Medications for type 2 diabetes offer a crucial arsenal in managing this chronic condition. This guide delves into the various classes of drugs, their mechanisms of action, and potential side effects. We’ll explore common medications like metformin and examine how they impact blood glucose levels. Furthermore, we’ll discuss choosing the right medication for individual patients, considering factors like lifestyle modifications and potential interactions with other drugs.
From understanding the basics of type 2 diabetes and its impact on the body to exploring emerging treatments and future directions, this comprehensive guide aims to equip readers with the knowledge needed to navigate this complex area. We’ll also cover crucial aspects like patient education, adherence, and considerations for specific populations, such as the elderly and pregnant women. Finally, the importance of lifestyle modifications in conjunction with medication will be emphasized.
Overview of Type 2 Diabetes Medications
Type 2 diabetes is a chronic metabolic disorder characterized by high blood sugar levels. This occurs because the body either doesn’t produce enough insulin or the body’s cells don’t respond properly to insulin, a hormone essential for glucose uptake. Over time, high blood sugar can lead to serious health complications, including heart disease, stroke, kidney damage, nerve damage, and eye problems.
Effective management of blood sugar is crucial to prevent or delay these complications.Various medications are available to help manage type 2 diabetes, targeting different aspects of the disease’s pathophysiology. These medications work by either stimulating insulin production, improving insulin sensitivity, or reducing glucose absorption from the gut.
While medications play a crucial role in managing type 2 diabetes, it’s equally important to consider the broader picture of access to type 2 diabetes care. Factors like insurance coverage and geographical location can significantly impact a person’s ability to obtain the necessary medications and support. Finding the right balance between medication and comprehensive care, like that offered through access to type 2 diabetes care , is key to effective management.
Ultimately, the best medication strategy for type 2 diabetes hinges on individual needs and access to comprehensive care.
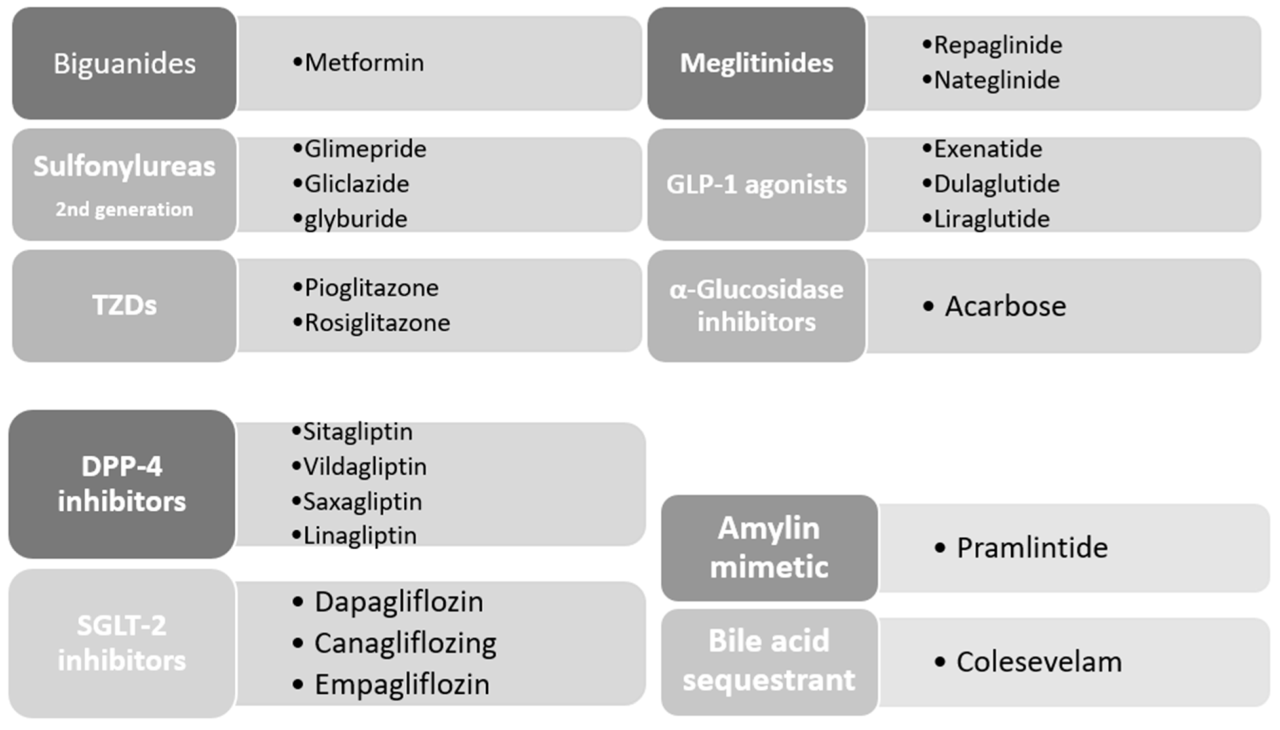
Different Classes of Type 2 Diabetes Medications
Several classes of medications are used to treat type 2 diabetes, each with its own mechanism of action. Understanding these mechanisms helps in tailoring treatment strategies to individual patient needs.
Medication Classes and Their Mechanisms
| Class Name | Mechanism of Action | Common Side Effects | Examples of Drugs |
