need for tailored interventions and support systems. The diverse experiences of these individuals provide a framework for developing more effective strategies for prevention and treatment.
Case Study 1: Andrew – Hyperphagia-Associated Obesity
Andrew, a 35-year-old male, presented with a history of significant weight gain over the past 10 years. He reported experiencing episodes of uncontrollable hunger, known as hyperphagia, particularly after stressful events. His medical history included anxiety and depression, conditions often associated with altered eating behaviors. Initial assessments revealed a BMI of 42, placing him in the severely obese category.
His treatment plan included cognitive behavioral therapy (CBT) to address his anxiety and coping mechanisms related to eating. Dietary counseling focused on portion control and mindful eating, while medication to regulate appetite was considered, along with regular exercise. Andrew’s progress was slow, but consistent with support, and he successfully managed his weight with a multidisciplinary approach. He learned to identify and manage his triggers for overeating, and to develop healthier coping mechanisms.
Case Study 2: Maria – Visceral Obesity
Maria, a 50-year-old female, presented with a significant increase in waist circumference. Her medical history included a sedentary lifestyle and a family history of cardiovascular disease. Assessments revealed a BMI of 38 and elevated blood pressure and cholesterol levels. Her treatment focused on lifestyle modifications, including regular aerobic exercise and a balanced diet. Dietary guidance emphasized reducing saturated fats and refined carbohydrates, while increasing fruits, vegetables, and lean protein.
Medication was also prescribed to manage blood pressure and cholesterol levels. Maria faced the challenge of making long-term lifestyle changes, requiring significant motivation and support. She struggled with social factors, such as limited access to healthy food options in her community. Her treatment plan incorporated community resources to address these barriers and promote long-term success.
Case Study 3: David – Subcutaneous Obesity
David, a 22-year-old male, presented with a BMI of 30, primarily characterized by an accumulation of fat under the skin. He had a history of poor dietary habits and a sedentary lifestyle, worsened by frequent fast-food consumption and limited physical activity. His treatment focused on comprehensive lifestyle modifications. Nutritional counseling addressed caloric intake and portion sizes, emphasizing whole foods.
He participated in a structured exercise program, focusing on cardiovascular activities and strength training. David’s primary challenge was establishing consistent healthy habits. His treatment plan emphasized creating a sustainable routine and making healthy choices convenient.
Summary Table of Illustrative Case Studies
| Case Study | Type of Obesity | Key Features | Medical History | Treatment Plan | Challenges |
|---|---|---|---|---|---|
| Andrew | Hyperphagia-Associated | Uncontrolled hunger, anxiety | Anxiety, depression, 10 years of significant weight gain | CBT, dietary counseling, potential medication | Managing triggers, establishing long-term habits |
| Maria | Visceral | Increased waist circumference | Sedentary lifestyle, family history of CVD, elevated blood pressure & cholesterol | Lifestyle modifications, exercise, balanced diet, medication | Long-term lifestyle changes, community resources |
| David | Subcutaneous | Fat accumulation under the skin | Poor dietary habits, sedentary lifestyle, frequent fast food consumption | Nutritional counseling, structured exercise program | Establishing consistent healthy habits |
Illustrative Images/Visualizations
Visual representations play a crucial role in understanding the complexities of obesity. Medical imaging techniques and standardized charts offer valuable insights into the distribution and severity of fat accumulation, which is essential for accurate diagnosis and personalized treatment strategies. These visualizations allow healthcare professionals and individuals to better comprehend the underlying causes and potential health risks associated with various obesity types.
Visceral Fat Accumulation in Medical Imaging
Medical imaging, such as CT scans and MRI, reveals the accumulation of visceral fat, which is located deep within the abdominal cavity, surrounding organs like the liver and intestines. Visually, this fat appears as a dense, slightly heterogeneous structure in the abdominal region. The extent of this fat accumulation can be quantified by measuring the cross-sectional area of the fat deposits.
