How often should i takegive pain medications – How often should I take pain medications? This is a crucial question for anyone experiencing pain, from a simple headache to chronic conditions. Understanding the types of pain relievers, their potential side effects, and the factors influencing dosage is key to managing pain safely and effectively. This guide will delve into the science behind pain medication use, exploring different pain conditions, and offering insights into optimal frequencies and safe usage.
From over-the-counter options to prescription drugs, we’ll explore the effectiveness and potential risks of various pain relief methods. We’ll also discuss the importance of personalized pain management plans and the role of a healthcare professional in guiding your treatment. Knowing how to assess pain severity, monitor your response to medication, and adjust your regimen is essential for optimal results.
Understanding Pain Medication Use
Pain is a common human experience, and managing it effectively is crucial for overall well-being. Understanding the different types of pain medications, their potential side effects, and the factors influencing dosage can empower individuals to make informed decisions about their pain management. This exploration will delve into the world of pain relief, providing a comprehensive overview of available options.Effective pain management often involves a multi-faceted approach, recognizing that different types of pain respond differently to various medications.
Choosing the right medication and dosage is essential to achieve relief without adverse effects. This includes considering the specific pain condition, individual sensitivities, and potential interactions with other medications.
Types of Pain Medications
Different pain medications cater to various needs and conditions. Understanding their distinctions is key to selecting the most suitable option. Over-the-counter (OTC) medications, readily available without a prescription, often address mild to moderate pain. Prescription medications, on the other hand, are typically used for more severe or persistent pain conditions.
- Over-the-Counter (OTC) Medications: These medications are generally safe for short-term use and mild pain. Common examples include ibuprofen (Advil, Motrin), acetaminophen (Tylenol), and naproxen (Aleve). These are often effective for headaches, muscle aches, and minor injuries. OTC medications typically have a lower risk of serious side effects compared to prescription medications, but still require caution and adherence to recommended dosages.
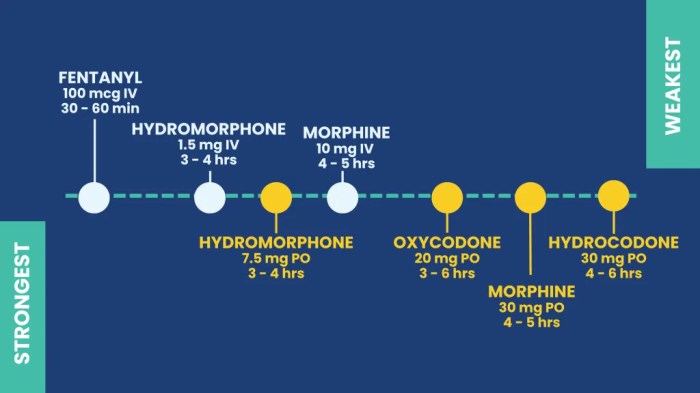
- Prescription Medications: These medications are stronger and often used for chronic or severe pain conditions. Examples include opioids (morphine, oxycodone), nonsteroidal anti-inflammatory drugs (NSAIDs), and certain antidepressants or anticonvulsants. Prescription medications must be taken under the supervision of a healthcare professional to ensure safety and efficacy. The potential for side effects and dependence is higher with prescription medications.
Common Pain Conditions
Pain can arise from various sources, influencing the choice of medication. Identifying the cause and nature of the pain is essential for appropriate treatment.
- Headaches: Tension headaches, migraines, and cluster headaches are common causes of head pain. OTC pain relievers like ibuprofen or acetaminophen are often sufficient for tension headaches. Migraines and cluster headaches may require stronger medications, potentially prescription-strength, based on severity.
- Arthritis: Conditions like osteoarthritis and rheumatoid arthritis cause joint pain and inflammation. NSAIDs, both OTC and prescription, are often used to manage the pain and inflammation associated with these conditions.