|---|---|---|---|
| Biguanides | These drugs, primarily metformin, reduce glucose production in the liver and improve insulin sensitivity in muscle cells. They also slightly reduce glucose absorption from the gut. | Gastrointestinal upset (e.g., diarrhea, nausea), vitamin B12 deficiency (long-term use). | Metformin (Glucophage) |
| Sulfonylureas | These medications stimulate the pancreas to release more insulin. | Hypoglycemia (low blood sugar), weight gain, increased risk of cardiovascular events (in some studies). | Glipizide (Glucotrol), Glyburide (DiaBeta) |
| Thiazolidinediones (TZDs) | These drugs increase insulin sensitivity in muscle, fat, and liver cells. | Weight gain, fluid retention, increased risk of heart failure, possible liver problems. | Pioglitazone (Actos), Rosiglitazone (Avandia) |
| DPP-4 Inhibitors | These medications prevent the breakdown of incretin hormones, which stimulate insulin release and suppress glucagon secretion. | Upper respiratory tract infections, headache, diarrhea, pancreatitis (rare). | Sitagliptin (Januvia), Saxagliptin (Onglyza) |
| SGLT2 Inhibitors | These drugs block the reabsorption of glucose in the kidneys, leading to increased glucose excretion in urine. | Increased urination, genital infections, dehydration, risk of diabetic ketoacidosis in some individuals. | Canagliflozin (Invokana), Dapagliflozin (Farxiga) |
| GLP-1 Receptor Agonists | These medications mimic the effects of incretin hormones, stimulating insulin release, suppressing glucagon secretion, and slowing gastric emptying. Many of these drugs are administered via injection. | Nausea, vomiting, diarrhea, pancreatitis (rare), thyroid cancer (some studies, not conclusive). | Liraglutide (Victoza), Exenatide (Byetta) |
Common Medications for Type 2 Diabetes
Understanding the various medications available for managing type 2 diabetes is crucial for individuals seeking effective treatment options. This section delves into the common classes of drugs, their mechanisms of action, and important considerations regarding their use. Effective management of blood glucose levels is paramount in preventing long-term complications associated with the disease.
Metformin, Medications for type 2 diabetes
Metformin is often the first-line medication prescribed for type 2 diabetes. Its primary mechanism involves decreasing hepatic glucose production and improving insulin sensitivity in peripheral tissues. Metformin does not directly stimulate insulin secretion from the pancreas, making it generally well-tolerated by most patients.
- Metformin typically lowers blood glucose levels by reducing the amount of glucose produced by the liver and enhancing the body’s response to insulin. This dual action helps maintain healthy blood sugar levels.
