Overactive bladder in men sets the stage for this enthralling narrative, offering readers a glimpse into a story that is rich in detail and brimming with originality from the outset. This condition, while often overlooked, can significantly impact a man’s quality of life. We’ll explore the causes, symptoms, and available treatments for this common issue, shedding light on everything from diagnosis to lifestyle adjustments.
Men experiencing overactive bladder often face a complex interplay of physical and emotional challenges. Understanding the various contributing factors, ranging from underlying medical conditions to lifestyle choices, is key to effective management. We’ll delve into these factors and offer practical insights to help navigate the path to better bladder control.
Introduction to Overactive Bladder in Men
Overactive bladder (OAB) is a common but often under-discussed condition affecting men, characterized by a sudden, urgent need to urinate, frequently accompanied by difficulty delaying urination. This can significantly impact a man’s daily life and quality of living. Understanding the symptoms, prevalence, and impact of OAB is crucial for men experiencing these issues.While OAB can affect anyone, men and women experience it differently.
Men may have specific concerns and challenges relating to their condition. This article provides a detailed overview of OAB in men, from its definition to its impact on daily life.
Definition of Overactive Bladder in Men
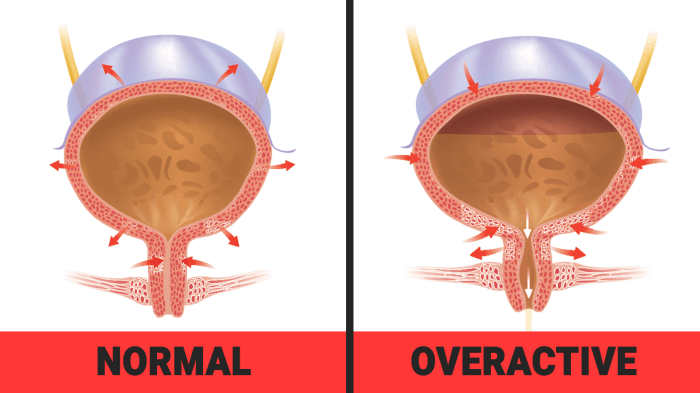
Overactive bladder (OAB) in men is a condition where the bladder muscles contract involuntarily, leading to a sudden urge to urinate. This involuntary contraction is often accompanied by frequent urination, particularly at night (nocturia). The urgency and frequency can significantly disrupt a man’s daily activities and social life.
Common Symptoms of OAB in Men
Men experiencing OAB often report a constellation of symptoms. The most prevalent include:
- Urgency: A sudden, strong need to urinate that is difficult to postpone.
- Frequency: Urinating more often than usual, especially during the day and night.
- Nocturia: Waking up at night to urinate, often multiple times.
- Incontinence: Leakage of urine before reaching the toilet, which can range from a few drops to a full bladder emptying.
Prevalence of OAB in Men
The prevalence of OAB in men is often underestimated due to underreporting and its association with other conditions. While definitive statistics vary, research suggests OAB affects a substantial portion of the male population, though often less frequently than in women. This lower prevalence is sometimes attributed to differing medical presentation or less open discussion among men.
Impact of OAB on Daily Life and Quality of Life
OAB can dramatically affect a man’s daily life. Frequent trips to the bathroom, particularly during social events or work meetings, can lead to social isolation, reduced mobility, and emotional distress. The inconvenience and associated limitations significantly impact a man’s quality of life, potentially affecting work performance, social activities, and overall well-being.
Severity Levels of OAB in Men
The severity of OAB is categorized based on the frequency and urgency of urination. The following table Artikels the different levels of severity, including example symptoms:
| Severity Level | Description | Example Symptoms |
|---|---|---|
| Mild | Occasional urgency and frequency, minimal impact on daily activities. | Urgency a few times a week, possibly some nocturia. |
| Moderate | Increased urgency and frequency, impacting daily routines, but still manageable. | Urgency several times a day, increased nocturia, occasional leakage. |
| Severe | Frequent urgency and frequency, significant disruption of daily life, impacting social and work activities. | Frequent urgency and leakage throughout the day and night, severely impacting social and work life. |
Underlying Causes and Risk Factors
Understanding why some men experience overactive bladder (OAB) requires looking beyond simple symptoms. Various factors, both medical and lifestyle-related, can contribute to this condition. A deeper understanding of these causes is crucial for effective diagnosis and management.Medical conditions can sometimes be the root cause of OAB in men. These conditions, when present, often trigger or exacerbate the symptoms.