- Muscle Strains and Sprains: Injuries to muscles or ligaments can cause significant pain and discomfort. OTC NSAIDs are commonly used to reduce inflammation and alleviate pain. In severe cases, prescription pain relievers may be necessary.
Effectiveness and Side Effects
The effectiveness and potential side effects of pain medications vary. Factors like individual responses, medication interactions, and dosage play crucial roles.
- Effectiveness: The effectiveness of a pain medication depends on various factors including the individual’s tolerance, the type of pain, and the severity of the condition. Some individuals may find OTC medications sufficient for mild pain, while others may require prescription-strength medication.
- Side Effects: Side effects can range from mild, like stomach upset, to severe, such as allergic reactions or organ damage. It’s crucial to be aware of potential side effects and to discuss them with a healthcare provider. The risk of side effects increases with stronger medications and higher dosages.
Factors Influencing Dosage
Determining the appropriate dosage of pain medication is a crucial aspect of safe and effective pain management. Several factors influence the recommended dosage.
- Individual Factors: Weight, age, and overall health status influence the optimal dosage of pain medication. Individuals with pre-existing health conditions may require adjustments in dosage or different medications entirely.
- Type of Pain: The nature and severity of the pain condition dictate the appropriate dosage. Mild aches may respond well to smaller doses, whereas severe pain may necessitate higher doses or different medications.
- Medication Interactions: Certain medications can interact with other medications, leading to potential side effects or reduced effectiveness. It’s essential to inform a healthcare provider about all medications being taken to avoid any harmful interactions.
Determining Frequency of Use
Knowing how often to take pain medication is crucial for effective pain management and minimizing potential side effects. This section will delve into assessing pain severity and duration, monitoring your response to medication, and providing practical schedules for various pain levels. Understanding these factors empowers you to take control of your pain relief journey.Pain management is a personalized process.
There’s no one-size-fits-all solution. Factors like the type of pain, individual response to medication, and underlying medical conditions all influence optimal medication frequency. This section will provide guidance to help you tailor your pain management strategy to your specific needs.
Assessing Pain Severity and Duration
Accurate assessment of pain is fundamental to determining the appropriate medication frequency. Consider both the intensity and duration of the pain when evaluating its severity. Pain intensity can be graded using a pain scale, such as the 0-10 numerical rating scale. A score of 0 indicates no pain, and a score of 10 represents the worst imaginable pain.
Pain duration refers to how long the pain has lasted. This information helps in understanding the potential cause and severity of the pain.
Monitoring Pain Response to Medication
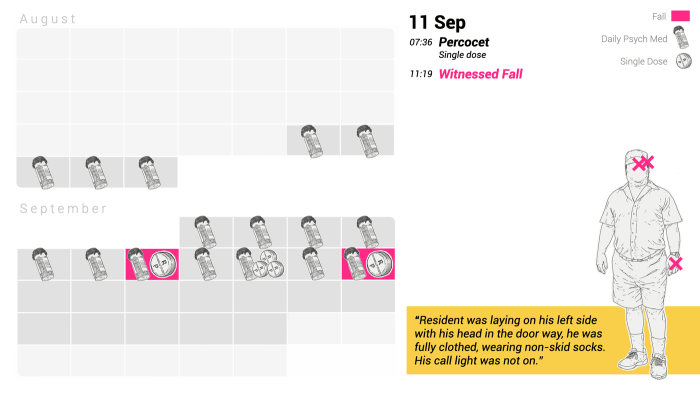
Closely monitoring your pain response is vital for adjusting medication frequency and dosage. Pay attention to how effectively the medication alleviates your pain. Regularly document your pain levels before and after taking medication using a pain scale. Keep a pain diary to track the onset, peak, and duration of pain, along with the effects of the medication.
Note any side effects experienced. This data helps you and your healthcare provider refine your pain management strategy.
