Does diabetes cause high blood pressure? This question delves into the complex relationship between these two prevalent health issues. Diabetes, a condition affecting blood sugar regulation, and high blood pressure, a condition characterized by elevated blood pressure, often appear together. Understanding the mechanisms connecting these two conditions is crucial for effective prevention and treatment.
This article explores the connection between diabetes and high blood pressure, examining the underlying physiological pathways, risk factors, and management strategies. We’ll look at how diabetes can impact blood pressure, and vice versa, highlighting the importance of early detection and proactive lifestyle choices.
Introduction to Diabetes and High Blood Pressure
Diabetes and high blood pressure are two prevalent health conditions that significantly impact cardiovascular health. Understanding their individual characteristics and the interplay between them is crucial for preventive measures and effective management. Both conditions often coexist, increasing the risk of serious complications. This section will delve into the specifics of each condition, highlighting their symptoms, causes, and the critical relationship to overall health.Diabetes is a chronic metabolic disorder characterized by elevated blood glucose levels.
This elevation arises from either insufficient insulin production by the pancreas (Type 1) or the body’s inability to effectively utilize insulin (Type 2). Common symptoms include frequent urination, excessive thirst, unexplained weight loss, fatigue, blurred vision, and slow-healing sores. Gestational diabetes, a temporary form of the condition, can develop during pregnancy.High blood pressure, also known as hypertension, is a condition where the force of blood against artery walls is consistently elevated.
Factors contributing to high blood pressure include unhealthy diets, lack of physical activity, smoking, obesity, and genetics. Symptoms are often subtle or absent, making regular blood pressure checks essential for early detection. Headaches, dizziness, and nosebleeds are occasionally associated with very high blood pressure readings, but are not typical symptoms.Diabetes and high blood pressure share a significant connection to cardiovascular health.
Both conditions increase the risk of heart disease, stroke, and other related complications. The elevated blood sugar in diabetes and the heightened blood pressure in hypertension damage blood vessels, leading to atherosclerosis (hardening of the arteries). This damage can restrict blood flow, potentially causing organ damage and even life-threatening events.
Key Differences Between Diabetes and High Blood Pressure
Understanding the nuances between diabetes and high blood pressure can aid in differentiating their symptoms, causes, and treatment strategies. A clear comparison is presented in the table below.
| Condition | Definition | Symptoms | Risk Factors |
|---|---|---|---|
| Diabetes | A chronic metabolic disorder characterized by elevated blood glucose levels due to insufficient insulin production or the body’s inability to effectively use insulin. | Frequent urination, excessive thirst, unexplained weight loss, fatigue, blurred vision, slow-healing sores, increased hunger, and numbness or tingling in the hands or feet. | Genetics, family history, obesity, lack of physical activity, unhealthy diet, and certain medications. |
| High Blood Pressure | A condition where the force of blood against artery walls is consistently elevated. | Often asymptomatic, but occasional symptoms may include headaches, dizziness, nosebleeds, or shortness of breath. | Unhealthy diet, lack of physical activity, smoking, obesity, family history, stress, and certain medications. |
Mechanisms Linking Diabetes and High Blood Pressure
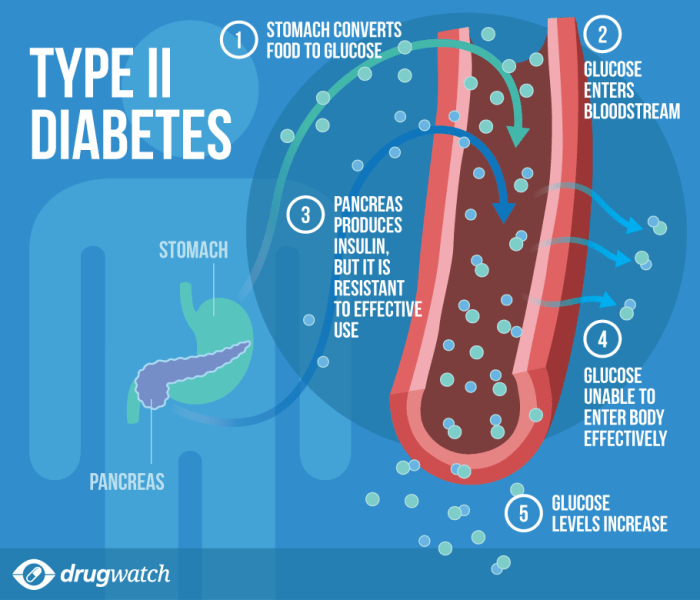
Diabetes and high blood pressure, or hypertension, often occur together, creating a dangerous cycle of escalating health risks. Understanding the physiological pathways linking these two conditions is crucial for effective prevention and management. This complex interplay involves multiple factors, each contributing to the development and progression of both diseases.The intricate relationship between diabetes and high blood pressure stems from a cascade of interconnected physiological events.