Lifestyle choices and the natural aging process also play significant roles. It’s important to remember that OAB isn’t inevitable and that proactive measures can often mitigate its impact.
Potential Medical Conditions
Many medical conditions can affect the urinary system and contribute to OAB in men. These conditions can interfere with bladder function, leading to the frequent urge to urinate. Conditions like enlarged prostate, urinary tract infections, and neurological disorders can all be implicated.
- Prostatitis: Inflammation of the prostate gland can cause pressure on the urethra, leading to increased urgency and frequency of urination.
- Enlarged Prostate (Benign Prostatic Hyperplasia): An enlarged prostate gland can compress the urethra, making it difficult to empty the bladder completely. This can lead to a persistent urge to urinate, even when the bladder isn’t full.
- Neurological Disorders: Conditions affecting the nervous system, such as multiple sclerosis or spinal cord injuries, can disrupt the signals between the brain and the bladder, leading to OAB symptoms.
- Urinary Tract Infections (UTIs): Infections in the urinary tract can cause inflammation and irritation, leading to an increased urge to urinate.
Lifestyle Factors
Certain lifestyle choices can increase the risk of developing OAB in men. These choices can affect bladder function and contribute to the development of the condition. For instance, excessive caffeine and alcohol intake can stimulate the bladder, increasing the frequency of urination.
- Caffeine and Alcohol Consumption: High intake of caffeinated beverages and alcohol can irritate the bladder, increasing the urge to urinate.
- Smoking: Smoking can contribute to various health issues, and bladder health is no exception. Nicotine can irritate the urinary tract, potentially increasing the risk of OAB.
- Lack of Physical Activity: Regular exercise can promote overall health and well-being, including bladder health. A sedentary lifestyle may contribute to OAB symptoms.
Role of Age
The prevalence of OAB increases with age in men. As men age, changes in the urinary system can occur, making them more susceptible to developing OAB.
- Age-Related Changes in the Urinary System: Changes in bladder muscles and nerve function associated with aging can lead to a decrease in bladder capacity and an increased frequency of urination.
- Examples: A man in his 70s experiencing increased urinary frequency may be exhibiting age-related changes in bladder function.
Prostate Issues and OAB
A significant link exists between prostate issues and OAB in men. The prostate gland, located below the bladder, plays a role in urination. Problems with the prostate can affect the way the bladder functions.
- Relationship: An enlarged prostate can put pressure on the urethra, obstructing the flow of urine and causing increased urinary frequency and urgency.
- Examples: A man experiencing both urinary issues and prostate enlargement may demonstrate the connection between the two conditions.
Comparison of Potential Causes of OAB in Men and Women
| Characteristic | Men | Women |
|---|---|---|
| Prostate Issues | Common (e.g., enlarged prostate, prostatitis) | Less common |
| Neurological Disorders | Possible (e.g., multiple sclerosis, spinal cord injury) | Possible (e.g., multiple sclerosis, stroke) |
| Lifestyle Factors | Smoking, alcohol, caffeine | Smoking, alcohol, caffeine, childbirth |
| Age | Prevalence increases with age | Prevalence increases with age, especially after childbirth or menopause |
Diagnosis and Evaluation
Unraveling the mystery behind overactive bladder (OAB) in men begins with a thorough diagnostic process. This involves a careful evaluation of symptoms, medical history, and potentially, various diagnostic tests. Accurate diagnosis is crucial for developing an effective treatment plan tailored to the individual’s specific needs.