Typical Pain Medication Schedules
The following table provides general guidelines for pain medication schedules based on pain intensity. These are just starting points and should be adjusted based on individual responses.
| Pain Intensity | Typical Schedule (Example) | Important Considerations |
|---|---|---|
| Mild Pain (1-4 on a 0-10 scale) | Take medication as needed, every 4-6 hours, or as directed by your doctor. | Mild pain may respond well to over-the-counter pain relievers. Listen to your body and adjust the frequency accordingly. |
| Moderate Pain (5-7 on a 0-10 scale) | Take medication every 3-4 hours, or as directed by your doctor. | Moderate pain may require stronger pain relievers. It’s essential to adhere to the prescribed dosage and frequency. |
| Severe Pain (8-10 on a 0-10 scale) | Take medication every 1-2 hours, or as directed by your doctor. | Severe pain often warrants immediate medical attention. Follow your doctor’s instructions carefully and consider seeking emergency care if needed. |
Recommended Frequency of Use for Different Pain Medications
Different pain medications have varying half-lives and mechanisms of action, which influence their optimal frequency of use. The following table provides a general comparison, but always consult your doctor for specific recommendations.
| Pain Medication | Typical Frequency | Important Considerations |
|---|---|---|
| Acetaminophen (Tylenol) | Every 4-6 hours as needed | Generally safe for short-term use. Avoid exceeding recommended dosages. |
| Ibuprofen (Advil, Motrin) | Every 4-6 hours as needed | May cause stomach upset. Take with food or as directed by your doctor. |
| Codeine | Every 4-6 hours as needed | Opioid analgesic. Use only as directed by your doctor. Can be habit-forming. |
| Tramadol | Every 4-6 hours as needed | Opioid-like analgesic. Use only as directed by your doctor. Can be habit-forming. |
Safety Considerations
Taking pain medication regularly, even for short periods, carries potential risks. Understanding these risks and how to manage them is crucial for safe and effective pain management. This section will delve into the potential side effects, warning signs, and strategies to prevent overuse. It’s important to remember that individual responses to medication can vary, and consulting with a healthcare professional is always recommended.Frequent pain medication use, while often necessary, can lead to a range of potential side effects.
These effects can range from mild discomfort to serious health concerns. Careful monitoring and awareness of these potential issues are essential for safe medication use.
Potential Risks and Side Effects
Regular use of pain medications can lead to various side effects, including gastrointestinal issues like nausea, vomiting, or ulcers. Kidney problems, liver damage, and allergic reactions are also possible, though less common. Some medications can interact with other medications or supplements, potentially causing harmful side effects. Long-term use may also lead to dependence or tolerance, where higher doses are needed to achieve the same pain relief.
Figuring out how often to take pain meds can be tricky, right? It really depends on the type of pain and the medication. Before you dive into a self-treatment plan, it’s always a good idea to check with your doctor or pharmacist. Understanding your blood pressure is also crucial for overall health, and taking a quick quiz like quiz how much do you know about blood pressure can help you get a better sense of your health.
Ultimately, sticking to your doctor’s recommendations is key for managing pain effectively and safely.
Warning Signs of Medication Interactions or Adverse Reactions
Recognizing the signs of potential medication interactions or adverse reactions is crucial for timely intervention. Symptoms may vary but can include unusual bleeding, skin rashes, swelling, difficulty breathing, or changes in vision or mental state. Any new or worsening symptoms during pain medication use should be reported to a healthcare provider immediately.
- Unusual bleeding: This includes nosebleeds, bleeding gums, or unusual bruising. Such instances may indicate a potential blood-thinning effect of the medication.
- Skin rashes or hives: A sudden rash or hives can be a sign of an allergic reaction. This reaction can be mild or severe, and prompt medical attention is necessary.
- Difficulty breathing or swallowing: These symptoms may indicate a serious allergic reaction or other complications. Seek immediate medical help if you experience these problems.
- Changes in vision or mental state: Some medications can affect cognitive function or vision. Sudden changes in these areas should be evaluated by a healthcare provider.
- Severe or persistent stomach pain: If stomach pain persists or worsens while taking pain medication, it could indicate a more serious condition, such as an ulcer or internal bleeding.