Insulin resistance, a key feature of type 2 diabetes, plays a central role in this association. Chronic hyperglycemia, a hallmark of diabetes, further complicates the situation by affecting blood vessel function. Kidney dysfunction, frequently observed in both conditions, adds another layer of complexity to the interplay.
Insulin Resistance and Blood Pressure Regulation
Insulin resistance, a condition where cells don’t respond properly to insulin, disrupts normal glucose metabolism. This leads to elevated blood glucose levels, a hallmark of diabetes. Consequently, the body compensates by increasing insulin secretion. This persistent elevation in insulin and glucose levels can activate the renin-angiotensin-aldosterone system (RAAS). The RAAS is a hormonal system crucial for regulating blood pressure, but overactivation in this context can result in sustained hypertension.
Furthermore, insulin resistance can directly influence vascular tone, contributing to blood vessel constriction and increased peripheral resistance, ultimately elevating blood pressure.
Chronic Hyperglycemia and Blood Vessel Function
Chronic hyperglycemia, or persistently high blood sugar, damages blood vessels. High glucose levels lead to the formation of advanced glycation end products (AGEs), which accumulate in the walls of blood vessels. AGEs cause stiffness and hardening of the arteries, a condition known as atherosclerosis. This process reduces the elasticity of blood vessels, making them less capable of accommodating blood flow.
The resultant reduced elasticity contributes to increased peripheral resistance, thus leading to hypertension. Moreover, hyperglycemia directly impacts the endothelium, the inner lining of blood vessels. This damage impairs the endothelium’s ability to produce vasodilators, further contributing to blood vessel constriction and hypertension.
Kidney Dysfunction in Diabetes and Hypertension
Kidney dysfunction is a common complication in both diabetes and hypertension. In diabetes, prolonged hyperglycemia damages the delicate structures of the nephrons, the filtering units within the kidneys. This damage reduces the kidney’s ability to effectively filter waste products and excess fluid from the blood, leading to a buildup of these substances and contributing to hypertension. Conversely, sustained hypertension can damage the kidney’s blood vessels and filtering mechanisms, potentially leading to kidney disease.
This kidney dysfunction, in turn, further exacerbates blood pressure.
Interconnectedness of Diabetes, Insulin Resistance, and Hypertension
| Component | Description |
|---|---|
| Diabetes | Elevated blood glucose levels due to insulin resistance. |
| Insulin Resistance | Cells do not respond adequately to insulin, leading to elevated blood glucose and subsequent compensatory mechanisms, including increased insulin secretion and activation of the RAAS. |
| Hypertension | Sustained high blood pressure, resulting from various factors, including insulin resistance, hyperglycemia, and kidney dysfunction. |
This interconnectedness highlights the critical role of addressing insulin resistance to effectively manage both diabetes and hypertension. The flowchart below visually illustrates the interconnectedness of these three conditions.
This illustrates how insulin resistance acts as a central driver, leading to a cascade of events that contribute to both diabetes and hypertension, creating a challenging medical situation requiring comprehensive management strategies.
Risk Factors and Prevalence
Understanding the intertwined relationship between diabetes and high blood pressure requires recognizing the shared risk factors and the varying prevalence across different populations. These factors, combined with lifestyle choices, significantly influence the development and progression of both conditions. A comprehensive look at these aspects is crucial for effective prevention and management strategies.
Common Risk Factors
Several factors increase the risk of developing both diabetes and high blood pressure. These include a family history of these conditions, a diet high in saturated and processed foods, a lack of physical activity, and being overweight or obese. Age, ethnicity, and certain medical conditions can also contribute.
