Rheumatoid arthritis effects on body systems are multifaceted and profound. This exploration delves into the intricate ways RA affects various bodily systems, from the musculoskeletal framework to the delicate balance of the endocrine system. We’ll examine how chronic inflammation, a defining characteristic of RA, triggers a cascade of effects, impacting not only physical function but also mental well-being.
Understanding these impacts is crucial for patients and healthcare providers alike.
The inflammatory nature of rheumatoid arthritis (RA) causes significant damage throughout the body. This detailed look at RA will explore the specific mechanisms by which RA attacks different systems. From the joints to the lungs, the cardiovascular system, and the nervous system, we will see how RA can manifest as pain, stiffness, inflammation, and functional limitations. We will also look at the important role of the immune system in this autoimmune disease and the impact of RA on the patient’s mental health.
Introduction to Rheumatoid Arthritis
Rheumatoid arthritis (RA) is a chronic autoimmune disease that primarily affects the joints. Unlike other joint conditions, RA is characterized by a persistent inflammatory response that can lead to significant joint damage over time. This inflammation isn’t just localized to the affected area; it often has systemic effects, impacting various organs and tissues throughout the body.The hallmark of RA is the body’s immune system mistakenly attacking its own healthy tissues, specifically the lining of the joints.
This attack triggers inflammation, causing pain, swelling, stiffness, and ultimately, potentially destructive changes in the joint structure. Understanding the complex interplay of the immune system in RA is crucial for developing effective treatments and managing the condition.
Key Characteristics and Symptoms of Rheumatoid Arthritis
RA manifests with a range of symptoms, often varying in severity and duration from person to person. Common characteristics include persistent joint pain, swelling, and stiffness, especially in the morning. These symptoms typically affect multiple joints simultaneously, symmetrically (meaning both sides of the body are affected). Fatigue, fever, and loss of appetite can also be present. The intensity and duration of these symptoms can fluctuate, and some individuals experience periods of remission, where symptoms subside or disappear.
Typical Progression of Rheumatoid Arthritis
The progression of RA is not uniform; it varies significantly among individuals. Early diagnosis and intervention are crucial in managing the condition’s progression. Some individuals may experience a slow, gradual progression of symptoms, while others may experience more rapid and severe joint damage. The rate of progression is influenced by factors like the severity of the initial inflammatory response, the individual’s overall health, and adherence to treatment plans.
Immune System’s Role in Rheumatoid Arthritis
The immune system’s primary function is to defend the body against foreign invaders like bacteria and viruses. In RA, the immune system malfunctions, mistaking healthy tissues as foreign threats. This misguided attack is initiated by a complex interplay of immune cells, including T cells and B cells, and the production of autoantibodies, such as rheumatoid factor (RF) and anti-citrullinated protein antibodies (ACPA).
These autoantibodies target the synovial lining of the joints, triggering an inflammatory cascade that damages cartilage and bone. The body’s own immune response, intended to protect, becomes the primary source of destruction in RA.