- Common side effects include gastrointestinal issues like nausea, diarrhea, and abdominal discomfort. These side effects are often mild and temporary, but patients should discuss them with their doctor.
- Metformin’s effectiveness varies among individuals, with some experiencing significant improvements in blood glucose control while others may require additional medications. Factors like diet and lifestyle choices play a crucial role in maximizing its efficacy.
Sulfonylureas
Sulfonylureas stimulate insulin release from the beta cells in the pancreas. This class of medications can be effective in lowering blood glucose, but they may also carry a higher risk of hypoglycemia (low blood sugar) compared to metformin.
- Sulfonylureas increase insulin production by the pancreas, which directly lowers blood sugar levels. However, this increased insulin production can lead to potential hypoglycemia, especially if not managed properly.
- Examples of sulfonylureas include glimepiride and glipizide. The specific effectiveness and side effect profile can vary between different sulfonylureas.
- Potential side effects include weight gain and hypoglycemia. Patients need to monitor their blood sugar levels closely and adjust their diet and lifestyle accordingly.
GLP-1 Receptor Agonists
GLP-1 receptor agonists mimic the effects of the incretin hormone GLP-1. These medications enhance insulin secretion in response to food intake, slow gastric emptying, and reduce appetite.
- GLP-1 receptor agonists promote insulin release in response to elevated blood glucose levels. This mechanism helps regulate blood sugar levels and can contribute to weight loss in some individuals.
- Common examples of GLP-1 receptor agonists include liraglutide and semaglutide. Different GLP-1 receptor agonists may have varying degrees of efficacy and side effect profiles.
- Potential side effects can include nausea, vomiting, and diarrhea. These side effects are usually temporary and diminish with continued use. Some patients may also experience injection-site reactions.
Medication Comparison
| Medication | Cost | Efficacy | Side Effects |
|---|---|---|---|
| Metformin | Generally affordable | Effective in lowering blood glucose, often first-line | GI upset (common), rarely serious |
| Sulfonylureas | Usually affordable | Effective in lowering blood glucose | Hypoglycemia, weight gain |
| GLP-1 Receptor Agonists | Can be more expensive | Effective in lowering blood glucose, often associated with weight loss | GI upset (common), potential injection site reactions |
Choosing the Right Medication: Medications For Type 2 Diabetes
Finding the right medication for type 2 diabetes is a personalized journey, not a one-size-fits-all approach. It requires careful consideration of individual patient factors, lifestyle, and the specific needs of each person. The goal is to effectively control blood sugar levels while minimizing side effects and improving overall well-being.Choosing the appropriate medication is a collaborative process between the patient and their healthcare provider.
This involves understanding the nuances of various medications, potential interactions, and the impact on individual health conditions. It’s a dynamic process that may necessitate adjustments as the patient’s health and needs evolve.
Factors Influencing Medication Selection
Understanding the individual patient’s characteristics is crucial for selecting the most suitable medication. This includes not only their medical history but also their lifestyle and preferences.
- Medical History: Pre-existing conditions, such as kidney disease, heart problems, or liver issues, can significantly impact medication choices. For instance, a patient with severe kidney disease might require medications with reduced renal excretion. Likewise, a patient with heart failure might benefit from medications with less impact on the cardiovascular system.
- Lifestyle Factors: Diet, exercise habits, and overall lifestyle significantly influence the effectiveness of medications. A patient actively engaged in lifestyle modifications might require a lower dosage or a different type of medication compared to a patient with sedentary habits. For example, a patient committed to a low-carbohydrate diet may respond well to a medication that targets post-meal glucose spikes.
- Patient Preferences: The patient’s preferences regarding medication frequency, administration method (oral vs. injectable), and potential side effects play a significant role. A patient who prefers an oral medication might be better suited for a once-daily pill than an injectable medication requiring multiple daily doses. This consideration is vital to promote patient adherence to the treatment plan.