Diagnostic Process for OAB in Men
The diagnostic process for OAB in men is multifaceted, focusing on gathering comprehensive information to pinpoint the cause and severity of the condition. It’s not a single test but a series of inquiries and examinations to reach a definitive diagnosis.
Questions a Doctor Might Ask
Understanding a patient’s medical history is paramount in diagnosing OAB. A doctor will ask a range of questions to ascertain the frequency, urgency, and volume of urination, as well as any associated symptoms. This detailed history aids in determining the potential underlying causes and ruling out other conditions with similar symptoms. These questions might include inquiries about the timing of urination, the presence of pain or discomfort during urination, and any changes in bladder habits over time.
Furthermore, the doctor will inquire about any underlying medical conditions, such as diabetes or prostate enlargement, that might contribute to OAB symptoms.
Diagnostic Tests
Various diagnostic tests can be employed to evaluate OAB in men. These tests help to assess the function of the bladder and identify any potential underlying medical conditions.
| Test | Description | Purpose |
|---|---|---|
| Urinalysis | Examination of urine sample for signs of infection, blood, or other abnormalities. | To detect urinary tract infections (UTIs) or other abnormalities that might contribute to OAB symptoms. |
| Urine Culture | Growing urine sample in a laboratory to identify the presence and type of bacteria. | To confirm the presence and type of bacteria, which might indicate a UTI, a potential cause of OAB. |
| Post-void Residual (PVR) Measurement | Measuring the amount of urine remaining in the bladder after urination. | To assess bladder emptying efficiency. High PVR suggests incomplete bladder emptying, which might contribute to OAB symptoms. |
| Urodynamic Studies | A series of tests measuring bladder pressure, capacity, and flow rate. | Provides detailed information about the function of the bladder and urethra. Urodynamic studies can help distinguish OAB from other conditions. |
| Cystoscopy | Visual examination of the bladder and urethra using a thin, flexible tube with a camera. | To identify any structural abnormalities, tumors, or other issues within the urinary tract that might be causing OAB symptoms. |
Importance of Medical History
A detailed medical history provides crucial context for understanding the patient’s overall health and identifying potential contributing factors to OAB symptoms. The history encompasses previous illnesses, surgeries, medications, and family history of urinary problems. This information helps the doctor rule out other conditions and tailor the diagnostic approach. For instance, a patient with a history of diabetes might be at higher risk for certain types of OAB, necessitating a different diagnostic path.
Role of Physical Examinations
Physical examinations are an integral part of the diagnostic process. These examinations allow the doctor to assess the patient’s overall health and look for any physical signs that might suggest an underlying condition contributing to OAB. For example, an enlarged prostate can be identified during a physical examination, suggesting a potential connection to the patient’s OAB symptoms. The examination may also include evaluating the patient’s neurological status to rule out any neurological disorders that could be contributing to the symptoms.
Treatment Options and Management
Managing overactive bladder (OAB) in men involves a multifaceted approach tailored to individual needs and symptom severity. A combination of lifestyle adjustments, medications, and potentially surgical interventions can significantly improve quality of life for those affected. Understanding the various treatment options empowers men to actively participate in their healthcare decisions and find the most effective strategies for managing their OAB.
Medication Treatments for OAB
Medications play a crucial role in managing OAB symptoms. Different medications work through various mechanisms to reduce bladder contractions and increase bladder capacity. Their effectiveness varies from person to person.
- Anticholinergics: These medications are commonly prescribed to relax the bladder muscles, decreasing the frequency and urgency of urination. Examples include oxybutynin, tolterodine, and solifenacin. Potential side effects can include dry mouth, constipation, and blurred vision. Dosage adjustments and careful monitoring are often necessary to minimize these side effects.
- Beta-3 agonists: These medications stimulate specific receptors in the bladder to reduce bladder contractions. Mirabegron is a commonly prescribed example. It’s typically well-tolerated, but possible side effects include increased blood pressure and heart rate.
- Combination therapy: In some cases, combining anticholinergics with other medications, like beta-3 agonists, can provide enhanced symptom relief. However, this requires careful consideration of potential side effects.