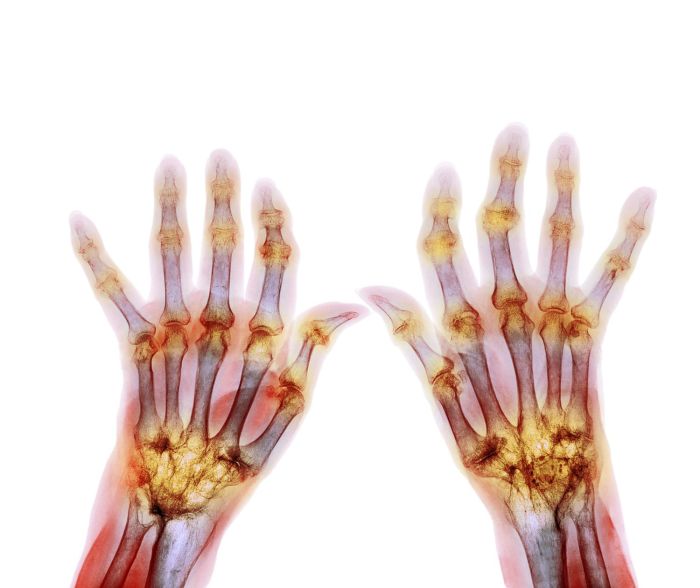
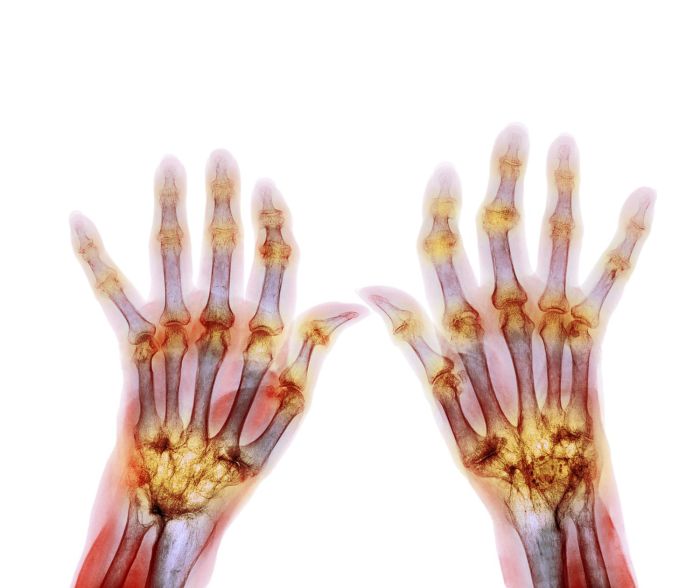
Effects on the Musculoskeletal System
Rheumatoid arthritis (RA) primarily targets the musculoskeletal system, causing significant damage and impacting daily life. The chronic inflammatory process within the joints leads to a cascade of events that progressively erode joint structures, resulting in pain, stiffness, and potentially debilitating deformities. Understanding these effects is crucial for effective management and treatment.Rheumatoid arthritis’s destructive action on the joints begins with inflammation.
This inflammation triggers the release of enzymes that break down cartilage and bone, ultimately leading to joint damage. The process is often asymmetrical, meaning one joint may be affected more severely than another.
Joint Damage Mechanisms
The inflammatory response in RA is characterized by an overactive immune system attacking the lining of the joints, known as the synovium. This attack triggers a cascade of inflammatory mediators, including cytokines and enzymes, that damage the joint’s cartilage, bone, and surrounding tissues. Cartilage, the smooth tissue that cushions the ends of bones, is gradually eroded, leading to pain and reduced joint mobility.
The underlying bone tissue is also affected, becoming thinned and eventually losing its structural integrity. These structural changes lead to the characteristic symptoms of RA.
Structural Changes in Affected Joints
The synovium, the inner lining of the joint capsule, becomes thickened and inflamed in RA. This thickened synovium forms a pannus, a tissue that invades the cartilage and bone. This pannus tissue releases enzymes that degrade cartilage and bone, creating a vicious cycle of destruction. The loss of cartilage results in bone-on-bone contact, further exacerbating pain and inflammation.
Joint spaces narrow, and the bone may fuse together, a condition known as ankylosis.
Development of Joint Inflammation, Pain, and Stiffness
Inflammation within the joint space is the primary cause of pain and stiffness. The release of inflammatory mediators causes swelling, heat, and redness in the affected area. The pain is often described as a deep, aching sensation, which can worsen with activity and improve with rest. Morning stiffness, lasting for more than an hour, is a common complaint in RA.
This stiffness is due to the accumulation of inflammatory fluid and the thickening of the synovium.
Potential for Joint Deformities
The progressive destruction of joint structures can lead to significant deformities. Over time, the joint’s normal alignment can be disrupted, leading to a loss of function and an altered gait. Common deformities include ulnar deviation of the wrist, boutonnière deformity of the fingers, and swan-neck deformity. These deformities, often visible and noticeable, can significantly impact a person’s ability to perform daily tasks.