- Cost and Insurance Coverage: The financial implications of medication choices must be considered. Some medications can be significantly more expensive than others. Insurance coverage can vary, impacting the affordability of different options. Healthcare providers should discuss cost implications with patients to ensure affordability and sustainability of treatment.
Lifestyle Modifications and Medication Synergy
Lifestyle modifications are integral to the success of any type 2 diabetes treatment plan. They enhance the effectiveness of medications and contribute to overall well-being.
- Diet and Nutrition: A balanced diet, low in processed foods and sugars, is essential. It helps manage blood glucose levels and improves overall health. Specific dietary approaches, such as the Mediterranean diet, have shown positive results in managing type 2 diabetes.
- Regular Exercise: Regular physical activity improves insulin sensitivity and helps manage weight. Consistent exercise routines can significantly improve blood glucose control, reducing reliance on medication.
- Stress Management: Chronic stress can impact blood sugar levels. Stress management techniques, such as meditation or yoga, can be beneficial in improving overall health and blood glucose control.
Decision-Making Flow Chart
A decision-making flow chart can guide clinicians in selecting appropriate medications for different patient profiles. The specific criteria and considerations are tailored to the individual patient.
| Patient Profile | Initial Considerations | Potential Medications |
|---|---|---|
| Patient with well-controlled blood sugar, mild symptoms, and no significant comorbidities | Lifestyle modifications, metformin as first-line | Metformin, SGLT2 inhibitors, DPP-4 inhibitors |
| Patient with uncontrolled blood sugar despite lifestyle modifications and metformin | Consider adding a second medication, assess for comorbidities | Combination therapy with two oral medications, GLP-1 receptor agonists, insulin |
| Patient with severe comorbidities, such as kidney disease or heart failure | Choose medications with minimal impact on the specific comorbidity | SGLT2 inhibitors (for kidney protection), GLP-1 receptor agonists (for cardiovascular benefits) |
“Individualized treatment plans are crucial for successful type 2 diabetes management. The selection of medications should be tailored to the specific needs of each patient.”
Potential Side Effects and Interactions
Understanding the potential side effects of diabetes medications is crucial for effective management. Knowing what to expect and how to address any issues can empower you to make informed decisions with your doctor. This knowledge allows for proactive strategies to minimize discomfort and optimize treatment outcomes.Managing type 2 diabetes often involves a combination of lifestyle changes and medication.
However, medications can have side effects, and some medications may interact with others, potentially affecting their effectiveness or increasing the risk of adverse reactions. Understanding these potential side effects and interactions is vital for safe and successful diabetes management.
Potential Side Effects of Different Medication Classes
Different classes of type 2 diabetes medications have varying potential side effects. This section provides an overview of common side effects associated with different medication groups. Careful monitoring and open communication with your healthcare provider are essential to identify and manage any potential issues promptly.
- Metformin: Common side effects include gastrointestinal issues like nausea, vomiting, diarrhea, and abdominal discomfort. These side effects are often mild and temporary, particularly when the medication is started at a low dose and gradually increased. To manage these effects, taking the medication with food can help reduce stomach upset. If symptoms persist or worsen, consult your doctor immediately.
- Sulfonylureas: These medications can cause hypoglycemia (low blood sugar), especially if combined with other diabetes medications or insufficient food intake. Symptoms of hypoglycemia include shakiness, sweating, dizziness, and confusion. Adjusting meal timing and portion sizes, or consulting with your doctor about medication adjustments, can help manage this risk. Regular blood sugar monitoring is crucial for detecting and preventing hypoglycemia.
- Thiazolidinediones: Fluid retention and weight gain are potential side effects. Regular monitoring of blood pressure and weight is important. Your doctor can advise on appropriate strategies to manage these side effects.
- DPP-4 Inhibitors: These medications often cause mild gastrointestinal issues such as nausea, diarrhea, or vomiting. As with other medications, these issues are often temporary and can be managed with lifestyle adjustments, such as taking the medication with food. Consult your doctor if symptoms persist or worsen.