Effectiveness of Medications for OAB in Men
The effectiveness of medications for OAB in men varies greatly. Individual responses depend on factors such as the severity of symptoms, the underlying cause of OAB, and the patient’s overall health. Clinical trials and patient experiences demonstrate that medications can significantly improve OAB symptoms for many men. However, not all medications work equally for everyone. It’s important to discuss potential side effects and adjust dosages as needed with a healthcare professional.
Lifestyle Modifications for OAB
Lifestyle modifications can be valuable adjuncts to medication therapy for OAB. These changes can often lessen symptoms and improve overall well-being.
- Fluid intake management: Adjusting fluid intake throughout the day can impact bladder frequency. Reducing fluid intake before bedtime can help prevent nighttime urination. However, proper hydration is crucial for overall health. A balanced approach is necessary to avoid dehydration and overhydration.
- Dietary modifications: Certain foods and drinks can irritate the bladder and exacerbate symptoms. Keeping a food diary can help identify potential triggers and adjust the diet accordingly. Avoiding or limiting caffeine, alcohol, and acidic foods might be beneficial for some individuals.
- Pelvic floor exercises: Strengthening the pelvic floor muscles can improve bladder control. Regular Kegel exercises can be highly effective in managing OAB symptoms.
- Weight management: Maintaining a healthy weight can positively influence bladder control. Excess weight can put pressure on the bladder, potentially worsening symptoms.
Behavioral Therapies for OAB
Behavioral therapies are often used alongside other treatments for OAB. These strategies focus on changing behaviors and habits that contribute to OAB symptoms.
- Bladder training: This involves gradually increasing the time between bathroom trips to improve bladder capacity. This approach encourages the bladder to hold more urine, reducing the need for frequent urination.
- Pelvic floor physical therapy: This approach focuses on strengthening and improving the coordination of pelvic floor muscles, thus improving bladder control.
- Biofeedback: This technique involves using devices to provide real-time feedback on bladder contractions and muscle activity. It helps patients learn to recognize and control their bladder function.
Surgical Interventions for Severe OAB
For men with severe OAB unresponsive to other treatments, surgical interventions might be considered.
| Surgical Procedure | Description | Effectiveness |
|---|---|---|
| Artificial sphincter implantation | Surgical placement of an artificial urinary sphincter, a device that helps control the flow of urine. | Highly effective for improving bladder control, but carries a risk of complications. |
| Botox injections into the bladder | Injecting botulinum toxin into the bladder to temporarily relax the muscles, decreasing bladder contractions. | May provide temporary relief, but requires repeated injections. |
Living with OAB in Men
Living with overactive bladder (OAB) can be challenging, but with the right strategies, men can effectively manage their symptoms and maintain a good quality of life. Understanding the impact of OAB on daily routines, social interactions, and emotional well-being is crucial for developing coping mechanisms. This section offers practical tips for navigating OAB in everyday life.
Dealing with an overactive bladder can be a real pain, guys. It’s a common issue, and while it’s often not immediately connected to other health concerns, sometimes it’s a sign of something else. For example, did you know that certain types of toenail fungus can sometimes cause similar symptoms? Checking out types of toenail fungus could potentially shed some light on underlying issues.
Regardless of the root cause, finding effective management strategies for overactive bladder is key.
Managing OAB Symptoms in Daily Life
Daily routines often need adjustments to accommodate OAB symptoms. Strategies for managing symptoms effectively include planning bathroom breaks in advance, particularly before outings or activities. This proactive approach helps prevent accidents and maintain a sense of control.
Improving Bladder Control and Minimizing Accidents
Strengthening pelvic floor muscles is a key strategy for improving bladder control. Kegel exercises, which involve contracting and relaxing the muscles surrounding the bladder, can be highly effective in restoring strength and function. Regular exercise, even simple activities like walking, can also improve bladder control by promoting overall physical health and reducing stress. Adequate fluid intake throughout the day is important, but it’s crucial to avoid excessive intake close to bedtime to reduce nighttime trips to the bathroom.