Recognizing and Managing Potential Drug Interactions
Medication interactions can occur when one medication alters the way another works in the body. This can either enhance or diminish the effects of the other medication. For example, combining aspirin with blood thinners can increase the risk of bleeding. Always inform your healthcare provider about all medications, supplements, and herbal remedies you are taking. This will help them assess potential interactions.
Always adhere to the prescribed dosage and frequency for all medications, and never self-treat or alter dosages without consulting a healthcare provider.
Figuring out how often to take pain meds can be tricky, right? It really depends on the severity and type of pain. But, while you’re focusing on pain relief, have you considered incorporating collagen supplements for skin health? Collagen supplements for skin can be a fantastic addition to a healthy lifestyle, supporting skin elasticity and reducing the need for external remedies.
Ultimately, sticking to your doctor’s recommendations for pain medication is key, regardless of other dietary supplements you’re trying.
Strategies to Prevent Medication Overuse
Preventing medication overuse is key to minimizing potential risks. Establishing a pain management plan with your healthcare provider is essential. This plan should consider non-pharmacological methods like physical therapy, lifestyle changes, and alternative therapies, as well as when and how to use medication. Follow the prescribed dosage and frequency meticulously. Avoid taking more medication than recommended, even if the pain persists.
If the pain doesn’t improve or worsens, contact your healthcare provider. Keep a detailed record of your pain levels and the medications you take to better communicate with your healthcare provider.
Individual Considerations
Taking pain medication is a deeply personal journey. What works for one person might not work for another. Factors like age, pre-existing health conditions, and concurrent medications significantly impact how often and how much medication someone needs. This personalized approach is crucial for effective pain management and minimizing potential side effects.
Factors Influencing Pain Medication Frequency
Understanding the individual variations in pain response and medication metabolism is paramount. Different factors can influence how often a person needs to take pain medication. These factors must be considered in a holistic manner.
| Factor | Explanation | Example |
|---|---|---|
| Age | Children and older adults often have different metabolic rates for medications. Their bodies may process drugs more slowly or quickly than adults in their prime. | A child might require a lower dose and less frequent administration of ibuprofen compared to an adult for the same pain. |
| Health Conditions | Existing medical conditions like kidney or liver problems can impact how the body processes medications. Conditions like gastrointestinal issues might make frequent medication use problematic. | Someone with kidney disease may need lower doses and less frequent use of certain pain relievers to avoid complications. |
| Other Medications | Simultaneous use of other medications can interact with pain relievers, altering their effectiveness or increasing the risk of side effects. | Taking blood thinners alongside NSAIDs can increase the risk of bleeding. |
| Individual Pain Tolerance | Pain tolerance varies greatly between individuals. What one person considers mild pain, another might perceive as severe. | A person with a higher pain tolerance might need a larger dose or more frequent administration of medication. |
| Medication Type | Different types of pain relievers have different half-lives and durations of action. | Opioids, for instance, often have a longer duration of action compared to NSAIDs. |
Importance of Professional Consultation
“Adjusting pain medication regimens should always be done under the supervision of a healthcare professional.”
Never attempt to alter your pain medication routine without first consulting your doctor. Self-medication can lead to serious complications, from adverse drug reactions to worsening underlying health conditions. A healthcare professional can assess your individual needs, consider your medical history, and tailor a safe and effective pain management plan.
Personalized Pain Management Plans
A personalized pain management plan is crucial for effective and safe pain relief. This approach considers the individual’s unique circumstances, including their medical history, lifestyle, and pain characteristics. Such plans are not one-size-fits-all solutions; instead, they are meticulously crafted to address the specific needs of each patient. This tailored approach ensures that the most appropriate pain relief strategies are employed, while minimizing the risk of adverse effects.
Comparing Approaches to Chronic Pain Management
Various approaches exist for managing chronic pain, each with its own strengths and weaknesses. These approaches may include, but are not limited to, medication management, physical therapy, behavioral therapies, and alternative therapies. The optimal approach is often determined by the type and severity of pain, the individual’s preferences, and the advice of their healthcare provider. The healthcare provider will be able to guide you through the most suitable approach for your specific circumstances.