Comparison of Effects on Different Joint Types
| Joint Type | Specific Effects |
|---|---|
| Wrists | Ulnar deviation, carpal tunnel syndrome, limited range of motion |
| Knees | Pain, swelling, instability, limited range of motion, potential for effusion (fluid buildup) |
| Ankles | Pain, swelling, stiffness, limited mobility, potential for subluxation (partial dislocation) |
Common Symptoms in Various Joints
| Joint | Pain | Swelling | Reduced Mobility |
|---|---|---|---|
| Wrists | Aching, throbbing pain, especially in the morning | Swelling and tenderness in the wrist area | Difficulty with gripping, turning, or bending the wrist |
| Knees | Deep, aching pain, often worse with weight-bearing activities | Swelling, warmth, and redness around the knee joint | Limited ability to bend, straighten, or rotate the knee |
| Ankles | Sharp, throbbing pain, especially with movement | Swelling and tenderness in the ankle area | Difficulty with walking, running, or climbing stairs |
Effects on the Cardiovascular System
Rheumatoid arthritis (RA) is not just a disease of the joints; its impact extends to other vital organs, including the cardiovascular system. This chronic inflammatory condition carries a significantly increased risk of cardiovascular diseases (CVD), a leading cause of death in RA patients. Understanding the mechanisms linking RA to CVD is crucial for developing effective preventative strategies and improving patient outcomes.
Increased Risk of Cardiovascular Diseases
Rheumatoid arthritis patients have a higher risk of developing cardiovascular diseases, including heart disease, stroke, and peripheral artery disease, compared to the general population. This increased risk is not fully understood, but likely stems from a complex interplay of factors related to chronic inflammation and the disease itself. The presence of persistent inflammation throughout the body contributes to a pro-thrombotic state, increasing the risk of blood clots and promoting atherosclerosis.
Mechanisms Linking RA to Cardiovascular Problems
Several mechanisms link rheumatoid arthritis to cardiovascular problems. Chronic inflammation, a hallmark of RA, damages blood vessels and promotes the formation of plaque in the arteries. This inflammation also leads to an increased production of inflammatory markers, such as C-reactive protein (CRP), which are linked to an increased risk of CVD. The chronic activation of the immune system in RA patients also contributes to the development of atherosclerosis, a condition where plaque builds up in the arteries, narrowing them and reducing blood flow.
This, in turn, raises blood pressure and increases the risk of heart attack or stroke.
Potential for Inflammation to Affect Blood Vessels and the Heart
The inflammatory process in RA can directly affect the blood vessels and the heart. Inflammation can damage the inner lining of the arteries (endothelium), which is crucial for maintaining healthy blood flow. This damage allows for the accumulation of cholesterol and other substances, leading to the formation of plaques. Over time, these plaques can harden and narrow the arteries, reducing blood flow to the heart and other organs.
The inflammation can also directly affect the heart muscle itself, leading to conditions like pericarditis (inflammation of the sac surrounding the heart) or myocarditis (inflammation of the heart muscle).
Impact of Long-Term Inflammation on Blood Pressure and Cholesterol Levels
Long-term inflammation associated with RA can significantly impact blood pressure and cholesterol levels. Elevated inflammatory markers, like CRP, are linked to higher blood pressure readings. This chronic inflammatory state can also impair the body’s ability to regulate cholesterol levels, leading to higher levels of low-density lipoprotein (LDL) cholesterol, often referred to as “bad” cholesterol. High LDL cholesterol contributes to the buildup of plaque in the arteries.
Influence of RA Medications on Cardiovascular Health, Rheumatoid arthritis effects on body systems
Some medications used to treat rheumatoid arthritis can have both beneficial and detrimental effects on cardiovascular health. While disease-modifying antirheumatic drugs (DMARDs) effectively control the inflammation associated with RA, some studies have shown a potential link between certain DMARDs and an increased risk of cardiovascular events, such as heart attack or stroke. It is crucial to carefully monitor patients on these medications for signs of cardiovascular problems and adjust treatment strategies accordingly.