- GLP-1 Receptor Agonists: Nausea and vomiting are common initial side effects, but these typically diminish over time. Starting with a low dose and gradual titration, alongside taking the medication with food, can help alleviate these symptoms. Consult your healthcare provider if nausea or vomiting is severe or persistent.
- SGLT2 Inhibitors: These medications can increase the risk of urinary tract infections (UTIs) and genital yeast infections. Maintaining good hygiene practices and promptly addressing any signs of infection are crucial. If infections persist, consult your doctor immediately.
Drug Interactions
Medication interactions can significantly impact the effectiveness and safety of diabetes treatments. It’s essential to inform your doctor about all medications, supplements, and herbal remedies you are taking. This comprehensive approach allows for proactive management of potential interactions and ensures optimal treatment outcomes.
Managing type 2 diabetes often involves medication, but sometimes the side effects can be surprising. For example, certain medications can affect your feet, potentially leading to discomfort like foot pain in the ball of the foot. Understanding these potential complications is crucial for managing the condition effectively. Learning about the link between medication and foot pain, like foot pain in ball of foot , can help you discuss options with your doctor and adjust your treatment plan.
Ultimately, the goal is to find the right medication balance for overall health and well-being.
- Alcohol: Alcohol can interact with several diabetes medications, potentially increasing the risk of hypoglycemia. Limit alcohol intake, especially if taking medications that can lower blood sugar.
- Other Medications: Some medications, such as diuretics, corticosteroids, and certain antibiotics, can affect blood sugar levels and may interact with diabetes medications. Regular communication with your doctor about all medications is essential to avoid adverse effects.
- Herbal Remedies: Some herbal remedies can also interact with diabetes medications. Always discuss herbal remedies with your doctor before using them, particularly if you are taking diabetes medications.
Managing Side Effects
Proactive strategies are crucial for effectively managing potential side effects. Implementing these strategies can minimize discomfort and ensure the medication’s effectiveness. Communicate openly with your doctor about any concerns or side effects you experience.
- Dietary Adjustments: Adjusting your diet, particularly the timing and composition of meals, can often mitigate gastrointestinal side effects associated with certain medications.
- Hydration: Staying well-hydrated can help manage side effects like dehydration and fluid retention, which can be associated with certain medications.
- Lifestyle Modifications: Regular exercise and stress management techniques can play a role in mitigating certain side effects and promoting overall well-being.
Medication-Specific Side Effects Table
| Medication Class | Potential Side Effects | Frequency | Management Strategies |
|---|---|---|---|
| Metformin | Nausea, vomiting, diarrhea, abdominal discomfort | Common (especially initially) | Take with food, start low and titrate slowly |
| Sulfonylureas | Hypoglycemia | Possible | Adjust meal timing, monitor blood sugar closely |
| Thiazolidinediones | Fluid retention, weight gain | Possible | Monitor blood pressure, weight, and fluid intake |
| DPP-4 Inhibitors | Mild gastrointestinal issues | Possible | Take with food, monitor symptoms |
| GLP-1 Receptor Agonists | Nausea, vomiting | Common initially | Start low, take with food, monitor symptoms |
| SGLT2 Inhibitors | UTIs, genital yeast infections | Possible | Maintain good hygiene, monitor for signs of infection |
Emerging Treatments and Future Directions
The landscape of Type 2 Diabetes management is constantly evolving, with researchers tirelessly exploring innovative treatments and strategies. This dynamic field promises exciting advancements that could significantly improve the lives of those affected. New medications and approaches are being developed, offering potential benefits beyond existing therapies. This section will delve into recent breakthroughs and discuss their potential impact on the future of diabetes care.
Recent Advancements in Medication
Several promising avenues of research are currently yielding exciting results. One area of significant interest involves the development of novel therapies targeting specific mechanisms underlying the disease. These new approaches aim to address the root causes of insulin resistance and impaired glucose regulation, potentially offering more comprehensive solutions than existing treatments. The development of medications designed to address these complex mechanisms will likely be a game changer in the field.