Specific Medication Examples
Knowing the recommended frequency of use for different pain medications is crucial for managing pain effectively and safely. Understanding the specific instructions for each medication can prevent potential side effects and ensure optimal pain relief. This section delves into the recommended frequencies for common over-the-counter and prescription pain relievers, highlighting important considerations for children and adults.Over-the-counter (OTC) and prescription pain medications vary significantly in their potency and how the body processes them.
This difference directly impacts how often they should be taken. The maximum daily dosage and frequency recommendations are often established to minimize potential adverse effects and maintain therapeutic blood levels.
Over-the-Counter Pain Relievers
Understanding the recommended frequency of use for over-the-counter pain relievers is essential for safe and effective pain management. Different types of OTC pain relievers have varying mechanisms of action and absorption rates, leading to distinct dosing guidelines.
- Acetaminophen (Tylenol): Generally, a maximum daily dose of 4,000 milligrams is recommended for adults. The recommended frequency is typically every 4 to 6 hours as needed, but never exceeding the maximum daily dose. Always follow the specific instructions on the product label.
- Ibuprofen (Advil, Motrin): The maximum daily dose for adults is typically 3,200 milligrams. The recommended frequency is typically every 4 to 6 hours as needed, but never exceeding the maximum daily dose. Always consult the product label for precise instructions.
- Naproxen (Aleve): The maximum daily dose for adults is typically 1,000 to 1,500 milligrams. The recommended frequency is typically every 8 to 12 hours as needed, but never exceeding the maximum daily dose. Always consult the product label for precise instructions.
Prescription Pain Medications
Prescription pain medications often have more potent effects and require careful monitoring. They should only be used under the guidance of a healthcare professional.
- Opioids (e.g., codeine, oxycodone, hydrocodone): These medications are highly effective but carry a risk of addiction. Dosage and frequency are determined by the individual’s pain level and tolerance. Always follow the prescribed dosage and frequency meticulously, and never exceed the prescribed amount. The frequency of use is often dictated by the specific medication and its half-life.
- Nonsteroidal anti-inflammatory drugs (NSAIDs) in prescription form (e.g., Celecoxib): These medications are also used for pain relief, but the specific dose and frequency vary depending on the individual’s needs and the type of pain. Always adhere to the prescription instructions and seek clarification from the prescribing physician if any doubts arise.
Dosage and Frequency Table
This table provides a general overview of maximum daily dosages and recommended frequencies for various pain relievers. Note that these are general guidelines and specific recommendations may vary based on individual needs and medical conditions. Always consult with a healthcare professional before altering or starting any new medication regimen.
| Medication | Maximum Daily Dosage (approximate) | Recommended Frequency |
|---|---|---|
| Acetaminophen | 4000 mg | Every 4-6 hours as needed |
| Ibuprofen | 3200 mg | Every 4-6 hours as needed |
| Naproxen | 1000-1500 mg | Every 8-12 hours as needed |
| Codeine | Variable | As prescribed |
| Oxycodone | Variable | As prescribed |
Children’s Dosage Considerations
Children require specific dosage considerations due to their smaller body size and developing physiology. Always consult a pediatrician or healthcare provider for appropriate dosages and frequencies for children. Never give a child an adult dose of medication. Dosage calculations are often based on weight and specific age guidelines.
Interactions and Considerations
Taking pain medication safely involves understanding how different drugs can interact. This knowledge empowers you to discuss potential risks and benefits with your doctor, leading to more effective and safer pain management. Careful consideration of interactions is crucial for achieving optimal results and avoiding unwanted side effects.Different pain medications can have unexpected interactions, potentially leading to amplified effects or dangerous side effects.
These interactions can range from mild discomfort to serious health complications. It’s vital to understand these potential interactions to make informed decisions about your medication regimen.