The long-term effects of these medications on cardiovascular health are still under investigation.
Risk Factors Comparison
| Risk Factor | Rheumatoid Arthritis Patients | Healthy Individuals |
|---|---|---|
| Chronic Inflammation | High | Low |
| Elevated Inflammatory Markers (e.g., CRP) | High | Low |
| Smoking | Potentially Higher (often comorbid) | Variable |
| Obesity | Potentially Higher (often comorbid) | Variable |
| Hypertension (High Blood Pressure) | Potentially Higher (often comorbid) | Variable |
| Hyperlipidemia (High Cholesterol) | Potentially Higher (often comorbid) | Variable |
| Family History of CVD | Potentially Higher (often comorbid) | Variable |
Note: Comorbidity implies that other conditions often exist alongside RA. The table above highlights potential differences in risk factors, but individual experiences can vary significantly.
Effects on the Respiratory System

Rheumatoid arthritis (RA) isn’t just a disease of the joints; it can impact various body systems, including the respiratory system. Understanding how RA affects the lungs is crucial for comprehensive patient care. While joint pain and stiffness are prominent features, respiratory complications can significantly reduce quality of life and, in some cases, lead to serious health concerns.RA’s inflammatory processes can extend beyond the musculoskeletal system, potentially causing damage to the lungs and airways.
This inflammation can manifest in various ways, impacting lung function and leading to breathing difficulties. The underlying mechanisms connecting RA to respiratory issues are complex and not fully understood, but research suggests a link between the body’s immune response and lung inflammation.
Potential for Lung Involvement
RA can affect the lungs through various pathways, including inflammation and immune system dysfunction. This can lead to a range of respiratory issues, from mild discomfort to serious conditions. A key concern is the development of interstitial lung disease (ILD).
Interstitial Lung Disease (ILD) in RA
Interstitial lung disease is a condition characterized by scarring and inflammation in the interstitial tissues of the lungs. In RA patients, this inflammation can be triggered by the same autoimmune processes that cause joint damage. The presence of RA can increase the risk of developing ILD, with some studies showing a correlation between the severity of RA and the likelihood of developing ILD.
Individuals with RA should be regularly monitored for signs of lung involvement. Symptoms often appear gradually, making early detection challenging. This highlights the importance of routine check-ups and reporting any unusual respiratory symptoms to healthcare providers.
Impact of Inflammation on Airways and Lungs
Inflammation, a hallmark of RA, can directly affect the airways and lungs. This inflammatory response can lead to narrowing of the airways, making breathing more difficult. Furthermore, inflammation can cause fluid buildup in the lungs, hindering oxygen exchange and leading to shortness of breath. The inflammatory process can also cause scarring, further compromising lung function.
Shortness of Breath and Coughing
Shortness of breath and coughing are common respiratory symptoms experienced by some RA patients. These symptoms can stem from the inflammatory processes described above, directly affecting the lungs’ ability to function optimally. Shortness of breath, often described as difficulty catching one’s breath, can range from mild to severe, impacting daily activities. Coughing, often dry or productive, can be a persistent symptom, adding to the patient’s discomfort.
Comparison of Respiratory Symptoms
| Symptom | Rheumatoid Arthritis | Asthma | Chronic Obstructive Pulmonary Disease (COPD) |
|---|---|---|---|
| Shortness of Breath | Progressive, often worse with exertion, associated with inflammation | Triggered by allergens or irritants, typically episodic | Progressive, often worse with exertion, associated with airflow obstruction |
| Cough | Dry or productive, can be persistent, often related to inflammation | Dry or productive, often triggered by allergens or irritants | Productive, often with mucus, associated with airway obstruction |
| Chest Pain | Possible, associated with inflammation | Less common | Possible, associated with airway obstruction and/or infections |
| Wheezing | Less common, can be present in some cases | Characteristic symptom | Less common, can be present in some cases |
This table provides a general comparison. Individual experiences and presentations can vary. It is crucial to consult with a healthcare professional for accurate diagnosis and treatment.