Emerging Therapies
New classes of medications are in various stages of clinical development. These include drugs that modulate the gut microbiome, potentially improving insulin sensitivity. Another exciting area focuses on therapies that directly target pancreatic beta cell function, aiming to restore or enhance their ability to produce insulin. Researchers are also exploring the use of gene therapy to potentially influence insulin production or sensitivity.
Such developments hold the promise of addressing the root cause of the condition rather than just managing symptoms.
Future of Diabetes Management
These emerging therapies could reshape the future of diabetes management. Imagine a future where treatments are more personalized, targeting individual patient needs and genetic predispositions. This approach would likely lead to improved glycemic control, reduced long-term complications, and enhanced patient well-being. Furthermore, the possibility of preventing the onset of Type 2 Diabetes through preventative therapies is a tantalizing prospect.
Timeline of Medication Evolution
| Year | Significant Milestone |
|---|---|
| 1921 | Insulin discovered, revolutionizing diabetes treatment. |
| 1950s | Oral hypoglycemic agents introduced, expanding treatment options. |
| 1990s | Thiazolidinediones and sulfonylureas emerged, further improving control. |
| 2000s | Metformin solidified its position as a first-line treatment. |
| Present | Focus on personalized medicine, novel mechanisms, and prevention. |
The table above provides a glimpse into the historical evolution of Type 2 Diabetes medications. Each milestone represents a significant step forward in our understanding and treatment of the disease.
Patient Education and Adherence
Effective management of type 2 diabetes hinges not just on medication, but also on patient understanding and commitment. A robust patient education program empowers individuals to actively participate in their care, leading to better outcomes and a higher quality of life. This crucial aspect involves more than just providing information; it necessitates fostering understanding, building confidence, and cultivating a sense of ownership over the treatment process.
Importance of Patient Education
Patient education is fundamental to successful diabetes management. It equips patients with the knowledge and skills needed to understand their condition, adhere to their medication regimen, and make informed lifestyle choices. This knowledge empowers them to actively participate in their care, leading to better blood sugar control, reduced complications, and improved overall health. A well-structured education program addresses not only the technical aspects of the disease and treatment but also the emotional and practical challenges faced by patients.
Strategies to Improve Medication Adherence
Medication adherence is crucial for achieving therapeutic goals in type 2 diabetes. Several strategies can enhance adherence. These strategies include simplifying medication schedules, providing clear and concise instructions, and offering ongoing support and encouragement. Furthermore, considering the patient’s individual circumstances, preferences, and lifestyle can significantly impact adherence.
- Simplified Medication Regimens: Complex medication schedules can lead to missed doses. Healthcare professionals should work with patients to design a regimen that is easy to follow, perhaps by combining medications or adjusting dosing times to align with daily routines. For example, a patient taking multiple pills daily could be transitioned to a once-a-day medication if possible.
- Clear Communication and Instructions: Patients need clear, concise, and understandable information about their medications, including how to take them, potential side effects, and when to contact their healthcare provider. This includes written materials, verbal explanations, and visual aids.
- Ongoing Support and Encouragement: Regular follow-up appointments, phone calls, or online support groups can help patients stay motivated and committed to their treatment plan. A dedicated diabetes educator can provide personalized support and address any concerns.
- Individualized Approaches: Consideration of individual circumstances, cultural backgrounds, and literacy levels is crucial for tailoring educational materials and support to the patient’s needs. For example, a visually impaired patient might benefit from audio recordings of instructions.
Communication with Patients
Effective communication is essential for building trust and fostering a collaborative relationship between healthcare providers and patients. This involves active listening, clear explanations, and empathetic responses to patient concerns.
- Active Listening: Truly understanding a patient’s perspective, concerns, and anxieties about their medication regimen is crucial. This involves acknowledging their feelings and addressing their questions directly and openly.
- Clear Explanations: Use clear and concise language to explain complex medical concepts. Avoid jargon and technical terms, and encourage patients to ask questions.