Medication Interaction Mechanisms
Understanding how medications interact is key to managing pain safely. Many medications are metabolized by the liver, and the concurrent use of multiple medications can lead to competition for these metabolic pathways. This competition can affect the rate at which the medications are processed, leading to either increased or decreased levels of the active drug in the bloodstream.
Other mechanisms of interaction include altering the absorption or excretion of drugs, or by impacting the receptor sites the drugs target.
Importance of Communicating with Healthcare Providers
Open communication with healthcare providers about all medications, including over-the-counter drugs, supplements, and herbal remedies, is paramount. This comprehensive approach ensures that your doctor has a complete picture of your current health status and medication regimen. This enables them to identify potential drug interactions and tailor the pain management plan accordingly. Failure to disclose all medications can lead to unforeseen complications.
Examples of Drug Interactions with Pain Relievers
Several medications can interact with pain relievers, potentially causing significant side effects. This section provides examples to illustrate the importance of thorough communication with your doctor.
- Nonsteroidal anti-inflammatory drugs (NSAIDs), such as ibuprofen and naproxen, can increase the risk of gastrointestinal bleeding when taken with blood thinners like warfarin. This increased risk can lead to ulcers or stomach bleeding, which can be serious.
- Acetaminophen (paracetamol) can be toxic to the liver when taken in excessive amounts, and this risk is amplified when combined with alcohol or certain other medications. The liver plays a crucial role in processing medications, and exceeding its capacity can cause significant damage.
- Opioid pain relievers, such as codeine and morphine, can interact with other medications, such as sedatives or antidepressants, to increase the risk of drowsiness, dizziness, or respiratory depression. This combination can significantly impair function and potentially be life-threatening.
- Certain medications used to treat high blood pressure or heart conditions can interact with NSAIDs, potentially affecting blood pressure control. This underscores the importance of informing your doctor about all medications.
Reporting Suspected Adverse Reactions
Prompt reporting of any suspected adverse reactions to medication is crucial for patient safety and improving healthcare practices. This allows healthcare providers to identify potential issues, track patterns, and ultimately improve the safety and efficacy of treatments.
- Always report any unusual symptoms, such as severe or persistent nausea, vomiting, skin rash, itching, or difficulty breathing, immediately to your healthcare provider. These symptoms could indicate a potential adverse reaction to the medication.
- Detailed information about the symptoms, the medication, and the timing of the onset can significantly aid the healthcare provider in assessing the situation. Be prepared to provide specifics about the symptoms and the medication.
- Keeping a medication log can help track potential patterns of adverse reactions, which may provide valuable insights for the healthcare team. This record includes the date, time, medication, dose, and any observed effects.
Pain Management Strategies
Taking a holistic approach to pain management is crucial for long-term well-being. Simply relying on medication often overlooks the powerful role of lifestyle changes and alternative therapies. This section explores effective non-pharmacological strategies to complement medication and improve overall pain management.Effective pain management goes beyond just treating the symptoms; it encompasses addressing the root causes and supporting the body’s natural healing processes.
Integrating various approaches, including medication, physical therapy, and lifestyle adjustments, often yields superior results compared to relying on medication alone. By understanding and implementing these strategies, individuals can actively participate in their recovery and lead more fulfilling lives.
Alternative Pain Relief Methods
Non-pharmacological approaches can significantly reduce pain and improve quality of life. These methods work by addressing the underlying causes of pain and promoting overall well-being. Physical therapy, for example, focuses on restoring function and improving mobility, thereby reducing pain.
- Physical Therapy: A physical therapist develops a personalized exercise program to strengthen muscles, improve flexibility, and address any physical limitations contributing to pain. This can include stretching, strengthening exercises, and manual therapy techniques.
- Lifestyle Changes: Adopting a healthier lifestyle can profoundly impact pain management. A balanced diet, regular exercise, and stress management techniques can reduce inflammation and improve overall physical function.