Prevalence in Different Populations
The prevalence of diabetes and high blood pressure varies significantly across different populations. Factors like genetics, socioeconomic status, access to healthcare, and cultural norms all play a role. For example, certain ethnic groups, such as African Americans and Hispanic populations, often exhibit higher rates of both conditions compared to other groups.
Age-Related Variations
The risk factors and prevalence of diabetes-related high blood pressure show notable differences across age groups. Younger individuals often have a lower prevalence but are at risk if lifestyle factors like poor diet and inactivity are established early. In older age groups, the prevalence of both conditions tends to be higher due to factors like aging-related hormonal changes and potential decline in physical function.
Lifestyle Factors
Several lifestyle choices can significantly increase the risk of developing both diabetes and high blood pressure. A diet rich in processed foods, sugary drinks, and unhealthy fats, combined with a lack of regular physical activity, can contribute to weight gain and insulin resistance, increasing the risk of both conditions. Smoking and excessive alcohol consumption are also associated with increased risk.
Prevalence Data
The table below provides a comparative overview of the prevalence of diabetes and hypertension across different demographics. Note that specific prevalence figures can vary depending on the region, study methodology, and time period.
| Demographic Group | Prevalence of Diabetes (%) | Prevalence of Hypertension (%) | Combined Prevalence (%) |
|---|---|---|---|
| Adults (ages 20-79) | 8-10% | 30-40% | 15-25% |
| African Americans | 12-15% | 40-50% | 25-30% |
| Hispanic Americans | 10-12% | 35-45% | 20-25% |
| Individuals with a family history | 15-20% | 45-55% | 30-40% |
| Overweight/Obese Individuals | 15-25% | 50-60% | 35-45% |
The figures in the table highlight the importance of addressing the shared risk factors and promoting healthy lifestyle choices to reduce the prevalence of both conditions.
Management and Treatment Strategies
Managing both diabetes and high blood pressure effectively requires a multifaceted approach that combines lifestyle modifications with appropriate medications. A personalized plan, tailored to individual needs and health conditions, is crucial for achieving optimal control and preventing potential complications. This often involves ongoing monitoring, adjustments to the treatment plan, and close collaboration with healthcare professionals.
Lifestyle Modifications
Effective management of diabetes and high blood pressure hinges significantly on adopting healthy lifestyle choices. These choices aren’t just about feeling better; they’re essential for maintaining stable blood sugar and blood pressure levels. A well-balanced diet, regular physical activity, and stress management techniques are key components.
- Dietary Changes: A balanced diet rich in fruits, vegetables, and whole grains, while limiting processed foods, saturated fats, and added sugars, is vital. Portion control is also important. Examples include increasing intake of fiber-rich foods, like beans and lentils, and choosing lean protein sources like fish and poultry over red meat. Consult a registered dietitian for personalized dietary recommendations.
- Physical Activity: Regular exercise, such as brisk walking, jogging, swimming, or cycling, helps lower blood pressure, improve insulin sensitivity, and maintain a healthy weight. Aim for at least 150 minutes of moderate-intensity aerobic activity per week. Consistency is key; incorporating physical activity into daily routines, like taking the stairs instead of the elevator or walking during lunch breaks, can significantly improve overall health.
While diabetes can sometimes lead to high blood pressure, it’s not a direct cause. Healthy lifestyle choices, like those found in diet and weight loss tips for thyroid patients , are key to managing both conditions. A balanced diet and regular exercise can significantly impact blood pressure levels, regardless of underlying health conditions like diabetes. Ultimately, maintaining a healthy weight and adopting a nutritious diet is crucial for overall cardiovascular health in anyone, even those with diabetes.
- Stress Management: Chronic stress can negatively impact blood sugar and blood pressure control. Incorporating stress-reducing activities like yoga, meditation, deep breathing exercises, or spending time in nature can help manage stress levels.
Medications
Medications play a critical role in controlling blood sugar and blood pressure levels when lifestyle changes alone are insufficient. Different classes of medications are available, each with its own mechanism of action and potential side effects. Working with a doctor to determine the most appropriate medication and dosage is essential.