- Empathetic Responses: Respond with empathy to patient concerns, addressing fears and anxieties about potential side effects or treatment complexities. Validation of their feelings can build trust.
- Open Dialogue: Create an environment where patients feel comfortable asking questions, expressing concerns, and sharing their experiences. Encourage open communication about treatment plans and expectations.
Components of a Comprehensive Patient Education Program
A comprehensive patient education program for diabetes management should cover various aspects of the disease and its management.
- Disease Management Education: The program should provide comprehensive information about type 2 diabetes, including its causes, symptoms, complications, and long-term management strategies.
- Medication Education: This includes details about the prescribed medications, how to take them, potential side effects, and when to contact the healthcare provider.
- Lifestyle Modifications: The program should emphasize the importance of healthy eating, regular physical activity, and stress management techniques in managing blood sugar levels.
- Monitoring Techniques: The program should cover blood glucose monitoring techniques, including how to use a glucometer and interpret results.
- Problem-Solving Skills: Teaching patients how to identify and address potential challenges related to their diabetes management is crucial.
Medication Considerations for Specific Populations
Managing type 2 diabetes requires careful consideration of individual patient characteristics. Different populations, such as the elderly, pregnant women, and those with kidney disease, present unique challenges when it comes to medication selection and dosage. This section explores these considerations, highlighting potential adjustments and risks associated with various medications.
Elderly Patients
Older adults often have multiple health conditions, impacting their ability to tolerate certain medications. This necessitates a more cautious approach to medication selection and dosage adjustments. For example, some medications may have a slower rate of elimination in the elderly, leading to potentially higher drug concentrations and an increased risk of side effects. Careful monitoring of blood glucose levels and other relevant parameters is crucial.
Managing type 2 diabetes often involves medication, but incorporating lifestyle changes like exercise is also crucial. A great way to improve your overall well-being and potentially ease back pain is by trying the one legged balance challenge for backache. This, combined with the right medication regimen, can contribute to better long-term health outcomes and help you feel your best.
Ultimately, finding a holistic approach to managing type 2 diabetes is key.
The elderly may also have decreased kidney function, requiring dose reductions of medications that are primarily eliminated by the kidneys. Clinicians need to be aware of these factors and choose medications with a lower risk of adverse events, considering the overall health profile of the patient.
Pregnant Women
Managing diabetes during pregnancy is critical for both the mother and the developing fetus. Certain medications may not be suitable for use during pregnancy due to potential risks to the fetus. Metformin is generally considered safe for use during pregnancy, and lifestyle modifications are often prioritized as initial treatment strategies. Insulin is frequently used in cases where lifestyle changes are insufficient.
The fluctuating hormonal changes during pregnancy can affect blood glucose levels, necessitating careful monitoring and adjustments to treatment regimens. Regular medical check-ups and close communication with healthcare providers are vital.
Patients with Kidney Disease
Kidney disease significantly impacts how medications are processed and eliminated from the body. This necessitates careful consideration of medication choices and dosages. Medications primarily eliminated by the kidneys may require dose adjustments or even complete discontinuation. For example, some sulfonylureas are less suitable for patients with kidney disease due to their potential for accumulating in the body.
The specific adjustments will depend on the severity of the kidney impairment and the individual patient’s condition. Close monitoring of kidney function and blood glucose levels is essential to ensure effective and safe treatment.
Medication Considerations Table
| Patient Population | Medication Considerations | Potential Adjustments | Example Medications |
|---|---|---|---|
| Elderly | Slower elimination, potential for increased drug concentration, multiple comorbidities | Lower initial doses, frequent monitoring, selection of medications with fewer side effects | Metformin, some DPP-4 inhibitors |
| Pregnant Women | Potential risks to the fetus, fluctuating blood glucose levels | Lifestyle modifications, Metformin, Insulin | Metformin, insulin |
| Patients with Kidney Disease | Impaired medication processing and elimination | Dose adjustments, selection of medications with renal clearance considerations | Metformin (with caution), GLP-1 receptor agonists (some) |
Lifestyle Modifications
Managing type 2 diabetes effectively often goes beyond medication. Lifestyle modifications play a crucial role in controlling blood sugar levels, improving overall health, and potentially reducing the need for certain medications. By adopting healthier habits, individuals can significantly impact their diabetes management.