- Mind-Body Practices: Techniques like yoga, tai chi, and meditation can promote relaxation, reduce stress, and improve pain tolerance. These practices can be particularly effective for chronic pain conditions.
- Heat and Cold Therapy: Applying heat or cold packs to the affected area can help reduce pain and inflammation. Heat promotes blood flow, while cold reduces swelling and inflammation.
Combining Medication with Other Strategies, How often should i takegive pain medications
Combining medication with other pain management strategies is often more effective than using medication alone. This approach considers the individual’s specific needs and conditions, allowing for a more comprehensive and targeted treatment plan.
- Synergy in Treatment: Non-pharmacological methods work synergistically with medication. For instance, a patient undergoing physical therapy while taking pain medication can experience a faster recovery and reduced reliance on medication over time.
- Personalized Approach: The most effective approach combines medication with strategies tailored to the individual’s specific needs and condition. This personalized approach ensures that treatment addresses both the symptoms and the underlying causes of pain.
- Improved Outcomes: Combining medication with other strategies often leads to improved outcomes in terms of pain reduction, functional improvement, and overall quality of life. This approach can minimize adverse effects and optimize the therapeutic benefits.
Effective Non-Pharmacological Techniques
Various non-pharmacological techniques are proven effective in managing pain. These methods can be integrated into a comprehensive pain management plan.
- Acupuncture: This ancient practice involves inserting thin needles into specific points on the body. It’s believed to stimulate the flow of energy and reduce pain signals.
- Massage Therapy: Massage therapy can reduce muscle tension, improve circulation, and release endorphins, which have natural pain-relieving properties.
- Guided Imagery and Relaxation Techniques: These techniques help individuals focus on positive thoughts and images, promoting relaxation and reducing pain perception.
Incorporating Lifestyle Changes
A comprehensive pain management plan often includes lifestyle adjustments. These adjustments promote overall well-being and can significantly impact pain levels.
- Balanced Diet: A diet rich in fruits, vegetables, and whole grains provides essential nutrients to support overall health and reduce inflammation.
- Regular Exercise: Regular physical activity, tailored to individual abilities, strengthens muscles, improves flexibility, and enhances overall physical function.
- Stress Management: Techniques like deep breathing exercises, mindfulness, and meditation can help reduce stress levels, which can often exacerbate pain.
Monitoring and Adjustment
Staying on top of your pain management plan is crucial for effective pain relief and minimizing potential side effects. Regular monitoring and adjustments are essential for ensuring that your medication regimen remains safe and effective. This involves paying close attention to how your pain levels change and how your body responds to the medication.Understanding how your pain responds to different medication dosages and frequencies allows you to tailor your treatment for optimal results.
This dynamic approach is vital because pain levels fluctuate, and medication effectiveness can vary from person to person and even over time. By carefully monitoring and adjusting your treatment plan, you can achieve the best possible pain relief while minimizing any potential risks.
Importance of Regular Pain Level Monitoring
Consistent tracking of pain levels is vital for adjusting your medication regimen effectively. This helps you identify patterns and trends in your pain, allowing you to predict future pain episodes and adjust your medication accordingly. Regular monitoring also helps you to notice changes in your pain response to the medication over time. This early detection of changes is crucial for preventing pain from becoming chronic or escalating to more severe levels.
Figuring out how often to take pain meds can be tricky, especially if you’re also dealing with anxiety. Sometimes, physical discomfort can amplify feelings of anxiety, which is why it’s important to manage both. Learning techniques for managing anxiety can significantly help you navigate pain medication schedules more effectively, such as practicing mindfulness or deep breathing exercises.
For more in-depth guidance on how to deal with anxiety, check out this helpful resource: how to deal with anxiety. Ultimately, sticking to your doctor’s prescribed dosage and schedule is crucial for managing pain effectively and safely.