Effects on the Neurological System
Rheumatoid arthritis (RA) isn’t just a disease of the joints; it can also impact the delicate workings of the nervous system. While less common than musculoskeletal or cardiovascular complications, neurological involvement can significantly affect a person’s quality of life. Understanding the potential pathways of nerve damage and the resulting symptoms is crucial for effective management and early intervention.
Potential Neurological Complications
RA can lead to a range of neurological complications, varying in severity. These complications aren’t always directly caused by RA itself, but can arise from the immune system’s overactive response or other factors associated with the disease. One significant concern is the potential for nerve damage, which can manifest as peripheral neuropathy.
Link Between Rheumatoid Arthritis and Nerve Damage
The inflammatory processes associated with RA can directly affect the nerves. The immune system’s attack on the joints can extend to the surrounding tissues, including nerves. This inflammation can cause compression, demyelination, or direct damage to the nerves, leading to a spectrum of symptoms. Additionally, certain medications used to treat RA can also have neurotoxic effects.
Peripheral Neuropathy and Other Neurological Disorders
Peripheral neuropathy, characterized by numbness, tingling, pain, and weakness in the extremities, is a common neurological manifestation of RA. Other potential neurological disorders include mononeuritis multiplex, a condition involving the inflammation of multiple peripheral nerves, and even, though less frequently, cerebrovascular accidents (strokes). It’s important to note that these conditions aren’t exclusive to RA; they can occur in various other diseases.
Mechanisms of Nerve Involvement in Rheumatoid Arthritis
Several mechanisms contribute to nerve involvement in RA. Inflammation can directly compress nerves, reducing blood flow and potentially causing damage. Antibodies produced during the immune response can also attack nerve tissues, leading to demyelination, a crucial process for nerve conduction. Vasculitis, inflammation of the blood vessels, can impair blood supply to nerves, further exacerbating the issue. The exact interplay of these mechanisms varies from person to person.
Neurological Symptoms Associated with Rheumatoid Arthritis
| Symptom | Description |
|---|---|
| Numbness | A loss of sensation in the affected area. |
| Tingling | A prickling or itching sensation. |
| Pain | A range of discomfort, from mild to severe. |
| Weakness | A diminished ability to move or use the affected area. |
| Muscle cramps | Involuntary contractions of muscles. |
| Loss of reflexes | A decrease or absence of the body’s involuntary responses. |
| Cognitive impairment | Difficulties with memory, concentration, or other mental functions. |
This table provides a concise overview of common neurological symptoms. It’s crucial to remember that these symptoms can vary significantly in their presentation and severity. A thorough medical evaluation is essential to accurately diagnose and manage any neurological complications.
Effects on the Gastrointestinal System
Rheumatoid arthritis (RA) isn’t just a disease of the joints; its inflammatory processes can extend to other body systems, including the gastrointestinal tract. This often manifests in various digestive issues, impacting the quality of life for those living with RA. Understanding these effects is crucial for comprehensive RA management.The inflammatory cascade characteristic of RA can directly or indirectly affect the gastrointestinal system.
This inflammation can trigger a range of symptoms, from mild discomfort to more severe complications. The link between RA and gastrointestinal issues isn’t fully understood, but it’s thought that shared immune system mechanisms may play a role.
Potential for Digestive System Impact
The inflammatory response triggered by RA can affect the lining of the digestive tract, leading to various issues. This inflammation can disrupt the normal functioning of the digestive system, leading to discomfort and potentially more severe complications. Inflammation can cause the digestive tract to become more sensitive to certain foods and triggers, potentially leading to food intolerances or digestive distress.