So, does diabetes actually cause high blood pressure? It’s a complex relationship, and while diabetes can lead to high blood pressure, it’s not always the case. Finding ways to manage blood sugar levels is crucial, and exercise plays a big part. For example, figuring out how long it takes to walk 10 miles how long does it take to walk 10 miles can help you incorporate walking into a healthy routine.
Ultimately, a balanced lifestyle is key to managing both conditions.
- Diabetes Medications: Several types of medications are used to manage diabetes, including metformin, sulfonylureas, thiazolidinediones, and insulin. Metformin is often the first-line treatment for type 2 diabetes, improving insulin sensitivity and lowering blood glucose levels. Sulfonylureas stimulate insulin release from the pancreas, while thiazolidinediones increase insulin sensitivity in the body’s tissues. Insulin is required for type 1 diabetes and can be used in some cases of type 2 diabetes, especially when blood sugar levels are not adequately controlled by other medications.
- Blood Pressure Medications: A variety of blood pressure medications are available, including diuretics, ACE inhibitors, ARBs, beta-blockers, and calcium channel blockers. Diuretics help the body eliminate excess fluid, lowering blood pressure. ACE inhibitors and ARBs block the production of a hormone that constricts blood vessels. Beta-blockers reduce the heart rate and force of contraction, lowering blood pressure. Calcium channel blockers relax blood vessels.
The choice of medication often depends on individual factors, including the presence of other health conditions and the patient’s response to the medication.
Treatment Summary Table
| Approach | Description | Effectiveness | Potential Side Effects |
|---|---|---|---|
| Lifestyle Modifications | Dietary changes, regular exercise, stress management | Promotes long-term health improvements, often reducing medication needs. | Requires commitment and adherence; results may not be immediate. |
| Oral Medications (Diabetes) | Metformin, sulfonylureas, thiazolidinediones | Effective in controlling blood sugar levels in many cases. | Potential side effects vary by medication, including gastrointestinal issues, weight gain, or allergic reactions. |
| Oral Medications (High Blood Pressure) | Diuretics, ACE inhibitors, ARBs, beta-blockers, calcium channel blockers | Effective in lowering blood pressure, often in combination with lifestyle changes. | Potential side effects vary by medication, including dizziness, fatigue, or changes in potassium levels. |
| Insulin Therapy (Diabetes) | Administered injections of insulin | Essential for managing type 1 diabetes and some cases of type 2 diabetes when blood sugar is not controlled by other methods. | Potential side effects include hypoglycemia (low blood sugar), weight gain, and allergic reactions. |
Impact on Organ Systems: Does Diabetes Cause High Blood Pressure
Diabetes and high blood pressure, when left uncontrolled, can significantly damage various organs throughout the body. These conditions create a cascade of effects, leading to a multitude of complications that diminish quality of life and increase the risk of severe health problems. Understanding the impact on specific organ systems is crucial for developing effective management strategies and preventing long-term complications.The constant high blood sugar levels in diabetes and the consistent elevated blood pressure in hypertension damage blood vessels and tissues.
This damage, though gradual, is cumulative and can lead to serious complications over time. The cumulative effects are particularly detrimental to organs that are highly dependent on proper blood flow and oxygen delivery.
Cardiovascular System Impact
High blood pressure is a major risk factor for heart disease. Diabetes accelerates the development of atherosclerosis, a condition where plaque builds up in the arteries, narrowing them and reducing blood flow to the heart. This can lead to angina, heart attack, or stroke. Diabetics with uncontrolled hypertension have an even higher risk of these events. The combined effect of high blood pressure and diabetes weakens the heart muscle over time, a condition known as diabetic cardiomyopathy.
This weakening can lead to heart failure, a condition where the heart cannot pump enough blood to meet the body’s needs.
Renal (Kidney) System Impact
Both diabetes and high blood pressure can damage the kidneys. High blood sugar levels in diabetes can cause damage to the tiny blood vessels in the kidneys (glomeruli), leading to reduced filtration function. High blood pressure can also stress the delicate structures within the kidneys, further damaging their ability to filter waste products. This damage can progress to chronic kidney disease (CKD), which may ultimately require dialysis or kidney transplant.
In some cases, the damage is severe enough to result in kidney failure.