Higher amounts of visceral fat are often associated with an increased risk of metabolic complications.
Subcutaneous Fat Distribution
Subcutaneous fat, located directly beneath the skin, is typically visible as a less dense, more diffuse structure in medical images compared to visceral fat. Its distribution can vary significantly across different individuals and body regions. While not as directly associated with metabolic complications as visceral fat, excessive subcutaneous fat can still contribute to overall weight and body composition, and potentially increase risk factors.
In medical imaging, subcutaneous fat appears as a less dense structure surrounding muscle and bone, and its distribution can be visualized and quantified in cross-sectional images.
BMI Charts and Interpretation
BMI charts provide a standardized method for assessing body weight relative to height. These charts plot BMI values against different height categories, allowing for the determination of a person’s BMI status. Different colors or shading are often used to represent various BMI categories (underweight, healthy weight, overweight, obese). Understanding the BMI chart and the corresponding interpretation of the BMI category is critical for understanding overall health risks.
A crucial aspect is recognizing that BMI alone doesn’t fully capture body composition, and other imaging techniques are often used in conjunction with BMI to provide a more comprehensive assessment.
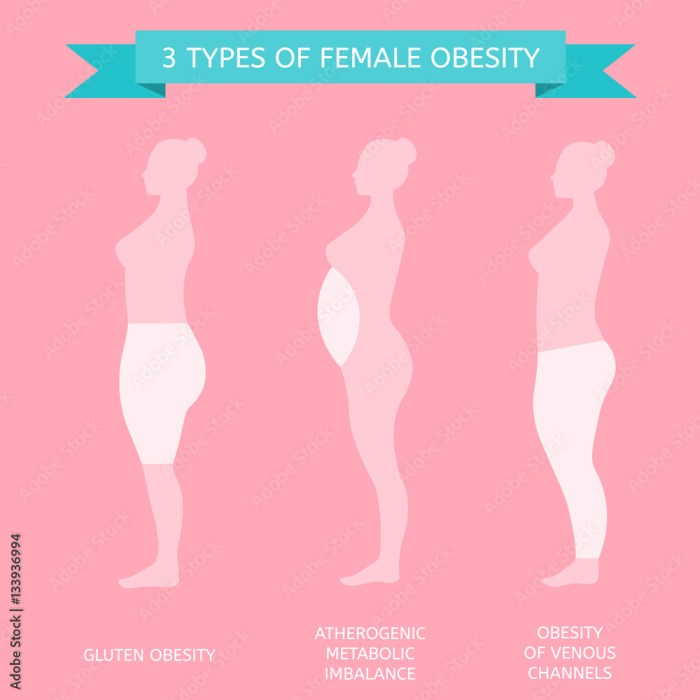
Types of Fat Distribution
Different types of obesity are characterized by varying patterns of fat distribution. These patterns are often visualized using medical imaging techniques.
- Android Obesity (Apple Shape): This type is characterized by an accumulation of visceral fat primarily in the abdominal region, giving the body an apple-like shape. Medical imaging, such as CT scans, clearly shows the increased density of fat in the abdominal area. This distribution is strongly linked to increased risk of cardiovascular disease and type 2 diabetes.
- Gynoid Obesity (Pear Shape): This type is primarily characterized by fat accumulation in the hips and thighs, giving the body a pear-like shape. Medical imaging demonstrates less pronounced visceral fat accumulation compared to android obesity. While not as directly associated with metabolic complications as android obesity, excess fat in this region can still contribute to overall health risks.
End of Discussion: Different Types Of Obesity
In conclusion, different types of obesity are not a single entity but a spectrum of conditions influenced by a multitude of factors. This discussion has highlighted the diverse aspects, from genetic predispositions and environmental influences to the associated health risks and management strategies. Understanding the intricacies of each type is crucial for effective prevention and treatment, emphasizing the importance of personalized approaches and comprehensive care.
Further research and awareness are essential for developing better solutions to address the challenges posed by this complex health issue.