Impact of OAB on Social and Emotional Well-being in Men
OAB can have a significant impact on social and emotional well-being. Social activities, like dining out or attending events, may be affected due to concerns about accidents or the need to find a restroom frequently. This can lead to feelings of anxiety, embarrassment, and social isolation. Addressing these feelings with open communication and support systems is essential for maintaining a positive self-image and social life.
Strategies for Communicating with Healthcare Providers About OAB
Open and honest communication with healthcare providers is vital in managing OAB. Men should clearly articulate their symptoms, including frequency, urgency, and any associated discomfort. They should also share their concerns about the impact of OAB on their daily lives and discuss any existing health conditions that might be contributing factors. A detailed medical history and open dialogue can help healthcare providers develop a personalized treatment plan.
Importance of Maintaining a Healthy Lifestyle to Reduce OAB Symptoms
Maintaining a healthy lifestyle plays a critical role in managing OAB. A balanced diet, rich in fruits, vegetables, and whole grains, can contribute to overall health and potentially reduce bladder irritability. Regular exercise, including cardiovascular activity and strength training, strengthens the pelvic floor muscles and improves circulation. Limiting caffeine and alcohol consumption, known bladder irritants, can also be beneficial.
Furthermore, stress management techniques like yoga, meditation, or mindfulness exercises can help reduce anxiety and improve bladder control.
Prevention and Prognosis
Overactive bladder (OAB) in men, while often manageable, can significantly impact quality of life. Understanding preventive measures and the potential long-term effects is crucial for proactive health management. Prognosis, too, is influenced by factors like the severity of the condition and the individual’s response to treatment.Effective prevention and a favorable prognosis hinge on early detection and appropriate management strategies.
This section will Artikel key preventive steps, explore potential long-term effects, and detail how the prognosis varies depending on the severity of OAB and timely intervention.
Preventive Measures for OAB
Maintaining a healthy lifestyle plays a pivotal role in reducing the risk of OAB. A balanced diet, regular exercise, and sufficient hydration are key components. Limiting caffeine and alcohol intake can also help to minimize bladder irritation. Addressing underlying medical conditions, such as diabetes or prostate issues, is equally important in preventing OAB.
- Dietary Adjustments: A diet rich in fruits, vegetables, and whole grains promotes overall health, potentially lessening the likelihood of OAB development. Reducing intake of highly processed foods, sugary drinks, and excessive caffeine can also be beneficial.
- Regular Exercise: Physical activity strengthens pelvic floor muscles, which support bladder function. Even moderate-intensity exercises like brisk walking or swimming can be helpful.
- Hydration: Drinking sufficient water is important for overall health and can help maintain bladder health. However, excessive fluid intake right before bed may increase the frequency of urination.
- Avoiding Irritants: Certain foods and beverages, such as alcohol and caffeine, can irritate the bladder. Reducing consumption of these substances can help prevent OAB symptoms.
- Managing Underlying Conditions: Conditions like diabetes and prostate issues can contribute to OAB. Managing these conditions through appropriate medical care can help mitigate the risk of OAB.
Long-Term Effects of OAB
Untreated or inadequately managed OAB can lead to several potential long-term consequences. These can range from social isolation due to frequent bathroom needs to decreased mobility and a lower quality of life. In some cases, OAB can impact personal relationships and employment opportunities.
Prognosis Based on Severity and Treatment
The prognosis for OAB in men is largely influenced by the severity of the condition and the effectiveness of treatment. Mild cases often respond well to lifestyle modifications and conservative therapies. Moderate to severe cases might necessitate more intensive treatment strategies, such as medications or surgery. Early diagnosis and prompt treatment are crucial for achieving positive outcomes.
- Mild OAB: Individuals with mild OAB often experience a favorable prognosis. Lifestyle changes, such as dietary modifications and regular exercise, can effectively manage symptoms, resulting in a good quality of life.
- Moderate OAB: Moderate OAB may require a combination of therapies, including medication and lifestyle adjustments, for optimal management. The prognosis remains positive with consistent treatment and adherence to the prescribed regimen.