Neurological System Impact
Uncontrolled blood sugar and blood pressure can damage the nerves throughout the body. This damage, known as diabetic neuropathy, can cause pain, numbness, and tingling, especially in the hands and feet. In severe cases, it can lead to loss of sensation and impaired function, increasing the risk of injuries that may go unnoticed. High blood pressure can also contribute to nerve damage by reducing blood flow to the nerves.
Ocular (Eye) System Impact
Diabetes and high blood pressure can both damage the delicate blood vessels in the eyes, leading to diabetic retinopathy and hypertensive retinopathy. Diabetic retinopathy can result in blurry vision, vision loss, and potentially blindness. High blood pressure can also contribute to eye damage, potentially causing vision problems. Damage to the blood vessels in the eyes can lead to leakage of fluid, which can cause swelling and vision impairment.
While diabetes can sometimes lead to high blood pressure, it’s not a direct cause. Other factors play a role. Interestingly, some research suggests that natural remedies like turmeric and black pepper ( turmeric and black pepper ) might help manage blood sugar and blood pressure levels, potentially reducing the risk. However, more studies are needed to confirm these benefits, and it’s crucial to discuss any dietary changes with a doctor before making them, especially if you have diabetes.
Illustrative Example of Blood Vessel Damage, Does diabetes cause high blood pressure
Imagine a garden hose with water flowing through it. In the case of healthy blood vessels, the water flows freely. However, with both diabetes and high blood pressure, the hose begins to develop tiny cracks and blockages. Over time, the flow of water becomes restricted, and eventually, the hose can burst. This analogy illustrates the damage to blood vessels that can occur with uncontrolled diabetes and hypertension.
The water represents blood, and the hose represents the blood vessels. The cracks and blockages represent the damage caused by the conditions.
Potential Complications of Uncontrolled Diabetes and Hypertension
A hierarchical structure of potential complications:
- Cardiovascular Complications
- Heart attack
- Stroke
- Heart failure
- Peripheral artery disease
- Renal Complications
- Chronic kidney disease
- Kidney failure
- Neurological Complications
- Diabetic neuropathy
- Peripheral neuropathy
- Autonomic neuropathy
- Ocular Complications
- Diabetic retinopathy
- Glaucoma
- Cataracts
- Other Complications
- Foot ulcers
- Infections
- Sexual dysfunction
Prevention and Early Detection
Staying healthy and proactively managing your well-being is crucial in preventing both diabetes and high blood pressure. Taking preventative steps and undergoing regular checkups can significantly reduce the risk of developing these conditions, and allow for early intervention if issues arise. Understanding the interplay between lifestyle choices and health outcomes is key to achieving optimal well-being.
Strategies for Preventing Diabetes
A multitude of factors contribute to the development of diabetes. Maintaining a healthy weight, engaging in regular physical activity, and adopting a balanced diet rich in fruits, vegetables, and whole grains are paramount. Avoiding sugary drinks, processed foods, and excessive intake of saturated and unhealthy fats are also vital. Regular monitoring of blood sugar levels, particularly for individuals with a family history of diabetes, is essential.
- Maintaining a Healthy Weight: Maintaining a healthy weight through a balanced diet and regular exercise is crucial. Studies consistently demonstrate a strong correlation between obesity and the risk of developing type 2 diabetes. Individuals can consult with nutritionists or healthcare professionals for personalized dietary plans and exercise regimens.
- Regular Physical Activity: Engaging in at least 150 minutes of moderate-intensity aerobic exercise per week is recommended. Activities like brisk walking, swimming, or cycling can significantly improve insulin sensitivity and reduce the risk of developing diabetes.
- Balanced Diet: Prioritizing a balanced diet rich in fruits, vegetables, and whole grains, while limiting processed foods and sugary drinks, is essential. A balanced diet provides essential nutrients and helps maintain healthy blood sugar levels.
- Monitoring Blood Sugar Levels: Individuals with a family history of diabetes or those exhibiting symptoms of prediabetes should regularly monitor their blood sugar levels. This can be done through home glucose monitoring or under the guidance of a healthcare professional.