Impact of Medications on the Digestive Tract
Many medications used to treat RA can also have significant side effects on the digestive system. These medications, while effective in managing RA symptoms, can sometimes disrupt the delicate balance of the gut microbiome and lead to a variety of digestive issues. It’s crucial for patients to be aware of these potential side effects and discuss them with their healthcare providers.
Gastrointestinal Side Effects of RA Medications
| Medication Category | Potential Gastrointestinal Side Effects |
|---|---|
| Nonsteroidal anti-inflammatory drugs (NSAIDs) | Nausea, heartburn, abdominal pain, indigestion, ulcers, bleeding |
| Disease-modifying antirheumatic drugs (DMARDs) | Nausea, vomiting, diarrhea, abdominal pain, constipation, loss of appetite |
| Biologics | Nausea, diarrhea, abdominal pain, vomiting, abdominal cramps, gastritis, and pancreatitis |
Note: This table is not exhaustive, and individual experiences may vary. Always consult with a healthcare professional for personalized guidance.
Effects on the Endocrine System
Rheumatoid arthritis (RA) isn’t just a disease of the joints; its inflammatory nature can have far-reaching effects on various bodily systems, including the endocrine system. This intricate network of glands and hormones plays a crucial role in regulating numerous functions, and RA can disrupt this delicate balance. Understanding the potential interactions between RA and the endocrine system is important for comprehensive patient care.The inflammatory processes characteristic of RA can influence hormone production and function, potentially leading to a range of endocrine complications.
The chronic inflammation associated with RA can create a complex interplay with the endocrine system, making it challenging to pinpoint precise causal relationships.
Potential Endocrine Effects in RA
RA’s impact on the endocrine system isn’t fully understood, but research suggests several potential links. The chronic inflammation can affect the production and regulation of hormones, leading to a range of possible outcomes. The immune system’s response in RA can indirectly affect hormone production in glands like the thyroid and adrenal glands.
Rheumatoid arthritis can affect various body systems, impacting everything from joints to lungs. While managing this condition often involves medication and physical therapy, sometimes a little self-care can help. For instance, if you experience chest congestion, exploring home remedies like herbal teas and steam inhalation can be beneficial. For more ideas, check out these simple home remedies for chest congestion here.
Ultimately, remember that rheumatoid arthritis symptoms vary greatly from person to person, so consulting with a doctor is crucial for proper diagnosis and treatment.
Impact of Inflammation on Hormone Production
The chronic inflammation in RA can disrupt the delicate balance of hormone production. Inflammation triggers the release of cytokines, signaling molecules that play a crucial role in the immune response. These cytokines can potentially interfere with the normal functioning of endocrine glands, affecting hormone synthesis and release. This disruption can lead to various symptoms and conditions. For example, the inflammatory processes can lead to an increase in cortisol levels, which can further impact other hormones and metabolic processes.
Medication Influence on the Endocrine System
Many medications used to treat RA can also have an impact on the endocrine system. Corticosteroids, often prescribed to reduce inflammation, can directly influence hormone levels, potentially leading to side effects such as Cushing’s syndrome. Other disease-modifying antirheumatic drugs (DMARDs) can also interact with the endocrine system, though the mechanisms are often less direct and more complex.
Rheumatoid arthritis can affect various body systems, impacting everything from joints to organs. One common symptom is experiencing rapid heartbeats, which can be concerning. If you’re wondering why your heart is racing, it’s always a good idea to check out resources like this page on why is my heart beating so fast. While this is a possible symptom, it’s crucial to remember that persistent rapid heartbeats could stem from other issues, and a doctor’s evaluation is always recommended to ensure proper diagnosis and treatment, especially if related to rheumatoid arthritis complications.