Methods for Adjusting Medication Frequency
Adjusting medication frequency involves systematically increasing or decreasing the dosage or administration schedule based on your pain levels and how your body responds to the medication. This process is best done gradually, with your healthcare provider’s guidance. You should carefully document your pain levels and the medication’s effectiveness in a pain journal or log. This detailed record provides valuable insights into the relationship between your pain and the medication.
Tracking Medication Usage and Adjustments
A detailed record of your medication use, including the dosage, frequency, and time of administration, is invaluable. This allows you to observe patterns and trends in your pain response. Note any side effects experienced and record them in your log. By noting these details, you can identify which dosages and frequencies are most effective for you. A simple table can be very helpful for tracking.
For example:
| Date | Time | Pain Level (1-10) | Medication | Dosage | Side Effects |
|---|---|---|---|---|---|
| October 26, 2023 | 8:00 AM | 7 | Ibuprofen | 600 mg | None |
| October 26, 2023 | 2:00 PM | 8 | Ibuprofen | 600 mg | Slight nausea |
| October 26, 2023 | 8:00 PM | 6 | Ibuprofen | 600 mg | None |
This structured approach allows you to see how your pain changes over time and how your body responds to the medication.
Seeking Professional Guidance for Significant Changes
Any significant changes to your pain management regimen, including altering medication frequency or dosage, should be discussed with your healthcare provider. They can assess the potential risks and benefits of such changes, and they can ensure that your treatment plan remains safe and effective. Your doctor can help you understand how these changes may interact with other medications you are taking, as well as the possible consequences of abrupt or drastic changes.
They can guide you through the process of adjusting your regimen to maximize benefits and minimize risks.
Patient Education: How Often Should I Takegive Pain Medications
Empowering patients with knowledge about pain medication use is crucial for effective pain management. This involves more than just providing a list of instructions; it’s about fostering a partnership where patients actively participate in their own care. Clear communication and tailored explanations are key to ensuring patients understand the importance of proper medication use and the potential risks of misuse.
Importance of Patient Understanding
Patient understanding of pain medication use goes beyond memorizing instructions. It encompasses comprehending the rationale behind dosage, frequency, and potential side effects. A patient who understands their condition and treatment plan is more likely to adhere to prescribed regimens, reducing the risk of complications and maximizing the effectiveness of the medication. This understanding also allows patients to communicate concerns and adjust their use as needed, under the guidance of their healthcare provider.
Tips for Educating Patients
Effective patient education relies on clear, concise language and visual aids. Use plain language, avoiding medical jargon, and explain complex concepts in a relatable manner. Visual aids, such as charts or diagrams, can significantly enhance understanding, especially when explaining dosage regimens or potential side effects. Encourage open communication and address any questions or concerns promptly and thoroughly.
Consider using interactive methods, such as role-playing or case studies, to reinforce learning and encourage active participation.
Key Points for Pain Medication Use
Understanding the rationale behind pain medication use is vital. Patients should be aware of the medication’s intended purpose, how it works in the body, potential side effects, and how it interacts with other medications or health conditions. Frequency of use, as determined by a healthcare professional, is crucial to managing pain effectively and preventing potential adverse effects. Regular monitoring of pain levels and medication response is essential for adjusting the treatment plan as needed.
Understanding Individual Needs
Individual patient needs vary considerably. A patient’s age, overall health, and other medications they’re taking can significantly influence how they respond to pain medication. Understanding these factors allows healthcare providers to tailor educational materials and treatment plans to meet individual needs. Encourage patients to share their experiences and concerns with their healthcare provider, fostering a collaborative approach to pain management.
For example, a patient with a history of liver disease might require a different pain management strategy compared to a younger, healthier individual. This personalized approach ensures the best possible outcomes.
Concluding Remarks
In conclusion, managing pain effectively requires a balanced approach that considers medication frequency, potential side effects, and individual circumstances. Understanding how different medications work, their interactions, and the importance of professional guidance are crucial steps in achieving optimal pain relief. Remember, this information is for educational purposes only and should not be considered medical advice. Always consult with a healthcare provider before making any changes to your pain management plan.