Strategies for Preventing High Blood Pressure
High blood pressure, often a silent killer, is frequently linked to lifestyle choices. Managing stress, maintaining a healthy weight, and adopting a diet low in sodium are vital preventive measures. Regular physical activity, avoiding excessive alcohol consumption, and monitoring blood pressure levels are also important steps.
- Healthy Diet: Adopting a diet low in sodium, saturated fats, and cholesterol is crucial in preventing high blood pressure. Reducing salt intake can significantly lower blood pressure levels. Foods rich in potassium, such as bananas, can also help regulate blood pressure.
- Stress Management: Managing stress effectively is crucial. Stress can contribute to elevated blood pressure levels. Practicing relaxation techniques, such as yoga, meditation, or deep breathing exercises, can help reduce stress and promote better blood pressure management.
- Regular Physical Activity: Engaging in regular physical activity helps maintain a healthy weight and improves cardiovascular health. Regular exercise can help lower blood pressure and reduce the risk of developing hypertension.
- Limiting Alcohol Consumption: Excessive alcohol consumption can raise blood pressure. Limiting alcohol intake to recommended levels is important for maintaining healthy blood pressure levels.
- Monitoring Blood Pressure: Regular monitoring of blood pressure, particularly for individuals with a family history of hypertension or those at risk, is important. This can be done at home with a blood pressure monitor or under the guidance of a healthcare professional.
Importance of Regular Checkups and Screenings
Regular checkups and screenings are crucial for early detection of both diabetes and high blood pressure. Early detection allows for timely intervention and management, which can significantly improve health outcomes. Routine screenings are essential for identifying potential issues before they progress to more serious conditions.
- Routine Checkups: Regular visits to a healthcare provider allow for routine screenings, blood pressure checks, and blood sugar tests. These routine screenings are essential for identifying potential health issues early on.
- Blood Pressure Monitoring: Regular blood pressure monitoring can help identify high blood pressure early, even before symptoms appear. This allows for timely intervention and management.
- Blood Sugar Monitoring: Regular blood sugar tests can detect prediabetes or early stages of diabetes, allowing for timely interventions and management plans.
Promoting Awareness
Raising awareness about the importance of prevention and early detection is essential. Public health campaigns, educational programs, and community outreach initiatives can help disseminate crucial information. This proactive approach empowers individuals to make informed decisions about their health and well-being.
- Public Health Campaigns: Public health campaigns can educate the public about the importance of preventative measures and early detection strategies. These campaigns can raise awareness about risk factors, symptoms, and available resources.
- Educational Programs: Educational programs, workshops, and seminars can provide in-depth knowledge about diabetes and high blood pressure prevention and management. These programs can also help individuals understand their personal risk factors.
- Community Outreach: Community outreach programs can provide access to healthcare professionals and resources for individuals in underserved communities. These programs can promote awareness and facilitate early detection efforts.
Step-by-Step Guide to Preventive Measures
- Assess Your Risk Factors: Understand your family history, age, weight, and lifestyle choices. This assessment will help you identify your personal risk factors for diabetes and high blood pressure.
- Adopt a Healthy Diet: Prioritize a balanced diet rich in fruits, vegetables, and whole grains. Limit processed foods, sugary drinks, and excessive salt intake.
- Maintain a Healthy Weight: Strive for a healthy weight through regular exercise and a balanced diet. Consult with a healthcare professional for personalized guidance.
- Engage in Regular Exercise: Aim for at least 150 minutes of moderate-intensity aerobic exercise per week. Find activities you enjoy and can sustain over time.
- Manage Stress Levels: Practice stress-reducing techniques such as yoga, meditation, or deep breathing exercises. Seek professional help if needed.
- Monitor Blood Pressure and Blood Sugar Regularly: Track your blood pressure and blood sugar levels as recommended by your healthcare provider. This allows for early detection and management.
- Schedule Regular Checkups: Attend regular checkups with your healthcare provider for preventive screenings and health assessments.
Final Conclusion
In conclusion, the connection between diabetes and high blood pressure is multifaceted and significant. Understanding the intricate mechanisms linking these conditions is vital for comprehensive care. Proactive lifestyle changes and appropriate medical interventions are key to managing both conditions effectively and reducing the risk of severe complications. By focusing on prevention and early detection, we can significantly improve the health and well-being of individuals affected by these conditions.