Comparison of Endocrine Effects in RA Patients and Healthy Individuals
| Characteristic | Rheumatoid Arthritis Patients | Healthy Individuals |
|---|---|---|
| Cortisol Levels | Potentially elevated due to chronic inflammation. May be influenced by corticosteroid use. | Maintain a relatively stable and balanced cortisol level. |
| Thyroid Function | Increased risk of thyroid dysfunction (hypothyroidism or hyperthyroidism). This is often subtle and requires specific testing. | Maintain stable thyroid function. |
| Glucose Metabolism | Increased risk of insulin resistance and impaired glucose tolerance, potentially leading to diabetes. | Maintain stable glucose metabolism. |
| Growth Hormone | Potentially affected, but more research is needed to fully understand the implications. | Maintain normal growth hormone levels. |
| Reproductive Hormones | Potential impact on reproductive hormones, though this is less well understood. | Maintain normal reproductive hormone levels. |
Effects on the Immune System
Rheumatoid arthritis (RA) isn’t just a disease of the joints; it’s a systemic autoimmune disorder that profoundly impacts the entire body, particularly the immune system. The immune system, designed to protect the body from invaders, malfunctions in RA, turning against the body’s own tissues. This leads to chronic inflammation, causing pain, stiffness, and damage to various organs.The immune system’s dysfunction is central to the development and progression of rheumatoid arthritis.
Rheumatoid arthritis can affect various body systems, impacting everything from joints to overall well-being. One surprising symptom is persistent coldness, often linked to inflammation and reduced blood flow. This can sometimes be mistaken for other issues, like a general feeling of being cold, but understanding the root cause is key. If you’re frequently chilly, exploring the reasons behind it, such as in why do you feel cold all the time , can help pinpoint if there’s an underlying condition affecting your body’s temperature regulation.
Ultimately, understanding how RA affects your body’s systems is crucial for managing your health effectively.
The intricate interplay of immune cells and the inflammatory response plays a crucial role in the disease process. Understanding this process is vital for developing effective therapies.
Autoimmune Mechanisms in RA
RA is characterized by an aberrant immune response, where the body’s immune system mistakenly identifies healthy tissues as foreign invaders. This misidentification triggers an inflammatory cascade that attacks the joints and other tissues. The process begins with the activation of immune cells, primarily T cells and B cells, that are inappropriately directed against the body’s own tissues. A key feature of this immune response is the production of autoantibodies, specifically rheumatoid factor (RF) and anti-citrullinated protein antibodies (ACPAs).
These autoantibodies bind to specific proteins within the body, forming immune complexes that further contribute to the inflammatory response.
Impact of Long-Term Inflammation on Immune Response
Chronic inflammation, a hallmark of RA, has a detrimental effect on the overall immune response. The persistent inflammatory environment disrupts the delicate balance of the immune system. This disruption can lead to a weakening of the immune system’s ability to fight off infections, increasing the susceptibility to other diseases. Furthermore, the continuous activation of immune cells can lead to the depletion of certain immune cell populations, such as T regulatory cells, which normally suppress inflammation.
The result is a heightened and uncontrolled inflammatory response, causing widespread damage.
Effect on Antibody and Immune Cell Production
The production of antibodies and immune cells is significantly affected in RA. The overproduction of autoantibodies, like RF and ACPAs, is a defining characteristic of the disease. This overproduction contributes to the formation of immune complexes that deposit in tissues, leading to inflammation and tissue damage. Furthermore, the chronic inflammation in RA can lead to the dysregulation of immune cell development and function.
This disruption in the balance between pro-inflammatory and anti-inflammatory immune responses is a key factor in the disease’s progression.
Diagram: Immune System and RA
[Diagram description: A circular diagram illustrating the complex interplay between the immune system and rheumatoid arthritis. The center of the circle represents the joint, with red arrows representing the activation of immune cells (e.g., T cells, B cells) that initiate an inflammatory response. The inflammatory response (depicted by a spreading red cloud) leads to the production of autoantibodies (RF, ACPAs), shown as yellow arrows targeting joint tissues.
The diagram further shows how the chronic inflammation weakens the immune system, indicated by a decreased size of immune cell populations (T regulatory cells). The diagram also shows the connection to other body systems, such as the cardiovascular and musculoskeletal systems, which are also affected by the chronic inflammation.]