- Severe OAB: Severe cases of OAB may necessitate more intensive interventions, including surgical procedures. The prognosis in these cases is generally favorable, but the recovery period might be longer, and the potential for recurrence should be considered.
Importance of Early Diagnosis and Treatment
Early diagnosis and treatment of OAB are essential for preventing the progression of symptoms and maintaining a good quality of life. Prompt intervention can also help prevent potential complications and associated long-term effects.
Factors Affecting Prognosis of OAB
| Factor | Description |
|---|---|
| Severity of OAB | Mild cases generally have a better prognosis compared to moderate or severe cases. |
| Underlying Conditions | Co-existing medical conditions, such as diabetes or prostate issues, can impact the severity and treatment response of OAB. |
| Treatment Adherence | Consistent adherence to prescribed treatment plans is vital for achieving positive outcomes. |
| Individual Response to Therapy | Individual responses to medications and therapies can vary, influencing the effectiveness of treatment. |
| Age | Age can influence the severity of symptoms and response to treatment. |
Illustrative Cases and Examples
Understanding overactive bladder (OAB) in men often benefits from concrete examples. Real-life scenarios help illustrate the range of symptoms, diagnostic processes, and treatment approaches that can be effective. These case studies and hypothetical situations offer valuable insights into managing OAB.
A Case Study of OAB Diagnosis and Treatment
John, a 65-year-old man, started experiencing frequent and urgent urination, especially at night. He also reported a sensation of incomplete bladder emptying. His doctor conducted a thorough medical history and physical examination, including a urine test to rule out infection. Further evaluation with urodynamic studies confirmed OAB. The treatment plan for John included lifestyle modifications, such as fluid management and timed voiding schedules.
Dealing with an overactive bladder can be a real pain, guys. It’s frustrating, and it can really impact your daily life. Interestingly, a recent study suggests that a high protein, high-fat breakfast might play a role in bettering overall health, potentially even helping with blood sugar control. This could be a game-changer for men experiencing issues with overactive bladder, as managing blood sugar levels is crucial for overall health, including reducing the risk of some health conditions.
You can check out more on how a high protein fat breakfast can reduce A1C here: high protein fat breakfast can reduce a1c. While more research is needed to directly link these two, it’s certainly worth exploring these potential health benefits in tandem with a doctor’s guidance. So, stay tuned for more tips on managing overactive bladder!
He was also prescribed an antimuscarinic medication, which effectively reduced his symptoms and improved his quality of life.
A Hypothetical Scenario of OAB Symptoms and Steps
Imagine Mark, a 40-year-old businessman, noticing increased urinary frequency and urgency. He initially attributed these symptoms to stress and caffeine intake. However, the symptoms persisted and interfered with his work and social life. He consulted his doctor, who performed a physical examination and ordered some basic tests. These tests ruled out infections and other medical conditions.
Dealing with an overactive bladder can be a real pain, guys. It’s frustrating, and sometimes the discomfort can be intense. It’s not just about frequent trips to the bathroom; it can impact your quality of life significantly. Sometimes, similar to the debilitating pain associated with a slap tear of the shoulder slap tear of the shoulder , the underlying issue can be a bit more complex than you might think.
While it’s not directly related, it’s important to remember that other health concerns can often play a role in this bladder issue. So, if you’re struggling, remember to talk to your doctor.
The doctor then discussed lifestyle changes, medication options, and possible surgical interventions. Mark chose to begin with lifestyle adjustments and medication, which provided significant relief.
A Case Study of Successful OAB Management
Sarah, a nurse practitioner, helped a patient, a 72-year-old retired teacher named Mr. Davis, manage his OAB. Mr. Davis had experienced OAB symptoms for several years, impacting his independence. Sarah guided him through bladder training exercises, and he started a timed voiding schedule.
She also educated him on the importance of fluid intake management and caffeine restriction. Combining these non-pharmacological strategies with a low-dose antimuscarinic medication resulted in significant improvement in Mr. Davis’s quality of life and reduced his dependence on incontinence products.