The Importance of Lifestyle Modifications
Type 2 diabetes is a chronic condition that arises from a complex interplay of genetic predisposition and lifestyle factors. While medications can help manage blood sugar, a comprehensive approach that includes lifestyle modifications is essential for long-term health and well-being. By making sustainable changes to diet, exercise, and stress management, individuals can improve insulin sensitivity, reduce blood glucose levels, and potentially prevent or delay complications associated with the disease.
This proactive approach empowers individuals to take an active role in managing their condition and enhancing their quality of life.
The Role of Diet in Blood Sugar Control
A balanced and healthy diet is fundamental to controlling blood sugar levels. Focus on whole, unprocessed foods, including fruits, vegetables, lean proteins, and whole grains. Limit refined carbohydrates, sugary drinks, and processed foods. Portion control is also essential, as overeating can lead to spikes in blood glucose. Regular monitoring of carbohydrate intake and understanding how different foods impact blood sugar is critical.
A registered dietitian can provide personalized dietary plans tailored to individual needs and preferences, helping patients make informed food choices.
The Role of Exercise in Blood Glucose Management
Regular physical activity is crucial for improving insulin sensitivity and managing blood sugar levels. Exercise helps the body use glucose more efficiently. Both aerobic and resistance exercises are beneficial. Aerobic activities, such as brisk walking, jogging, swimming, or cycling, improve cardiovascular health and help regulate blood sugar. Resistance training, such as weightlifting or bodyweight exercises, builds muscle mass, which further enhances insulin sensitivity.
Finding activities that are enjoyable and sustainable is key to long-term adherence.
The Role of Stress Management in Blood Sugar Control
Chronic stress can negatively impact blood sugar control. Stress hormones, like cortisol, can increase blood glucose levels. Stress management techniques, such as yoga, meditation, deep breathing exercises, and spending time in nature, can help reduce stress levels and improve blood sugar control. Identifying and managing stressors in daily life is an important component of a holistic approach to diabetes management.
Comparing the Effectiveness of Lifestyle Interventions
The effectiveness of different lifestyle interventions varies based on individual factors. While a balanced diet is essential for all, the specific dietary approach might differ based on individual needs and preferences. Similarly, the optimal exercise regimen can vary based on physical capabilities and individual preferences. Stress management techniques can also be customized to suit individual needs and preferences.
A holistic approach that integrates all three components is often most effective in achieving and maintaining optimal blood glucose control.
Actionable Steps for Lifestyle Improvement
- Dietary Changes: Gradually incorporate more fruits, vegetables, and whole grains into your diet. Limit processed foods, sugary drinks, and refined carbohydrates. Consider consulting a registered dietitian for personalized meal plans.
- Physical Activity: Aim for at least 150 minutes of moderate-intensity aerobic exercise per week. Incorporate strength training exercises two or more times per week. Find activities you enjoy to maintain motivation.
- Stress Management: Practice relaxation techniques, such as deep breathing exercises, meditation, or yoga. Prioritize sufficient sleep and time management to reduce stress levels.
- Monitoring and Support: Regularly monitor blood glucose levels and adjust lifestyle choices as needed. Seek support from healthcare professionals and support groups for encouragement and guidance.
Closing Notes
In conclusion, managing type 2 diabetes effectively requires a multifaceted approach, combining medication with lifestyle changes. This guide has provided a thorough overview of medications for type 2 diabetes, highlighting the different classes, common uses, potential side effects, and considerations for various patient populations. By understanding the intricacies of these medications and the importance of patient education and adherence, individuals and healthcare providers can work together to achieve optimal blood glucose control and improve overall well-being.