Effects on Mental Health
Living with rheumatoid arthritis (RA) can significantly impact mental well-being. The chronic pain, fatigue, and unpredictable nature of the disease can lead to feelings of isolation, anxiety, and depression. Understanding the psychological toll of RA is crucial for effective management and support.The chronic inflammation and pain associated with RA can trigger a cascade of negative psychological effects. This often results in a diminished quality of life and a reduced ability to participate in activities that were once enjoyable.
The physical limitations imposed by the disease can also contribute to feelings of frustration and helplessness.
Psychological Impact of Rheumatoid Arthritis
The chronic pain and fatigue associated with RA can lead to significant psychological distress. Individuals with RA often experience feelings of hopelessness, helplessness, and isolation due to the unpredictable nature of the disease. This can further exacerbate existing mental health concerns or contribute to the development of new ones. Difficulties with daily tasks, reduced mobility, and social isolation can contribute to a negative self-image and a sense of decreased self-worth.
This often leads to emotional distress, anxiety, and depressive symptoms.
Link Between Rheumatoid Arthritis and Mental Health Conditions
A strong correlation exists between RA and mental health conditions like anxiety and depression. Studies have shown that individuals with RA are at an increased risk of developing these conditions compared to the general population. The chronic nature of RA, coupled with its physical and emotional toll, can significantly impact mental well-being. Factors such as pain, fatigue, and limited mobility can contribute to feelings of stress, hopelessness, and isolation, increasing the vulnerability to mental health issues.
Impact of Chronic Pain and Disability on Mental Well-being
Chronic pain and disability, common features of RA, have a profound impact on mental well-being. The constant pain and limitations in physical function can lead to feelings of frustration, anger, and irritability. The unpredictable nature of RA exacerbates these feelings, as individuals may experience periods of significant flare-ups followed by periods of relative remission. This unpredictability can be mentally taxing, causing anxiety and impacting daily routines.
Reduced mobility and difficulty with daily tasks can further contribute to feelings of isolation and decreased self-esteem.
Importance of Mental Health Support for Rheumatoid Arthritis Patients
Acknowledging the importance of mental health support for RA patients is crucial. Adequate mental health support can significantly improve their quality of life. It allows patients to cope with the emotional and psychological challenges of living with RA, manage stress effectively, and maintain a sense of hope and resilience. Mental health professionals, such as psychologists and psychiatrists, can provide tailored support and strategies to help individuals navigate the emotional aspects of RA.
Support groups can also offer invaluable peer-to-peer connections and shared experiences.
Resources for Mental Health Support Specific to Rheumatoid Arthritis
Numerous resources provide mental health support tailored to the specific needs of RA patients.
- Support Groups: Support groups offer a safe and supportive environment for individuals with RA to connect with others who understand their experiences. Sharing stories and coping mechanisms can be empowering and foster a sense of community. These groups can provide practical advice, emotional support, and a sense of belonging.
- Mental Health Professionals: Mental health professionals, such as psychologists and psychiatrists, can provide evidence-based therapies and counseling to address specific mental health concerns related to RA. Therapies like cognitive behavioral therapy (CBT) can help individuals manage stress, anxiety, and depression associated with the disease.
- Patient Advocacy Organizations: Patient advocacy organizations often offer resources and support for RA patients, including information about mental health services and support groups. They can connect patients with relevant resources and promote understanding of the impact of RA on mental well-being.
Closing Notes: Rheumatoid Arthritis Effects On Body Systems
In conclusion, rheumatoid arthritis’s effects on the body systems are far-reaching and complex. The chronic inflammation characteristic of RA creates a domino effect, impacting various organs and functions. From joint destruction to cardiovascular risks and neurological complications, understanding these effects is vital for effective management and improved quality of life for individuals living with this condition. The discussion highlights the importance of comprehensive care, addressing not just the physical symptoms but also the mental and emotional aspects of living with RA.

Leave a Reply