A Real-Life Example of Lifestyle Changes Improving OAB Symptoms
A 55-year-old accountant named David noticed a significant improvement in his OAB symptoms after implementing lifestyle changes. He reduced his caffeine intake and increased his fluid intake throughout the day instead of just before bedtime. He also started incorporating regular exercise into his routine. These changes significantly reduced the frequency and urgency of his urination.
Table of Real-Life Scenarios Demonstrating Successful OAB Management in Men
| Scenario | Patient Profile | Management Strategy | Outcome |
|---|---|---|---|
| 1 | 68-year-old man with benign prostatic hyperplasia (BPH) | Combination of medication for BPH and bladder training exercises | Significant reduction in urinary frequency and urgency. |
| 2 | 42-year-old man with a history of prostate surgery | Lifestyle modifications (fluid management, timed voiding), and medication. | Improved symptom control and reduced reliance on incontinence products. |
| 3 | 58-year-old man with diabetes | Blood sugar management, lifestyle modifications (fluid management, timed voiding), and medication. | Improved symptom control, and reduced need for medication. |
| 4 | 70-year-old man with a history of stroke | Physiotherapy for improved pelvic floor muscles, lifestyle modifications (fluid management, timed voiding), and medication. | Improved urinary control and reduced risk of falls. |
Additional Resources and Support: Overactive Bladder In Men
Navigating the complexities of overactive bladder (OAB) can be challenging, but you’re not alone. This section provides valuable resources to help men better understand and manage their OAB, empowering them with knowledge and support networks.
Reliable Resources for Men with OAB, Overactive bladder in men
Understanding OAB involves accessing credible information. Numerous organizations and websites offer valuable insights into the condition, treatment options, and management strategies. Reputable sources provide accurate information and support for men facing OAB.
- The National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK): This government agency offers comprehensive information on various health conditions, including OAB, with evidence-based research and detailed explanations.
- The American Urological Association (AUA): A professional organization dedicated to advancing urological care, the AUA provides information for both patients and healthcare providers. This resource can help you understand the latest research and treatment approaches for OAB.
- Urology Care Foundation: This foundation focuses on providing reliable information about urological health. Their website often features articles, FAQs, and details about treatments and preventative measures.
Support Groups for Men with OAB
Finding a support system is crucial for managing OAB. Connecting with others facing similar challenges can offer emotional support, shared experiences, and practical advice. Online forums and support groups can provide a safe space for men to connect and share their journeys.
- Online Forums and Communities: Many online communities cater to men with various health conditions, including OAB. These platforms often provide a space for discussions, questions, and sharing experiences.
- Local Support Groups: Check with local hospitals, clinics, and urology practices for possible support groups or workshops. These groups can offer in-person connections and opportunities to ask questions and share experiences with others facing similar challenges.
Seeking Professional Medical Advice
Professional medical advice is essential for accurate diagnosis and effective treatment. Consulting with a qualified urologist is the first step in managing OAB.
- Finding a Qualified Urologist: When searching for a urologist, consider their experience in treating overactive bladder. Look for specialists with advanced training and a proven track record in OAB management. A urologist’s website or online directory may provide details on their expertise.
Patient Advocacy and Community Engagement
Engaging with patient advocacy groups can amplify your voice and help create positive change in the medical community. Supporting these organizations can bring about greater awareness and improved care for men with OAB.
- Patient Advocacy Organizations: Research and connect with organizations dedicated to supporting patients with OAB or related urological conditions. Their work often includes advocacy for improved research, better treatment options, and increased public awareness of the condition.
Last Point
In conclusion, overactive bladder in men is a multifaceted issue requiring a comprehensive understanding of its causes, symptoms, and treatment options. By exploring the available resources and strategies, men can take proactive steps toward managing their symptoms and improving their overall well-being. Remember, seeking professional medical advice is crucial for accurate diagnosis and personalized treatment plans. This discussion has highlighted the importance of open communication and proactive engagement in managing this condition.










